Abstract
Epilepsy surgery is safe and effective treatment in children who fail to respond to antiepileptic medications. After failure of two appropriate antiepileptic medications, chances that the child will become seizure free with more or different medications is <5 %, and she should be diagnosed with “refractory epilepsy”. A consideration for surgical candidacy should be given to all children who fulfill the definition of refractory epilepsy. In appropriately selected children, epilepsy surgery offers a high chance of seizure freedom without incurring any new post-operative neurological deficits. No age is bar to epilepsy surgery. Even infants can safely have epilepsy surgery if they are surgical candidates. For most children, who are surgical candidates, a good history and physical examination, video EEG evaluation, and a high quality brain MRI are sufficient to make surgical decision. These tools are increasingly available all over the world. Better education of families, Pediatricians, Pediatric Neurologists and community care-givers is necessary to salvage children early from mortality and morbidity of untreated, sometimes life long, epilepsy.







Similar content being viewed by others
References
Gupta A. Special characteristics of surgically remediable epilepsy in infants. In: Luders H, editor. Textbook of epilepsy surgery. London: Informa Healthcare; 2008. p. 400–6.
Harvey AS, Cross JH, Shinnar S. Mathern GW; ILAE pediatric epilepsy surgery survey taskforce defining the spectrum of international practice in pediatric epilepsy surgery patients. Epilepsia. 2008;49:146–55.
Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med. 2000;342:314–9.
Duchowny M, Jayakar P, Resnick T, Harvey AS, Alvarez L, Dean P, et al. Epilepsy surgery in the first three years of life. Epilepsia. 1998;39:737–43.
Wyllie E, Comair YG, Kotagal P, Bulacio J, Bingaman W, Ruggieri P. Seizure outcome after epilepsy surgery in children and adolescents. Ann Neurol. 1998;44:740–8.
Moosa AN, Gupta A, Jehi L, Marashly A, Cosmo G, Lachhwani D, et al. Longitudinal seizure outcome and prognostic predictors after hemispherectomy in 170 children. Neurology. 2013;80:253–60.
Moseley BD. Excellent outcomes after extratemporal epilepsy surgery in children. Dev Med Child Neurol. 2012;54:968.
Huttenlocher PR, Hapke RJ. A follow-up study of intractable seizures in childhood. Ann Neurol. 1990;28:699–705.
Dikmen S, Matthews CG, Harley JP. Effect of early versus late onset of major motor epilepsy on cognitive-intellectual performance: further considerations. Epilepsia. 1977;18:31–6.
Loddenkemper T, Holland KD, Stanford LD, Kotagal P, Bingaman W, Wyllie E. Developmental outcome after epilepsy surgery in infancy. Pediatrics. 2007;119:930–5.
Moosa AN, Jehi L, Marashly A, Cosmo G, Lachhwani D, Wyllie E, et al. Long-term functional outcomes and their predictors after hemispherectomy in 115 children. Epilepsia. 2013;54:1771–9.
Asarnow RF, LoPresti C, Guthrie D, Elliott T, Cynn V, Shields WD, et al. Developmental outcomes in children receiving resection surgery for medically intractable infantile spasms. Dev Med Child Neurol. 1997;39:430–40.
Kossoff EH, Vining EP, Pillas DJ, Pyzik PL, Avellino AM, Carson BS, et al. Hemispherectomy for intractable unihemispheric epilepsy etiology vs outcome. Neurology. 2003;61:887–90.
Taha JM, Crone KR, Berger TS. The role of hemispherectomy in the treatment of holohemispherichemimegaloencephaly. J Neurosurg. 1994;81:37–42.
Maehara T, Shimizu H, Kawai K, Shigetomo R, Tamagawa K, Yamada T, et al. Postoperative development of children after hemispherotomy. Brain Dev. 2002;24:155–60.
Mizrahi EM, Kellaway P, Grossman RG, Rutecki PA, Armstrong D, Rettig G, et al. Anterior temporal lobectomy and medically refractory temporal lobe epilepsy of childhood. Epilepsia. 1990;31:302–12.
