Abstract
Purpose
The International Extranodal Lymphoma Study Group (IELSG) score is widely used in clinical practice to stratify the risk of primary central nervous system lymphoma (PCNSL) patients. Our study aims to confirm and improve the IELSG score in PCNSL patients based on Chinese populations.
Materials and methods
A total of 79 PCNSL patients were retrospectively analyzed. All patients treated with high-dose methotrexate (HD-MTX)-based therapy collected clinical data. The receiver-operating characteristic (ROC) curve was used to determine the optimal cut-off values for the factors in IELSG score. Progression of disease (POD) at the most landmark time point was determine by Epanechnikov kernel and the area under the ROC curve (AUROC). Kaplan–Meier and multivariable regression methods were used to analyze survival data. Nomogram was generated for calculating the weight of each selected factor.
Results
The traditional IELSG score had no significant difference on OS and PFS except ECOG ≥ 2 and could not stratify the risk groups in PCNSL. The improved IELSG scoring system was established, which incorporated age ≥ 54 years, ECOG ≥ 2, deep brain structure, elevated CSF protein, and LDH/ULN > 0.75. On the other hand, POD18 was identified as a new powerful prognostic factor for PCNSL. In multivariate analysis, POD18 and the improved IELSG scoring system were independent prognostic factors for OS. Nomogram including the two significant variables showed the best performance (C-index = 0.828).
Conclusions
In this study, the IELSG score was improved and a new prognostic indicator POD18 was incorporated to construct a nomogram prognostic model, thereby further improving the predictive ability of the model.






Similar content being viewed by others
Availability of data and materials
The data used and analyzed during the current study are included in the manuscript.
References
Fox CP, Phillips EH, Smith J, Linton K, Gallop-Evans E, Hemmaway C, et al. Guidelines for the diagnosis and management of primary central nervous system diffuse large B-cell lymphoma. Br J Haematol. 2019;184(3):348–63. https://doi.org/10.1111/bjh.15661.
Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375–90. https://doi.org/10.1182/blood-2016-01-643569.
Korfel A, Schlegel U. Diagnosis and treatment of primary CNS lymphoma. Nat Rev Neurol. 2013;9(6):317–27. https://doi.org/10.1038/nrneurol.2013.83.
Houillier C, Soussain C, Ghesquières H, Soubeyran P, Chinot O, Taillandier L, et al. Management and outcome of primary CNS lymphoma in the modern era: an LOC network study. Neurology. 2020;94(10):e1027–39. https://doi.org/10.1212/wnl.0000000000008900.
Villano JL, Koshy M, Shaikh H, Dolecek TA, McCarthy BJ. Age, gender, and racial differences in incidence and survival in primary CNS lymphoma. Br J Cancer. 2011;105(9):1414–8. https://doi.org/10.1038/bjc.2011.357.
Holdhoff M, Mrugala MM, Grommes C, Kaley TJ, Swinnen LJ, Perez-Heydrich C, et al. Challenges in the treatment of newly diagnosed and recurrent primary central nervous system lymphoma. J Natl Compr Cancer Netw JNCCN. 2020;18(11):1571–8. https://doi.org/10.6004/jnccn.2020.7667.
Ferreri AJM, Cwynarski K, Pulczynski E, Fox CP, Schorb E, La Rosée P, et al. Whole-brain radiotherapy or autologous stem-cell transplantation as consolidation strategies after high-dose methotrexate-based chemoimmunotherapy in patients with primary CNS lymphoma: results of the second randomisation of the International Extranodal Lymphoma Study Group-32 phase 2 trial. Lancet Haematol. 2017;4(11):e510–23. https://doi.org/10.1016/s2352-3026(17)30174-6.
Ferreri AJM, Cwynarski K, Pulczynski E, Fox CP, Schorb E, Celico C, et al. Long-term efficacy, safety and neurotolerability of MATRix regimen followed by autologous transplant in primary CNS lymphoma: 7-year results of the IELSG32 randomized trial. Leukemia. 2022;36(7):1870–8. https://doi.org/10.1038/s41375-022-01582-5.
Fortin Ensign SP, Gathers D, Wiedmeier JE, Mrugala MM. Central nervous system lymphoma: novel therapies. Curr Treat Options Oncol. 2022;23(1):117–36. https://doi.org/10.1007/s11864-021-00921-5.
Grommes C, Rubenstein JL, DeAngelis LM, Ferreri AJM, Batchelor TT. Comprehensive approach to diagnosis and treatment of newly diagnosed primary CNS lymphoma. Neuro Oncol. 2019;21(3):296–305. https://doi.org/10.1093/neuonc/noy192.
