Abstract
Purpose
Immune checkpoint inhibitors are one of the most effective treatments available in advanced non-small cell lung cancer. However, at present, there are no clinical or analytical biomarkers that define which patients benefit with certainty from these treatments. In our study, we evaluated whether excess weight could be a good predictive biomarker of benefit from these drugs.
Methods
We studied a population of 79 patients, divided into a study group with 39 patients diagnosed with non-small cell lung cancer treated with immunotherapy and 40 patients in a control group, diagnosed with different advanced cancers, treated with non-immunotherapy treatment. We analyzed according to the presence of excess weight or not, the treatment’s outcome in the study group and in the control group (objective response, and progression-free and overall survival).
Results
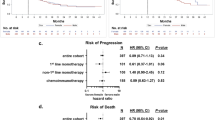
In our study, we detected a better response rate to immunotherapy in patients with excess weight (62.50 vs 26.08%, OR 4.72, p = 0.02), and a better median progression-free survival (14.19 vs 5.03 months, HR 0.50, p = 0.058) and median overall survival (33.84 months vs 20.76 months, HR 0.43, p = 0.01) in the study group. These findings were specific to the immunotherapy group since in the control group, with patients who did not receive immune checkpoint inhibitors, these findings were not found.
Conclusion
Our study suggests that patients with excess weight who receive anti-PD-1 immune checkpoint inhibitors diagnosed with non-small cell lung cancer have a better outcome. This effect is specific to patients receiving immunotherapy.



Similar content being viewed by others
References
Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861–7. https://doi.org/10.1001/jama.293.15.1861 (PMID: 15840860).
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. https://doi.org/10.1001/jama.2012.113905 (PMID:23280227;PMCID:PMC4855514).
Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96. https://doi.org/10.1016/S0140-6736(09)60318-4 (PMID: 19299006; PMCID: PMC2662372).
Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. International agency for research on cancer handbook working group body fatness and cancer-viewpoint of the IARC working group. N Engl J Med. 2016;375(8):794–8. https://doi.org/10.1056/NEJMsr1606602 (PMID: 27557308 PMCID: PMC6754861).
Cortellini A, Bersanelli M, Santini D, Buti S, Tiseo M, Cannita K, Perrone F, Giusti R, De Tursi M, Zoratto F, Marconcini R, Russano M, Zeppola T, Anesi C, Filetti M, Marchetti P, Botticelli A, Gelibter A, De Galitiis F, Vitale MG, Rastelli F, Tudini M, Silva RR, Atzori F, Chiari R, Ricciuti B, De Giglio A, Migliorino MR, Mallardo D, Vanella V, Mosillo C, Bracarda S, Rinaldi S, Berardi R, Natoli C, Ficorella C, Porzio G, Ascierto PA. Another side of the association between body mass index (BMI) and clinical outcomes of cancer patients receiving programmed cell death protein-1 (PD-1)/ Programmed cell death-ligand 1 (PD-L1) checkpoint inhibitors: A multicentre analysis of immune-related adverse events. Eur J Cancer. 2020;128:17–26. https://doi.org/10.1016/j.ejca.2019.12.031 (PMID: 32109847).
Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer. 2004;4(8):579–91. https://doi.org/10.1038/nrc1408 (PMID: 15286738).
Parr CL, Batty GD, Lam TH, Barzi F, Fang X, Ho SC, Jee SH, Ansary-Moghaddam A, Jamrozik K, Ueshima H, Woodward M, Huxley RR. Asia-pacific cohort studies collaboration. Body-mass index and cancer mortality in the Asia-Pacific cohort studies collaboration: pooled analyses of 424,519 participants. Lancet Oncol. 2010;11(8):741–52. https://doi.org/10.1016/S1470-2045(10)70141-8.PMID:20594911;PMCID:PMC4170782.
Tao W, Lagergren J. Clinical management of obese patients with cancer. Nat Rev Clin Oncol. 2013;10(9):519–33. https://doi.org/10.1038/nrclinonc.2013.120 (Epub 2013 Jul 16 PMID: 23856746).
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight obesity and mortality from cancer in a prospectively studied cohort of US adults. N Engl J Med. 2003;348(17):1625–38. https://doi.org/10.1056/NEJMoa021423 (PMID: 12711737).
Dahlberg SE, Schiller JH, Bonomi PB, Sandler AB, Brahmer JR, Ramalingam SS, Johnson DH. Body mass index and its association with clinical outcomes for advanced non-small-cell lung cancer patients enrolled on Eastern cooperative oncology group clinical trials. J Thorac Oncol. 2013;8(9):1121–7. https://doi.org/10.1097/JTO.0b013e31829cf942 (PMID:23887169;PMCID:PMC3763835).