Camfield CS, Camfield PR, Veugelers PJ. Death in children with epilepsy: a population-based study. Lancet. 2002;359:1891–5.
Appleton RE. Mortality in paediatric epilepsy. Arch Dis Child. 2003;88:1091–4.
Callenbach PM, Westendorp RG, Geerts AT, Arts WF, Peeters EA, van Donselaar CA, et al. Mortality risk in children with epilepsy: the Dutch study of epilepsy in childhood. Pediatrics. 2001;107:1259–63.
Paolicchi JM, Jayakar P, Dean P, Yaylali I, Morrison G, Prats A, et al. Predictors of outcome in pediatric epilepsy surgery. Neurology. 2000;54:642–7.
Chugani HT, Shewmon DA, Peacock WJ, Shields WD, Mazziotta JC, Phelps ME. Surgical treatment of intractable neonatal-onset seizures: the role of positron emission tomography. Neurology. 1988;38:1178–88.
Kossoff EH, Vining EP, Pyzik PL, Kriegler S, Min KS, Carson BS, et al. The postoperative course and management of 106 hemidecortications. Pediatr Neurosurg. 2002;37:298–303.
Vining EP, Freeman JM, Pillas DJ, Uematsu S, Carson BS, Brandt J, et al. Why would you remove half a brain? The outcome of 58 children after hemispherectomy-the johns hopkins experience. Pediatrics. 1997;100:163–71.
Guldvog B, Loyning Y, Hauglie-Hanssen E, Flood S, Bjornaes H. Surgical treatment for partial epilepsy among Norwegian children and adolescents. Epilepsia. 1994;35:554–65.
Lim ME, Bowen JM, Snead 3rd OC, Elliott I, Donner E, Weiss SK, et al. Access to surgery for paediatric patients with medically refractory epilepsy: a systems analysis. Epilepsy Res. 2013;107:286–96.
Simasathien T, Vadera S, Najm I, Gupta A, Bingaman W, Jehi L. Improved outcomes with earlier surgery for intractable frontal lobe epilepsy. Ann Neurol. 2013;73:646–54.
Sadanand V. Economics of epilepsy surgery. Ann Indian Acad Neurol. 2014;17:S120–3.
Acharya JN, Wyllie E, Luders HO, Kotagal P, Lancman M, Coelho M. Seizure symptomatology in infants with localization-related epilepsy. Neurology. 1997;48:189–96.
Jr NDR, Bazil CW, Scheuer ML, Pedley TA. Recognition and classification of seizures in infants. Epilepsia. 1997;38:553–60.
Chugani HT, Shewmon DA, Shields WD, Sankar R, Comair Y, Vinters HV, et al. Surgery for intractable infantile spasms: neuroimaging perspectives. Epilepsia. 1993;34:764–71.
Asanuma H, Wakai S, Tanaka T, Chiba S. Brain tumors associated with infantile spasms. Pediatr Neurol. 1995;12:361–4.
Brockhaus A, Elger CE. Complex partial seizures of temporal lobe origin in children of different age groups. Epilepsia. 1995;36:1173–81.
Moseley BD, Nickels K, Wirrell EC. Surgical outcomes for intractable epilepsy in children with epileptic spasms. J Child Neurol. 2012;27:713–20.
Gowda S, Salazar F, Bingaman WE, Kotagal P, Lachhwani DL, Gupta A, et al. Surgery for catastrophic epilepsy in infants 6 months of age and younger. J Neurosurg Pediatr. 2010;5:603–7.
Gupta A, Wyllie E. Presurgical evaluation in children with catastrophic epilepsy. In: Luders H, Rosenow F, editors. Presurgical assessment of the epilepsies with clinical neurophysiology and functional imaging. Amsterdam: Elsevier; 2004. p. 451–9.
