Abstract
Objective
The purpose of this study was to explore the appropriate surgical procedure and clinical decision for appendiceal adenocarcinoma.
Methods
A total of 1,984 appendiceal adenocarcinoma patients from 2004 to 2015 were retrospectively identified from the Surveillance, Epidemiology, and End Results (SEER) database. All patients were divided into three groups based on the extent of surgical resection: appendectomy (N = 335), partial colectomy (N = 390) and right hemicolectomy (N = 1,259). The clinicopathological features and survival outcomes of three groups were compared, and independent prognostic factors were assessed.
Results
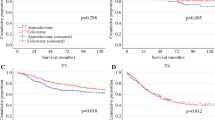
The 5-year OS rates of patients who underwent appendectomy, partial colectomy and right hemicolectomy were 58.3%, 65.5% and 69.1%, respectively (right hemicolectomy vs appendectomy, P < 0.001; right hemicolectomy vs partial colectomy, P = 0.285; partial colectomy vs appendectomy, P = 0.045). The 5-year CSS rates of patients who underwent appendectomy, partial colectomy and right hemicolectomy were 73.2%, 77.0% and 78.7%, respectively (right hemicolectomy vs appendectomy, P = 0.046; right hemicolectomy vs partial colectomy, P = 0.545; partial colectomy vs appendectomy, P = 0.246). The subgroup analysis based on the pathological TNM stage indicated that there was no survival difference amongst three surgical procedures for stage I patients (5-year CSS rate: 90.8%, 93.9% and 98.1%, respectively). The prognosis of patients who underwent an appendectomy was poorer than that of those who underwent partial colectomy (5-year OS rate: 53.5% vs 67.1%, P = 0.005; 5-year CSS rate: 65.2% vs 78.7%, P = 0.003) or right hemicolectomy (5-year OS rate: 74.2% vs 53.23%, P < 0.001; 5-year CSS rate: 65.2% vs 82.5%, P < 0.001) for stage II disease. Right hemicolectomy did not show a survival advantage over partial colectomy for stage II (5-year CSS, P = 0.255) and stage III (5-year CSS, P = 0.846) appendiceal adenocarcinoma.
Conclusions
Right hemicolectomy may not always be necessary for appendiceal adenocarcinoma patients. An appendectomy could be sufficient for therapeutic effect of stage I patients, but limited for stage II patients. Right hemicolectomy was not superior to partial colectomy for advanced stage patients, suggesting omission of standard hemicolectomy might be feasible. However, adequate lymphadenectomy should be strongly recommended.


Similar content being viewed by others
Data availability
The supportive data of this manuscript are available from the public SEER database (https://seer.cancer.gov/).
References
Kelly KJ. Management of Appendix Cancer. Clin Colon Rectal Surg. 2015;28(4):247–55.
Köhler F, Matthes N, Rosenfeldt M, Kunzmann V, Germer CT, Wiegering A. Neoplasms of the Appendix. Dtsch Arztebl Int. 2023 Sep 04 (Forthcoming). https://doi.org/10.3238/arztebl.m2023.0136
Connor SJ, Hanna GB, Frizelle FA. Appendiceal tumors: retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum. 1998;41(1):75–80.
Murphy EM, Farquharson SM, Moran BJ. Management of an unexpected appendiceal neoplasm. Br J Surg. 2006;93(7):783–92.
Benedix F, Reimer A, Gastinger I, Mroczkowski P, Lippert H, Kube R, et al. Primary appendiceal carcinoma–epidemiology, surgery and survival: results of a German multi-center study. Eur J Surg Oncol. 2010;36(8):763–71.
Marmor S, Portschy PR, Tuttle TM, Virnig BA. The rise in appendiceal cancer incidence: 2000–2009. J Gastrointest Surg. 2015;19(4):743–50.
Whitfield CG, Amin SN, Garner JP. Surgical management of primary appendiceal malignancy. Colorectal Dis. 2012;14(12):1507–11.
