Abstract
Purpose
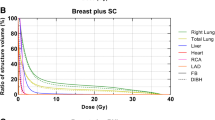
Compared to the free-breathing technique, adjuvant left breast irradiation after breast-conserving surgery or mastectomy using the breath-hold method significantly reduces the heart mean dose, Left anterior descending artery, and ipsilateral lung doses. Movement with deep inspiration may also reduce heart volume in the field and regional node doses.
Materials and methods
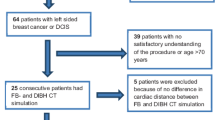
Pre-radiotherapy planning CT was performed in the free-breathing, and breath-hold techniques using RPM, demographic information, clinicopathological data, heart volume in the field, heart mean dose, LAD mean dose, and regional nodal doses were calculated in both free breathing and DIBH. Fifty patients with left breast cancer receiving left breast adjuvant radiation were enrolled.
Results
There was no significant difference in axillary LN coverage between the two techniques, except for SCL maximum dose, Axilla I node maximum dose, and Axilla II minimum dose in favor of the breath hold technique. The mean age was 47.54 years, 78% had GII IDC, 66% had positive LVSI results, and 74% of patients had T2. The breath hold strategy resulted in considerably decreased mean heart dose (p = 0.000), LAD dose (p = 0.000), ipsilateral lung mean dose (p = 0.012), and heart volume if the field (p = 0.013). The mean cardiac dosage and the dose of the LAD were significantly correlated (p = 0.000, R = 0.673). Heart volume in the field and heart mean dosage was not significantly correlated (p = 0.285, r = − 0.108).
Conclusion
When compared to free breathing scans, DIBH procedures result in considerably reduced dosage to the OAR and no appreciable changes in dose exposure to regional lymph node stations in patients with left-sided breast cancer.











Similar content being viewed by others
Data availability
The datasets are available from the first author upon reasonable request.
Abbreviations
- DIBH:
-
Deep inspiration breath-hold
- FB:
-
Free-breathing technique
- RPM:
-
Real-time position management
- BCS:
-
Breast conservative surgery
- OARs:
-
Organs at risk
- WBI:
-
Whole breast radiation
- IHD:
-
Ischemic Heart disease
- PTV:
-
Planning target volume
- RTOG:
-
Radiation therapy oncology group
- CAD:
-
Coronary artery disease
- ABC:
-
Active breathing control
- RNI:
-
Regional nodal irradiation
- LAD:
-
Left anterior descending artery
References
Overgaard M, Hansen PS, Overgaard J, Rose C, Andersson M, Bach F, et al. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish breast cancer cooperative group 82b trial. N Engl J Med. 1997;337:949–55.
Kanapuru B, Ershler WB, Hesdorffer C, Jemal A, Yates JW. Long-term survival of older breast cancer patients: population-based estimates over three decades. Breast Cancer Res Treat. 2012;134:853–7. https://doi.org/10.1007/s10549-012-2115-.
Taylor CW, Brønnum D, Darby SC, Gagliardi G, Hall P, Jensen MB, et al. Cardiac dose estimates from Danish and Swedish breast cancer radiotherapy during 1977–2001. Radiotherapy Oncol. 2011;100:176–83. https://doi.org/10.1016/j.radonc.2011.01.02.
Wikström K, Isacsson U, Nilsson K, Ahnesjö A. Reproducibility of heart and thoracic wall position in repeated deep inspiration breath holds for radiotherapy of left-sided breast cancer patients. Acta Oncol. 2018;57(10):1318–24.
Tanguturi SK, Lyatskaya Y, Chen Y, Catalano PJ, Chen MH, Yeo W, et al. Prospective assessment of deep inspiration breath hold using 3-dimensional surface tracking for irradiation of left-sided breast cancer. Int J Radiat Oncol Biol Phys. 2015;5(6):358–65.
Bhadra K, Patra NB, Manna A, Kabasi A, Pal J, Sarkar SK. Abnormalities by pulmonary regions studied with computer tomography and clinical correlation following local-regional radiotherapy for breast cancer. South Asian J Cancer. 2013;2(1):21–5.
Gokula K, Earnest A, Wong LC. Meta-analysis of incidence of early lung toxicity in 3-dimensional conformal irradiation of breast carcinomas. Radiat Oncol. 2013;8:268.
Henson KE, McGale P, Taylor C, Darby SC. Radiation-related mortality from heart disease and lung cancer more than 20 years after radiotherapy for breast cancer. Br J Cancer. 2013;108(1):179–82.
Krengli M, Sacco M, Loi G, Masini L, Ferrante D, Gambaro G, et al. Pulmonary changes after radiotherapy for conservative treatment of breast cancer: a prospective study. Int J Radiat Oncol Biol Phys. 2008;70(5):1460–7.
Shah C, Badiyan S, Berry S, Khan AJ, Goyal S, Schulte K, et al. Cardiac dose sparing and avoidance techniques inbreast cancer radiotherapy. Radiother Oncol. 2014;112:9–16.
Lu HM, Cash E, Chen MH, Chin L, Manning WJ, Harris J, et al. Reduction of cardiac volume in left-breast treatment fields by respiratory maneuvers: a CT study. Int J Radiat Oncol Biol Phys. 2000;47:895–904.
Chen MH, Cash EP, Danias PG, Kissinger KV, Bornstein BA, Rhodes LM, et al. Respiratory maneuvers decrease irradiatedcardiac volume in patients with left-sided breast cancer. J Cardiovasc Magn Reson. 2002;4:265–71.
Poortmans PM, Collette S, Kirkove C, Van Limbergen E, Budach V, Struikmans H, et al. Internal mammary and medial supraclavicular irradiation in breast cancer. N Engl J Med. 2015;373:317–27.