Yang R, Cheung MC, Pedroso FE, Byrne MM, Koniaris LG, Zimmers TA. Obesity and weight loss at presentation of lung cancer are associated with opposite effects on survival. J Surg Res. 2011;170(1):75–83. https://doi.org/10.1016/j.jss.2011.04.061 (PMID: 21704331, PMCID: PMC3154461).
Lam VK, Bentzen SM, Mohindra P, Nichols EM, Bhooshan N, Vyfhuis M, Scilla KA, Feigenberg SJ, Edelman MJ, Feliciano JL. Obesity is associated with long-term improved survival in definitively treated locally advanced non-small cell lung cancer (NSCLC). Lung Cancer. 2017;104:52–7. https://doi.org/10.1016/j.lungcan.2016.11.017 (Epub 2016 Dec 1 PMID: 28213000).
Zhang X, Liu Y, Shao H, Zheng X. Obesity paradox in lung cancer prognosis: evolving biological insights and clinical implications. J Thorac Oncol. 2017;12(10):1478–88. https://doi.org/10.1016/j.jtho.2017.07.022 (PMID: 28757418).
Aparicio T, Ducreux M, Faroux R, Barbier E, Manfredi S, Lecomte T, Etienne PL, Bedenne L, Bennouna J, Phelip JM, François E, Michel P, Legoux JL, Gasmi M, Breysacher G, Rougier P, De Gramont A, Lepage C, Bouché O, JF Seitz for FFCD investigators. Overweight is associated to a better prognosis in metastatic colorectal cancer: a pooled analysis of FFCD trials. Eur J Cancer. 2018;98:1–9. https://doi.org/10.1016/j.ejca.2018.03.031 (PMID: 29807237).
Wang Z, Aguilar EG, Luna JI, Dunai C, Khuat LT, Le CT, Mirsoian A, Minnar CM, Stoffel KM, Sturgill IR, Grossenbacher SK, Withers SS, Rebhun RB, Hartigan-O’Connor DJ, Méndez-Lagares G, Tarantal AF, Isseroff RR, Griffith TS, Schalper KA, Merleev A, Saha A, Maverakis E, Kelly K, Aljumaily R, Ibrahimi S, Mukherjee S, Machiorlatti M, Vesely SK, Longo DL, Blazar BR, Canter RJ, Murphy WJ, Monjazeb AM. Paradoxical effects of obesity on T cell function during tumor progression and PD-1 checkpoint blockade. Nat Med. 2019;25(1):141–51. https://doi.org/10.1038/s41591-018-0221-5 (PMID: 30420753, PMCID: PMC6324991).
Richtig G, Hoeller C, Wolf M, Wolf I, Rainer BM, Schulter G, Richtig M, Grübler MR, Gappmayer A, Haidn T, Kofler J, Huegel R, Lange-Asschenfeldt B, Pichler M, Pilz S, Heinemann A, Richtig E. Body mass index may predict the response to ipilimumab in metastatic melanoma: an observational multi-centre study. PLoS ONE. 2018;13(10): e0204729. https://doi.org/10.1371/journal.pone.0204729.PMID:30273398;PMCID:PMC6166940.
McQuade JL, Daniel CR, Hess KR, Mak C, Wang DY, Rai RR, Park JJ, Haydu LE, Spencer C, Wongchenko M, Lane S, Lee DY, Kaper M, McKean M, Beckermann KE, Rubinstein SM, Rooney I, Musib L, Budha N, Hsu J, Nowicki TS, Avila A, Haas T, Puligandla M, Lee S, Fang S, Wargo JA, Gershenwald JE, Lee JE, Hwu P, Chapman PB, Sosman JA, Schadendorf D, Grob JJ, Flaherty KT, Walker D, Yan Y, McKenna E, Legos JJ, Carlino MS, Ribas A, Kirkwood JM, Long GV, Johnson DB, Menzies AM, Davies MA. Association of body-mass index and outcomes in patients with metastatic melanoma treated with targeted therapy, immunotherapy, or chemotherapy: a retrospective, multicohort analysis. Lancet Oncol. 2018;19(3):310–22. https://doi.org/10.1016/S1470-2045(18)30078-0. (PMID: 29449192; PMCID: PMC5840029).