Jelicic J, Stauffer Larsen T, Bukumiric Z, Juul-Jensen K, Andjelic B. Prognostic models in primary central nervous system lymphoma patients: a systematic review. Crit Rev Oncol Hematol. 2021;161: 103341. https://doi.org/10.1016/j.critrevonc.2021.103341.
Ferreri AJ, Blay JY, Reni M, Pasini F, Spina M, Ambrosetti A, et al. Prognostic scoring system for primary CNS lymphomas: the International Extranodal Lymphoma Study Group experience. J Clin Oncol. 2003;21(2):266–72. https://doi.org/10.1200/jco.2003.09.139.
Abrey LE, Ben-Porat L, Panageas KS, Yahalom J, Berkey B, Curran W, et al. Primary central nervous system lymphoma: the Memorial Sloan-Kettering Cancer Center prognostic model. J Clin Oncol. 2006;24(36):5711–5. https://doi.org/10.1200/jco.2006.08.2941.
Liu CJ, Lin SY, Yang CF, Yeh CM, Kuan AS, Wang HY, et al. A new prognostic score for disease progression and mortality in patients with newly diagnosed primary CNS lymphoma. Cancer Med. 2020;9(6):2134–45. https://doi.org/10.1002/cam4.2872.
Bessell EM, Graus F, Lopez-Guillermo A, Lewis SA, Villa S, Verger E, et al. Primary non-Hodgkin’s lymphoma of the CNS treated with CHOD/BVAM or BVAM chemotherapy before radiotherapy: long-term survival and prognostic factors. Int J Radiat Oncol Biol Phys. 2004;59(2):501–8. https://doi.org/10.1016/j.ijrobp.2003.11.001.
Wu Q, Yang Z, Xu Y. Nomograms predict survival outcome of primary intramedullary spinal cord lymphoma patients. Med Sci Monit Int Med J Exp Clin Res. 2019;25:7418–29. https://doi.org/10.12659/msm.919628.
Luo Q, Yang C, Fu C, Wu W, Wei Y, Zou L. Prognostic role of blood markers in primary central nervous system lymphoma patients treated with high-dose methotrexate-based therapy. Front Oncol. 2021;11: 639644. https://doi.org/10.3389/fonc.2021.639644.
Schorb E, Kasenda B, Atta J, Kaun S, Morgner A, Hess G, et al. Prognosis of patients with primary central nervous system lymphoma after high-dose chemotherapy followed by autologous stem cell transplantation. Haematologica. 2013;98(5):765–70. https://doi.org/10.3324/haematol.2012.076075.
Jahr G, Broi MD, Holte H Jr, Beiske K, Meling TR. Evaluation of Memorial Sloan-Kettering Cancer Center and International Extranodal Lymphoma Study Group prognostic scoring systems to predict overall survival in intracranial primary CNS lymphoma. Brain Behav. 2018;8(3):e00928. https://doi.org/10.1002/brb3.928.
Ghesquières H, Ferlay C, Sebban C, Perol D, Bosly A, Casasnovas O, et al. Long-term follow-up of an age-adapted C5R protocol followed by radiotherapy in 99 newly diagnosed primary CNS lymphomas: a prospective multicentric phase II study of the Groupe d’Etude des Lymphomes de l’Adulte (GELA). Ann Oncol. 2010;21(4):842–50. https://doi.org/10.1093/annonc/mdp529.
Wallace D, Casulo C. Early progressing follicular lymphoma. Curr Oncol Rep. 2021;23(12):149. https://doi.org/10.1007/s11912-021-01126-7.
Conconi A, Thieblemont C, Cascione L, Torri V, Kiesewetter B, Margiotta Casaluci G, et al. Early progression of disease predicts shorter survival in MALT lymphoma patients receiving systemic treatment. Haematologica. 2020;105(11):2592–7. https://doi.org/10.3324/haematol.2019.237990.
Casulo C, Dixon JG, Le-Rademacher J, Hoster E, Hochster HS, Hiddemann W, et al. Validation of POD24 as a robust early clinical end point of poor survival in FL from 5225 patients on 13 clinical trials. Blood. 2022;139(11):1684–93. https://doi.org/10.1182/blood.2020010263.
Luminari S, Merli M, Rattotti S, Tarantino V, Marcheselli L, Cavallo F, et al. Early progression as a predictor of survival in marginal zone lymphomas: an analysis from the FIL-NF10 study. Blood. 2019;134(10):798–801. https://doi.org/10.1182/blood.2019001088.
Maurer MJ, Ghesquières H, Jais JP, Witzig TE, Haioun C, Thompson CA, et al. Event-free survival at 24 months is a robust end point for disease-related outcome in diffuse large B-cell lymphoma treated with immunochemotherapy. J Clin Oncol. 2014;32(10):1066–73. https://doi.org/10.1200/jco.2013.51.5866.