Poortmans PM, Struikmans H, Bartelink H. Regional nodal irradiation in early-stagebreast cancer. N Engl J Med. 2015;373:1879–80.
Jagsi R, Chadha M, Moni J, Ballman K, Laurie F, Buchholz TA, et al. Radiation field design in the ACOSOG Z0011(Alliance) trial. J Clin Oncol. 2014;32:3600–6.
Borm KJ, Oechsner M, Combs SE, Duma MN. Deep-inspiration breath-hold radiation therapy in breast cancer: a word of caution on the dose to the axillary lymph node levels. Int J Radiat Oncol Biol Phys. 2018;100:263–9.
Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancerand sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305:569–75.
Alongi F, Ricchetti F, Fiorentino A, Gori S. Postoperative breast radiotherapy after neoadjuvant chemotherapy: which uncertainties still remain? Tumori. 2014;100:e212-213.
Mamounas EP. Impact of neoadjuvant chemotherapy on locoregional surgical treatment of breast cancer. Ann Surg Oncol. 2015;22:1425–33.
Schönecker S, Walter F, Freislederer P, Marisch C, Scheithauer H, Harbeck N, et al. Treatment planning and evaluation of gated radiotherapy in left-sided breast cancerpatients using the CatalystTM/SentinelTM system for deep inspirationbreath-hold (DIBH). Radiat Oncol. 2016;11:143.
White J, Tai1 A, Arthur D, Buchholz T, MacDonald S, Marks L, et al. https://www.rtog.org/LinkClick.aspx?fileticket=vzJFhP aBipE%3d&tabid=236.
Feng M, Moran JM, Koelling T, Chughtai A, Chan JL, Freedman L, et al. Development and validation of a heart atlas to study cardiac exposure to radiation following treatment for breast cancer. Int J Radiat Oncol Biol Phys. 2011;79(1):10–8.
Offersen BV, Boersma LJ, Kirkove C, Hol S, Aznar MC, Biete Sola A, et al. ESTRO consensus guideline on target volume delineation for elective radiationtherapy of early-stage breast cancer. Radiother Oncol. 2015;114:3–10.
Measurements TICoRUa. Prescribing, recording, and reporting photon-beam intensity-modulated radiation therapy (IMRT). J ICRU. 2010. https://doi.org/10.1093/jicru/ndq002.
Smyth LM, Knight KA, Aarons YK, Wasiak J. The cardiac dose-sparing benefits of deep inspiration breath-hold in left breast irradiation: a systematic review. J Med Radiat Sci. 2015;62(1):66–73. https://doi.org/10.1002/jmrs.89.
Zurl B, Stranzl H, Winkler P, Kapp KS. Quantitative assessment of irradiated lung volume and lung mass in breast cancer patients treated with tangential fields in combination with deep inspiration breath hold (DIBH). Strahlentherapie und Onkologie. 2010;186(3):157–62. https://doi.org/10.1007/s00066-010-2064-y.
Rosana Y, Leigh C, Karen L, Daphne W. Cardiac dose reduction with deep inspirationn breath hold for left sided breast cancer radiotherapy patients with or without regional nodal irradiation. Radiat oncol. 2015;22(10):200.
Haussmann J, Budach W, Strnad V, Corradini S, Krug D, Schmidt L, et al. Comparing local and systemic control between partial- and whole-breast radiotherapy in low-risk breast cancer-a meta-analysis of randomized trials. Cancers. 2021;13(12):2967.
Schmitt M, Pin Y, Pfumio C, Mathelin C, Pivot X, Noel G. Incidental axillary dose delivery to axillary lymph node levels I-III by diferent techniques of whole-breast irradiation: a systematic literature review. Strahlenther Onkol. 2021;197(9):820–8.
Hildebrandt G, Stachs A, Gerber B, Potenberg J, Krug D, Wolter K, et al. Central review of radiation therapy planning among patients with breastconserving surgery: results from a quality assurance process integrated into the INSEMA trial. Int J Radiat Oncol Biol Phys. 2020;107(4):683–93.
Pazos M, Fiorentino A, Gaasch A, Schonecker S, Reitz D, Heinz C, et al. Dose variability in diferent lymph node levels during locoregional breast cancer irradiation: the impact of deep-inspiration breath hold. Strahlen—Ther Onkol. 2019;195(1):13–20.
Borm KJ, Oechsner M, Combs SE, Duma MN. Deep-inspiration breathhold radiation therapy in breast cancer: a word of caution on the dose to the axillary lymph node levels. Int J Radiat Oncol Biol Phys. 2018;100(1):263–9.
Wolf J, Kurz S, Rothe T, Serpa M, Scholber J, Erbes T, et al. Incidental irradiation of the regional lymph nodes during deep inspiration breath-hold radiation therapy in left-sided breast cancer patients: a dosimetric analysis. BMC Cancer. 2022;22(1):682. https://doi.org/10.1186/s12885-022-09784-x.
Mahmoud AA, Sadaka EA, Abouegylah M, Amin SA, Elmansy H, Asal MF, et al. Impact of breath-hold technique on incidence of cardiac events in adjuvant left breast cancer irradiation. J Cancer Res Clin Oncol. 2022. https://doi.org/10.1007/s00432-022-04551-8. (PMID: 36585984).
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
All authors declare that they have no conflict of interests.
Ethics approval
Not Applicable
Consent to participate
The study was carried out in accordance with the Declaration of Helsinki, and the requirement for informed consent was waived because of the retrospective design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abouegylah, M., Elemary, O., Ahmed, A.A. et al. Impact of breath hold on regional nodal irradiation and heart volume in field in left breast cancer adjuvant irradiation. Clin Transl Oncol 26, 288–296 (2024). https://doi.org/10.1007/s12094-023-03256-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03256-9