Abstract
Background
Triple-positive breast cancer (TPBC) is a tumor that simultaneously expresses estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor-2 (HER2). Luminal A-like TPBC is a special subtype with a favorable prognosis but benefits less from HER2-targeted therapy. However, little is known about how to identify luminal A-like TPBCs. Therefore, our study aims to explore a clinically feasible method to identify luminal A-like TPBCs using immunohistochemical (IHC) markers.
Methods
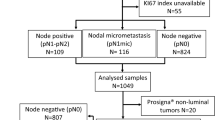
Our cohort enrolled consecutive 190 patients with early-stage TPBCs diagnosed, treated and followed up in our hospital between 2013 and 2019. Patients whose IHC staining displayed ≥ 50% in both ER and PR scores and B-cell lymphoma 2 (BCL2) positivity were classified as cohort A (n = 64), and the rest were enrolled in cohort B (n = 126). Kaplan–Meier plotter and log-rank test were used to compare the survival difference between cohort A and cohort B and the efficacy of trastuzumab therapy in the two cohorts.
Results
The disease-free survival (DFS) of patients in cohort A was significantly better than in cohort B (p = 0.031). In cohort A, there was no statistically significant difference in DFS between patients treated with trastuzumab and those without trastuzumab (p = 0.663). While in cohort B, patients treated with trastuzumab had significantly better DFS than those without trastuzumab (p = 0.032). Multivariate survival analysis showed that cohort A was associated with better DFS(95%CI 1.046–11.776, p = 0.042).
Conclusion
TPBCs consist of heterogeneous subtypes. Detecting the expression of ER, PR and BCL2 via IHC can help identify luminal A-like TPBCs. This study will enable individualized treatment of TPBCs.


Similar content being viewed by others
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Sabatier R, Finetti P, Mamessier E, Raynaud S, Cervera N, Lambaudie E, et al. Kinome expression profiling and prognosis of basal breast cancers. Mol Cancer. 2011;10:86. https://doi.org/10.1186/1476-4598-10-86.
Perou CM, Sørlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000;406(6797):747–52. https://doi.org/10.1038/35021093.
Sørlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98(19):10869–74. https://doi.org/10.1073/pnas.191367098.
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ. Strategies for subtypes–dealing with the diversity of breast cancer: highlights of the St. Gallen international expert consensus on the primary therapy of early breast cancer 2011. Ann Oncol. 2011;22(8):1736–47. https://doi.org/10.1093/annonc/mdr304.
Howlader N, Altekruse SF, Li CI, Chen VW, Clarke CA, Ries LA, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106:5. https://doi.org/10.1093/jnci/dju055.
Gradishar WJ, Anderson BO, Abraham J, Aft R, Agnese D, Allison KH, et al. Breast cancer, version 3 2020, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2020;18(4):452–78. https://doi.org/10.6004/jnccn.2020.0016.
Zhao S, Liu XY, Jin X, Ma D, Xiao Y, Shao ZM, et al. Molecular portraits and trastuzumab responsiveness of estrogen receptor-positive, progesterone receptor-positive, and HER2-positive breast cancer. Theranostics. 2019;9(17):4935–45. https://doi.org/10.7150/thno.35730.
You SH, Chae BJ, Eom YH, Yoo TK, Kim YS, Kim JS, et al. Clinical differences in triple-positive operable breast cancer subtypes in korean patients: an analysis of korean breast cancer registry data. J Breast Cancer. 2018;21(4):415–24. https://doi.org/10.4048/jbc.2018.21.e53.
Kay C, Martínez-Pérez C, Meehan J, Gray M, Webber V, Dixon JM, et al. Current trends in the treatment of HR+/HER2 + breast cancer. Future Oncol. 2021;17(13):1665–81. https://doi.org/10.2217/fon-2020-0504.
Kim HK, Park KH, Kim Y, Park SE, Lee HS, Lim SW, et al. Discordance of the PAM50 intrinsic subtypes compared with immunohistochemistry-based surrogate in breast cancer patients: potential implication of genomic alterations of discordance. Cancer Res Treat. 2019;51(2):737–47. https://doi.org/10.4143/crt.2018.342.
Perillo B, Sasso A, Abbondanza C, Palumbo G. 17Beta-estradiol inhibits apoptosis in MCF-7 cells, inducing bcl-2 expression via two estrogen-responsive elements present in the coding sequence. Mol Cell Biol. 2000;20(8):2890–901. https://doi.org/10.1128/mcb.20.8.2890-2901.2000.
Vici P, Pizzuti L, Sperduti I, Frassoldati A, Natoli C, Gamucci T, et al. “Triple positive” early breast cancer: an observational multicenter retrospective analysis of outcome. Oncotarget. 2016;7(14):17932–44. https://doi.org/10.1863/oncotarget.7480.
Dawson SJ, Makretsov N, Blows FM, Driver KE, Provenzano E, Le Quesne J, et al. BCL2 in breast cancer: a favourable prognostic marker across molecular subtypes and independent of adjuvant therapy received. Br J Cancer. 2010;103(5):668–75. https://doi.org/10.1038/sj.bjc.6605736.
Hwang KT, Kim K, Chang JH, Oh S, Kim YA, Lee JY, et al. BCL2 regulation according to molecular subtype of breast cancer by analysis of the cancer genome atlas database. Cancer Res Treat. 2018;50(3):658–69. https://doi.org/10.4143/crt.2017.134.
Hwang KT, Kim YA, Kim J, Oh HJ, Park JH, Choi IS, et al. Prognostic influences of BCL1 and BCL2 expression on disease-free survival in breast cancer. Sci Rep. 2021;11(1):11942. https://doi.org/10.1038/s41598-021-90506-x.