Murphy WJ, Longo DL. The surprisingly positive association between obesity and cancer immunotherapy efficacy. JAMA. 2019;321(13):1247–8. https://doi.org/10.1001/jama.2019.0463 (PMID: 30882850).
Kichenadasse G, Miners JO, Mangoni AA, Rowland A, Hopkins AM, Sorich MJ. Association between body mass index and overall survival with immune checkpoint inhibitor therapy for advanced non-small cell lung cancer. JAMA Oncol. 2020;6(4):512–8. https://doi.org/10.1001/jamaoncol.2019.5241 (PMID:31876896;PMCID:PMC6990855).
Rogado J, Romero-Laorden N, Sanchez-Torres JM, Ramos-Levi AM, Pacheco-Barcia V, Ballesteros AI, Arranz R, Lorenzo A, Gullon P, Garrido A, Serra López-Matencio JM, Donnay O, Adrados M, Costas P, Aspa J, Alfranca A, Mondejar R, Colomer R. Effect of excess weight and immune-related adverse events on the efficacy of cancer immunotherapy with anti-PD-1 antibodies. Oncoimmunology. 2020;9(1):1751548. https://doi.org/10.1080/2162402X.2020.1751548 (PMID:32363123;PMCID:PMC7185216).
WHO . Health topics. Obesity. [accessed 2020 Apr 12]. https://www.who.int/topics/obesity/en
NIH . Classification of overweight and obesity by BMI, waist circumference, and associated disease risks. [accessed 2020 Apr 12]. https://www.nhlbi.nih.gov/
Rogado J, Sánchez-Torres JM, Romero-Laorden N, Ballesteros AI, Pacheco-Barcia V, Ramos-Leví A, Arranz R, Lorenzo A, Gullón P, Donnay O, Adrados M, Costas P, Aspa J, Alfranca A, Mondéjar R, Colomer R. Immune-related adverse events predict the therapeutic efficacy of anti-PD-1 antibodies in cancer patients. Eur J Cancer. 2019;109:21–7. https://doi.org/10.1016/j.ejca.2018.10.014 (Epub 2019 Jan 22 PMID: 30682533).
Funding
Projects PIE15/00068, PI17/01865 and PI20/01458 (Instituto de Salud Carlos III) awarded to RC; Projects FIS PI19/01491 and CIBER Cardiovascular (Fondo de Investigación Sanitaria del Instituto de Salud Carlos III with co-funding from the Fondo Europeo de Desarrollo Regional FEDER) awarded to AA; CNIO Bioinformatics Unit is supported by the Instituto de Salud Carlos III (ISCIII); Project RETOS RTI2018-097596-B-I00 (AEI/10.13039/501100011033 MCI/FEDER, UE); Projects PI17/00801 and PI21/01111 grants from Instituto de Salud Carlos III and JR17/00007 awarded to NRL, and Project Molecular analysis of the Exhaled Breath Condensate in the management of solitary pulmonary nodule (ideas semilla AECC 2019), from Asociación Española Contra el Cáncer (AECC) awarded to JA.
Author information
Authors and Affiliations
Contributions
J.R. contributed to the conception and design of the study, data acquisition, interpretation of the data and writing of the manuscript. F.P. and K.T. contributed to the statistical analysis and interpretation of the data. J.M.S.T., N.R.L., R.M., O.D., A.B., V.P.B. and J.A. contributed to the data acquisition. F.A-S. contributed to the statistical analysis and interpretation of the data. A.A. contributed to the data acquisition, interpretation of the data and writing of the manuscript. R.C. contributed to the conception and design of the study, interpretation of the data and writing of the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Jacobo Rogado reports personal fees from Roche, AstraZeneca, Merck, Ferrer, Persan Farma, Fresenius Kabi, travel expenses from MSD, BMS, Roche, AstraZeneca and advisor consultancies from Fresenius Kabi. Nuria Romero reports advisory consultancies from Ipsen, Janssen, Clovis, AstraZeneca and research funding from Janssen, MSD and Pfizer. Ramon Colomer reports research funding from Roche, Janssen, BMS, and MSD. All the declared conflict of interests are outside the submitted work. All the other authors have no conflicts to declare.
Ethical approval
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the Hospital Universitario La Princesa on 22 December 2016 under the code 2918.
Informed consent
Informed consent was obtained from all patients involved in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rogado, J., Pozo, F., Troulé, K. et al. Excess weight and anti-PD-1 immune checkpoint inhibitor’s outcomes in non-small cell lung cancer. Clin Transl Oncol 24, 2241–2249 (2022). https://doi.org/10.1007/s12094-022-02887-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-022-02887-8