Abstract
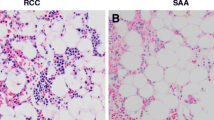
Myelodysplastic syndrome (MDS) comprises of a heterogeneous group of bone marrow disorders resulting from a clonal stem cell defect characterised by cytopenias despite a relatively hypercellular marrow, ineffective hematopoiesis, morphological dysplasia in the marrow elements, no response to hematinics such as iron, B12 or folic acid and risk of progression to leukemia. Myelodysplastic syndrome in childhood is extremely rare and accounts for less than 5 % of all hematopoietic neoplasms in children below the age of 14 y. The primary MDS in children, also known as de novo MDS differs from secondary MDS which generally follows congenital or acquired bone marrow (BM) failure syndromes as well as from therapy related MDS, commonly resulting from cytotoxic therapy. MDS associated with Down syndrome which accounts for approximately one-fourth of cases of childhood MDS is now considered a unique biologic entity synonymous with Down syndrome-related myeloid leukemia and is biologically distinct from other cases of childhood MDS. Refractory cytopenia of childhood (RCC) is the commonest type of MDS. Genetic changes predisposing to MDS in childhood remain largely obscure. Monosomy 7 is by-far the commonest cytogenetic abnormality associated with childhood MDS; however most cases of RCC show a normal karyotype. Complex cytogenetic abnormalities and trisomy 8 and trisomy 21 are also occasionally observed. The most effective and curative treatment is Hematopoietic stem cell transplantation and this is particularly effective in children with the monosomy 7 genetic defect as well as those displaying complex karyotype abnormalities provided it is instituted early in the course of the disease.
Similar content being viewed by others
References
Hasle H, Wadsworth LD, Massing BG, McBride M, Schultz KR. A population-based study of childhood myelodysplastic syndrome in British Columbia, Canada. Br J Haematol. 1999;106:1027–32.
Proytcheva MA. Diagnostic Paediatric Haematopathology. New York: Cambridge University Press; 2011. pp. 254–60.
Hasle H, Niemeyer CM, Chessells JM, Baumann I, Bennett JM, Kerndrup G, et al. A paediatric approach to the WHO classification of myelodysplastic and myeloproliferative diseases. Leukemia. 2003;17:277–82.
Steven H, Harris NL, Jaffe ES, Brunning RD, Vardiman JW, Thiele J. Childhood MDS in WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 4th ed. France: Lyon; 2008. pp. 104–7.
Niemeyer CM, Baumann I. Classification of Childhood Aplastic Anaemias and MDS. ASH Educ Book. 2011;2011:84–9.
Steliarova-Foucher E, Stiller C, Lacour B, Kaatsch P. International classification of childhood cancer, third edition. Cancer. 2005;103:1457–67.
Paediatric Myelodysplastic Syndrome. Prasad Mathew SIOP Education Book 2006, International society of Paediatric Oncology, 38th Congress of the International Society of Paediatric Oncology Geneva, Switzerland·September 17–21, 2006.
Niemeyer CM, Baumann I. Myelodysplastic syndrome in children and adolescents. Semin Hematol. 2008;45:60–70.
Dokal I. Dyskeratosis congenita in all its forms. Br J Haematol. 2000;110:768–79.
Smith OP. Shwachman-diamond syndrome. Semin Hematol. 2002;39:95–102.
Strahm B, Locatelli F, Bader P, Ehlert K, Kremens B, Zintl F, et al. Reduced intensity conditioning in unrelated donor transplantation for refractory cytopenia in childhood. Bone Marrow Transplant. 2007;40:329–33.
Yoshida N, Yagasaki H, Hama A, Takahashi Y, Kosaka Y, Kobayashi R, et al. Predicting response to immunosuppressive therapy in childhood aplastic anaemia. Haematologica. 2011;96:771–4.
The European Working Group of MDS and JMML in Childhood. Proceedings of the 6th International Symposium on Childhood MDS and Bone Marrow Failure syndromes. Prague: Czech Republic; 7–9 November 2012.
McKenna RW. Myelodysplasia and myeloproliferative disorders in children. Am J Clin Pathol. 2004;122:S58–69.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick H, et al. The chronic myeloid leukaemia: Guidelines for distinguishing chronic granulocytic, atypical chronic myeloid and chronic myelomonocytic leukaemia. Proposals by the French-American-British Cooperative Leukaemia Group. Br J Haematol. 1994;87:746–54.
Hoffman R, Furie B, McGlave P, Silberstein LE, Shattil SJ, Benz EJ, et al. Haematology: Basic Principles and Practice. 5th ed. Philadelphia: Churchill Livingstone; 2009.
Hoffbrand VA, Catovsky D, Tuddenham EGD, Green AR. Postgraduate Haematology. 6th ed. New Jersey: Wiley-Blackwell; 2011.
Niemeyer CM, Fenu S, Hasle H, Mann G, Stary J, van Wering E. Differentiating juvenile myelomonocytic leukemia from infectious diseases. Blood. 1998;91:365–7.
Locatelli F, Nöllke P, Zecca M, Korthof E, Lanino E, Peters C, et al; European Working Group on Childhood MDS; European Blood and Marrow Transplantation Group. Hematopoietic stem cell transplantation (HSCT) in children with juvenile myelomonocytic leukemia (JMML): Results of the EWOG-MDS/EBMT trial. Blood. 2005;105:410–9. Epub 2004 Sep 7.
Chatterjee T, Mahapatra M, Dixit A, Naithani R, Tyagi S, Mishra P, et al. Primary myelodysplastic syndrome in children–clinical, haematological and histomorphological profile from a tertiary care centre in India. Hematology. 2005;10:495–9.
Singh ZN, Kashyap R, Pati HP, Choudhry VP. Myelodysplastic syndromes in childhood and adolescence: Clinical and hematological profile. Indian Pediatr. 2001;38:71–6.
Garewal G, Marwaha RK, Roy R, Marwaha N. Clinicohaematological profile and natural history of childhood myelodysplastic syndromes. Indian J Pediatr. 1993;60:573–81.
Nair R, Athale UA, Iyer RS, Nair CN, Pai SK, Kurkure PA, et al. Childhood myelodysplastic syndromes: Clinical features, cytogenetics and prognosis. Indian J Pediatr. 1992;59:443–8.
Agarwal BR, Currimbhoy ZE. Childhood myelodysplasia. Indian Pediatr. 1994;31:797–806.
Luna-Fineman S, Shannon KM, Atwater SK, Davis J, Masterson M, Ortega J, et al. Myelodysplastic and myeloproliferative disorders of childhood: A study of 167 patients. Blood. 1999;93:459–66.
Conflict of Interest
None.
Role of Funding Source
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chatterjee, T., Choudhry, V.P. Childhood Myelodysplastic Syndrome. Indian J Pediatr 80, 764–771 (2013). https://doi.org/10.1007/s12098-013-1130-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-013-1130-8