Yamaguchi M, Suzuki R, Kim SJ, Ko YH, Oguchi M, Asano N, et al. Early disease progression in patients with localized natural killer/T-cell lymphoma treated with concurrent chemoradiotherapy. Cancer Sci. 2018;109(6):2056–62. https://doi.org/10.1111/cas.13597.
Yang Y, Wang Y, Liu X, He X, Zhang LL, Wu G, et al. Progression-free survival at 24 months and subsequent survival of patients with extranodal NK/T-cell lymphoma: a China Lymphoma Collaborative Group (CLCG) study. Leukemia. 2021;35(6):1671–82. https://doi.org/10.1038/s41375-020-01042-y.
Maurer MJ, Ellin F, Srour L, Jerkeman M, Bennani NN, Connors JM, et al. International assessment of event-free survival at 24 months and subsequent survival in peripheral t-cell lymphoma. J Clin Oncol. 2017;35(36):4019–26. https://doi.org/10.1200/jco.2017.73.8195.
Advani RH, Skrypets T, Civallero M, Spinner MA, Manni M, Kim WS, et al. Outcomes and prognostic factors in angioimmunoblastic T-cell lymphoma: final report from the international T-cell Project. Blood. 2021;138(3):213–20. https://doi.org/10.1182/blood.2020010387.
Dalia S, Forsyth P, Chavez J, Price S, Shah B, Bello C, et al. Primary B-cell CNS lymphoma clinicopathologic and treatment outcomes in 89 patients from a single tertiary care center. Int J Hematol. 2014;99(4):450–6. https://doi.org/10.1007/s12185-014-1540-z.
Yuan XG, Huang YR, Yu T, Xu Y, Liang Y, Zhang XH, et al. Primary central nervous system lymphoma in China: a single-center retrospective analysis of 167 cases. Ann Hematol. 2020;99(1):93–104. https://doi.org/10.1007/s00277-019-03821-9.
Zhou X, Niu X, Li J, Zhang S, Yang W, Yang Y, et al. Risk factors for early mortality in patients with primary central nervous system lymphoma: a large-cohort retrospective study. World Neurosurg. 2020;138:e905–12. https://doi.org/10.1016/j.wneu.2020.03.150.
Lin CH, Yang CF, Yang HC, Fay LY, Yeh CM, Kuan AS, et al. Risk prediction for early mortality in patients with newly diagnosed primary CNS lymphoma. J Cancer. 2019;10(17):3958–66. https://doi.org/10.7150/jca.32467.
Acknowledgements
Not applicable.
Funding
This work was supported by National Natural Science Foundation of China (81770166, 81720108002, and 81800192), Jiangsu Province’s Medical Elite Programme (ZDRCA2016022), Project of National Key Clinical Specialty, Jiangsu Provincial Special Program of Medical Science (BE2017751) and National Science and Technology Major Project (2018ZX09734007), Nature Science Foundation for Youths of Jiangsu Province (BK20171079), and Young Scholars Fostering Fund of the First Affiliated Hospital of Nanjing Medical University (PY2021026).
Author information
Authors and Affiliations
Contributions
Conception: J-ZW, J-YL, and WX. Interpretation or analysis of data: K-XD and B-HP. Preparation of the manuscript: K-XD and H-RS. Revision for important intellectual content: J-ZW and WX. Supervision: LW, J-HL, YL, and HY.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval and consent to participate
This study was carried out according to the principles established by the Declaration of Helsinki and approved by the Ethical Committee of the Nanjing Medical University (the approval number: 2022-SR-040). All participants were provided with an informed consent that they signed prior to the experiments.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
12094_2023_3292_MOESM1_ESM.docx
Supplementary file1 Table S1 Reference values and the optimal cut-off values for variable. Table S2 Determination of the optimal cut-off values for early disease progression (DOCX 14 KB)


12094_2023_3292_MOESM3_ESM.jpg
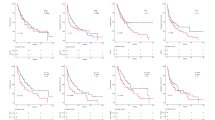
Supplementary file3 Fig. S2 Kaplan-Meier curves for PFS and OS stratified by the original cut-off values of various risk factors. Factors include age ≥60 years (A, B), deep brain structure (C, D) , LDH >271 U/L (E, F) and elevated CSF protein (G, H) (JPG 3506 KB)

Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Du, KX., Shen, HR., Pan, BH. et al. Prognostic value of POD18 combined with improved IELSG in primary central nervous system lymphoma. Clin Transl Oncol 26, 720–731 (2024). https://doi.org/10.1007/s12094-023-03292-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03292-5