Gahagan JV, Whealon MD, Phelan MJ, Mills S, Pigazzi A, Stamos MJ, et al. Lymph node positivity in appendiceal adenocarcinoma: should size matter. J Am Coll Surg. 2017;225(1):69–75.
González-Moreno S, Sugarbaker PH. Right hemicolectomy does not confer a survival advantage in patients with mucinous carcinoma of the appendix and peritoneal seeding. Br J Surg. 2004;91(3):304–11.
Turaga KK, Pappas S, Gamblin TC. Right hemicolectomy for mucinous adenocarcinoma of the appendix: just right or too much. Ann Surg Oncol. 2013;20(4):1063–7.
Nasseri YY, Zhu R, Sutanto C, Wai C, Cohen JS, Ellenhorn J, et al. Role of right hemicolectomy in patients with low-grade appendiceal mucinous adenocarcinoma. Am J Surg. 2019;218(6):1239–43.
Hata K, Tanaka N, Nomura Y, Wada I, Nagawa H. Early appendiceal adenocarcinoma. A review of the literature with special reference to optimal surgical procedures. J Gastroenterol. 2002;37(3):210–4.
AlMasri SS, Hammad AY, Singhi AD, Paniccia A, Zureikat AH, Celebrezze JP Jr, et al. Appendectomy Is oncologically equivalent to right hemicolectomy for well-differentiated T1 appendiceal adenocarcinoma. Dis Colon Rectum. 2023;66(1):67–74.
Straker RJ 3rd, Grinberg SZ, Sharon CE, Shannon AB, Fraker DL, Shanmugan S, et al. Pathologic factors associated with low risk of lymph node metastasis in nonmucinous adenocarcinoma of the appendix. Ann Surg Oncol. 2022;29(4):2334–43.
Shannon AB, Goldberg D, Song Y, Paulson EC, Roses RE, Fraker DL, et al. Predictors of lymph node metastases in patients with mucinous appendiceal adenocarcinoma. J Surg Oncol. 2020;122(3):399–406.
Fleischmann I, Warschkow R, Beutner U, Marti L, Schmied BM, Steffen T. Improved survival after retrieval of 12 or more regional lymph nodes in appendiceal cancer. Eur J Surg Oncol. 2017;43(10):1876–85.
Yada H, Sawai K, Taniguchi H, Hoshima M, Katoh M, Takahashi T. Analysis of vascular anatomy and lymph node metastases warrants radical segmental bowel resection for colon cancer. World J Surg. 1997;21(1):109–15.
Mo S, Zhou Z, Ying Z, Dai W, Xiang W, Han L, et al. Epidemiology of and prognostic factors for appendiceal carcinomas: a retrospective, population-based study. Int J Colorectal Dis. 2019;34(11):1915–24.
Day RW, Chang YH, Stucky CC, Gray R, Pockaj B, Wasif N. A predictive model for nodal metastases in patients with appendiceal cancers. Ann Surg. 2021;274(1):155–61.
Enblad M, Graf W, Birgisson H. Risk factors for appendiceal and colorectal peritoneal metastases. Eur J Surg Oncol. 2018;44(7):997–1005.
Funding
This work was supported by the Tianjin Health Science and Technology Project (NO.ZC20213).
Author information
Authors and Affiliations
Contributions
(I) Study conception and design: ZBC and MKW; (II) Data collection: ZBC and WJC; (III) Data analysis and interpretation: ZBC, MZC, WJC and WWQ; (IV). Manuscript drafting: ZBC; (V) Manuscript editing and preparation: ZBC and MZC; (VI) Manuscript review and supervision: YT and MKW. All authors read and approved the final edition of this manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval and informed consent
Ethical approval and informed consent were waived since the data of all patients were obtained from a publicly available database.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, B., Ma, Z., Wang, J. et al. Which is the appropriate surgical procedure for appendiceal adenocarcinoma: appendectomy, partial colectomy or right hemicolectomy?. Clin Transl Oncol 26, 297–307 (2024). https://doi.org/10.1007/s12094-023-03259-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03259-6