Gupta A, Chirla A, Wyllie E, Lachhwani DK, Kotagal P, Bingaman WE. Pediatric epilepsy surgery in focal lesions and generalized electroencephalogram abnormalities. Pediatr Neurol. 2007;37:8–15.
Wyllie E, Lachhwani DK, Gupta A, Chirla A, Cosmo G, Worley S, et al. Successful surgery for epilepsy due to early brain lesions despite generalized EEG findings. Neurology. 2007;69:389–97.
Hemb M, Velasco TR, Parnes MS, Wu JY, Lerner JT, Matsumoto JH, et al. Improved outcomes in pediatric epilepsy surgery: the UCLA experience. Neurology. 2010;74:1768–75.
Grant PE, Barkovich AJ, Wald LL, Dillon WP, Laxer KD, Vigneron DB. High-resolution surface-coil MR of cortical lesions in medically refractory epilepsy: a prospective study. AJNR Am J Neuroradiol. 1997;18:291–301.
Gupta A, Carreno M, Wyllie E, Bingaman WE. Hemispheric malformations of cortical development. Neurology. 2004;62:S20–6.
Gonzalez-Martinez JA, Gupta A, Kotagal P, Lachhwani D, Wyllie E, Luders HO, et al. Hemispherectomy for catastrophic epilepsy in infants. Epilepsia. 2005;46:1518–25.
Mohamed A, Wyllie E, Ruggieri P, Kotagal P, Babb T, Hilbig A, et al. Temporal lobe epilepsy due to hippocampal sclerosis in pediatric candidates for epilepsy surgery. Neurology. 2001;56:1643–9.
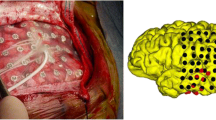
Gupta A, Raja S, Kotagal P, Lachhwani D, Wyllie E, Bingaman WB. Ictal SPECT in children with partial epilepsy due to focal cortical dysplasia. Pediatr Neurol. 2004;31:89–95.
Koh S, Jayakar P, Resnick T, Alvarez L, Liit RE, Duchowny M. The localizing value of ictal SPECT in children with tuberous sclerosis complex and refractory partial epilepsy. Epileptic Disord. 1999;1:41–6.
Vera P, Kaminska A, Cieuta C, Hollo A, Stievenart JL, Gardin I, et al. Use of subtraction ictal SPECT co-registered to MRI for optimizing the localization of seizure foci in children. J Nucl Med. 1999;40:786–92.
RamachandranNair R, Otsubo H, Shroff MM, Ochi A, Weiss SK, Rutka JT, et al. MEG predicts outcome following surgery for intractable epilepsy in children with normal or nonfocal MRI findings. Epilepsia. 2007;48:149–57.
Ochi A, Otsubo H, Iida K, Oishi M, Elliott I, Weiss SK, et al. Identifying the primary epileptogenic hemisphere from electroencephalographic (EEG) and magnetoencephalographic dipole lateralizations in children with intractable epilepsy. J Child Neurol. 2005;20:885–92.
Gaillard WD, Berl MM, Moore EN, Ritzl EK, Rosenberger LR, Weinstein SL, et al. Atypical language in lesional and nonlesional complex partial epilepsy. Neurology. 2007;69:1761–71.
Koudijs SM, Leijten FS, Ramsey NF, van Nieuwenhuizen O, Braun KP. Lateralization of motor innervation in children with intractable focal epilepsy–a TMS and fMRI study. Epilepsy Res. 2010;90:140–50.
Conflict of Interest
Dr. Gupta has research grant from Tuberous Sclerosis Alliance. He is on the editorial board of Pediatric Neurology and Epileptic Disorders. Dr. Gupta is on the professional advisory boards of Tuberous Sclerosis Alliance with no financial support. Dr. Gupta has done teaching, speaking and advisory/consultative work for Lundbeck Inc and Questcor Inc.
Source of Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gupta, A. Epilepsy Surgery in Children: Why, When and How?. Indian J Pediatr 81, 1081–1088 (2014). https://doi.org/10.1007/s12098-014-1541-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-014-1541-1