Hwang KT, Han W, Kim J, Moon HG, Oh S, Song YS, et al. Prognostic influence of BCL2 on molecular subtypes of breast cancer. J Breast Cancer. 2017;20(1):54–64. https://doi.org/10.4048/jbc.2017.20.1.54.
Abdel-Razeq H, Edaily S, Iweir S, Salam M, Saleh Y, Sughayer M, et al. Effect of level of hormone-receptor expression on treatment outcomes of “triple-positive” early-stage breast cancer. Breast Cancer Res Treat. 2021;185(2):459–67. https://doi.org/10.1007/s10549-020-05942-6.
Yang Z, Barnes CJ, Kumar R. Human epidermal growth factor receptor 2 status modulates subcellular localization of and interaction with estrogen receptor alpha in breast cancer cells. Clin Cancer Res. 2004;10(11):3621–8. https://doi.org/10.1158/1078-0432.Ccr-0740-3.
Shou J, Massarweh S, Osborne CK, Wakeling AE, Ali S, Weiss H, et al. Mechanisms of tamoxifen resistance: increased estrogen receptor-HER2/neu cross-talk in ER/HER2-positive breast cancer. J Natl Cancer Inst. 2004;96(12):926–35. https://doi.org/10.1093/jnci/djh166.
Schiff R, Massarweh SA, Shou J, Bharwani L, Mohsin SK, Osborne CK. Cross-talk between estrogen receptor and growth factor pathways as a molecular target for overcoming endocrine resistance. Clin Cancer Res. 2004;10(1 Pt 2):331s-s336. https://doi.org/10.1158/1078-0432.ccr-031212.
Thanopoulou E, Khader L, Caira M, Wardley A, Ettl J, Miglietta F, et al. Therapeutic strategies for the management of hormone receptor-positive, human epidermal growth factor receptor 2-positive (HR+/HER2+) breast cancer: a review of the current literature. Cancers. 2020;12:11. https://doi.org/10.3390/cancers12113317.
Giuliano M, Hu H, Wang YC, Fu X, Nardone A, Herrera S, et al. Upregulation of ER signaling as an adaptive mechanism of cell survival in HER2-positive breast tumors treated with anti-HER2 therapy. Clin Cancer Res. 2015;21(17):3995–4003. https://doi.org/10.1158/1078-0432.Ccr-14-2728.
Hayes DF. HER2 and breast cancer - a phenomenal success story. N Engl J Med. 2019;381(13):1284–6. https://doi.org/10.1056/NEJMcibr1909386.
Loibl S, Gianni L. HER2-positive breast cancer. Lancet. 2017;389(10087):2415–29. https://doi.org/10.1016/s0140-6736(16)32417-5.
Pegram M, Hsu S, Lewis G, Pietras R, Beryt M, Sliwkowski M, et al. Inhibitory effects of combinations of HER-2/neu antibody and chemotherapeutic agents used for treatment of human breast cancers. Oncogene. 1999;18(13):2241–51. https://doi.org/10.1038/sj.onc.1202526.
Emlet DR, Brown KA, Kociban DL, Pollice AA, Smith CA, Ong BB, et al. Response to trastuzumab, erlotinib, and bevacizumab, alone and in combination, is correlated with the level of human epidermal growth factor receptor-2 expression in human breast cancer cell lines. Mol Cancer Ther. 2007;6(10):2664–74. https://doi.org/10.1158/1535-7163.Mct-07-0079.
Zazo S, González-Alonso P, Martín-Aparicio E, Chamizo C, Cristóbal I, Arpí O, et al. Generation, characterization, and maintenance of trastuzumab-resistant HER2 + breast cancer cell lines. Am J Cancer Res. 2016;6(11):2661–78.
Wu YY, Huang TC, Tsai TN, Chen JH, Dai MS, Chang PY, et al. The clinical efficacy and cardiotoxicity of fixed-dose monthly trastuzumab in HER2-positive breast cancer: a single institutional analysis. PLoS ONE. 2016;11(3):e0151112. https://doi.org/10.1371/journal.pone.0151112.
Hsieh PH, Kacew AJ, Dreyer M, Serritella AV, Knoebel RW, Strohbehn GW, et al. Alternative trastuzumab dosing strategies in HER2-positive early breast cancer are associated with patient out-of-pocket savings. NPJ Breast Cancer. 2022;8(1):32. https://doi.org/10.1038/s41523-022-00393-2.
Earl HM, Hiller L, Vallier AL, Loi S, McAdam K, Hughes-Davies L, et al. 6 Versus 12 months of adjuvant trastuzumab for HER2-positive early breast cancer (PERSEPHONE): 4 year disease-free survival results of a randomised phase 3 non-inferiority trial. Lancet. 2019;393(10191):2599–612. https://doi.org/10.1016/s0140-6736(19)30650-6.
Funding
This research did not receive any specific grant from funding agencies from any public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
GY and YX contributed to the conception and design of the study; All authors collected the data; YX and YL analyzed the data and wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No authors have any conflicts of interest to disclose.
Ethical approval
The independent ethics committee/institutional review board of the Second Hospital of Jilin University approved our study (Approval Number: 2022-157). The requirement for informed patient consent was waived due to the study's retrospective nature.
Informed consent
Because of the retrospective nature of the study and the lack of personal details of participants that compromise anonymity, consent was waived.
Consent for publication
All authors read and approved the manuscript as submitted.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, Y., Liang, Y. & Yin, G. Detecting the expression of HRs and BCL2 via IHC can help identify luminal A-like subtypes of triple-positive breast cancers. Clin Transl Oncol 25, 1024–1032 (2023). https://doi.org/10.1007/s12094-022-03007-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-022-03007-2