Abstract
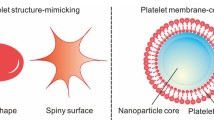
Extensive research is currently being conducted into a variety of bio-inspired biomimetic nanoparticles (NPs) with new cell simulation functions across the fields of materials science, chemistry, biology, physics, and engineering. Cells such as erythrocytes, platelets, and stem cells have been engineered as new drug carriers. The platelet-derived drug delivery system, which is a new targeted drug delivery system (TDDS), can effectively navigate the blood circulatory system and interact with the complex tumor microenvironment; it appears to outperform traditional anticancer drugs; hence, it has attracted considerable research interest. In this review, we describe innovative studies and outline the latest progress regarding the use of platelets as tumor targeting and drug delivery vehicles; we also highlight opportunities and challenges relevant to the manufacture of tumor-related platelet TDDSs.




Similar content being viewed by others
References
Cheng WW, Allen TM. Targeted delivery of anti-CD19 liposomal doxorubicin in B-cell lymphoma: a comparison of whole monoclonal antibody, Fab′ fragments and single chain Fv. J Control Release. 2008;1:50–8.
Yue X, Dai Z. Recent advances in liposomal nanohybrid cerasomes as promising drug nanocarriers. Adv Colloid Interface Sci. 2014;207:32–42.
Mitchell MJ, Billingsley MM, Haley RM, et al. Engineering precision nanoparticles for drug delivery. Nat Rev Drug Discov. 2021;20(2):101–24.
Yin Q, Shen J, Zhang Z, et al. Reversal of multidrug resistance by stimuli-responsive drug delivery systems for therapy of tumor. Adv Drug Deliv Rev. 2013;13–14:1699–715.
Kolhatkar RB, Swaan P, Ghandehari H. Potential oral delivery of 7-ethyl-10-hydroxy-camptothecin (SN-38) using poly (amidoamine) dendrimers. Pharm Res. 2008;7:1723–9.
Bukowski K, Kciuk M, Kontek R. Mechanisms of multidrug resistance in cancer chemotherapy. Int J Mol Sci. 2020;9:3233.
Szakács G, Paterson JK, Ludwig JA, et al. Targeting multidrug resistance in cancer. Nat Rev Drug Discov. 2006;5(3):219–34.
Zhang Y-N, Poon W, Tavares AJ, et al. Nanoparticle–liver interactions: cellular uptake and hepatobiliary elimination. J Control Release. 2016;240:332–48.
De La Harpe KM, Kondiah PP, Choonara YE, et al. The hemocompatibility of nanoparticles: a review of cell–nanoparticle interactions and hemostasis. Cells. 2019;10:1209.
Kunde SS, Wairkar S. Platelet membrane camouflaged nanoparticles: biomimetic architecture for targeted therapy. Int J Pharm. 2021;598:120395.
Choi B, Park W, Park S-B, et al. Recent trends in cell membrane-cloaked nanoparticles for therapeutic applications. Methods. 2020;177:2–14.
Li S, Liu J, Sun M, et al. Cell membrane-camouflaged nanocarriers for cancer diagnostic and therapeutic. Front Pharmacol. 2020;11:24.
Thon JN, Italiano JE. Platelets: production, morphology and ultrastructure. Antiplatelet Agents. 2012;210:3–2.
Ono-Uruga Y, Ikeda Y, Matsubara Y. Platelet production using adipose-derived mesenchymal stem cells: mechanistic studies and clinical application. J Thromb Haemost. 2021;2:342–50.
Ehrmann C, Engel J, Moritz A, et al. Assessment of platelet biology in equine patients with systemic inflammatory response syndrome. J Vet Diagn Invest. 2021;33(2):300–7.
Contursi A, Grande R, Dovizio M, et al. Platelets in cancer development and diagnosis. Biochem Soc Trans. 2018;46(6):1517–27.
Goubran HA, Burnouf T, Stakiw J, et al. Platelet microparticle: a sensitive physiological “fine tuning” balancing factor in health and disease. Transfus Apher Sci. 2015;52(1):12–8.
Chen H, Lu A, Zhang X, et al. Design and development of ICCA as a dual inhibitor of GPIIb/IIIa and P-selectin receptors. Drug Des Dev Ther. 2018;12:2097.
Xu P, Zuo H, Chen B, et al. Doxorubicin-loaded platelets as a smart drug delivery system: An improved therapy for lymphoma. Sci Rep. 2017;7(1):1–16.
Dai L, Gu N, Chen B-A, et al. Human platelets repurposed as vehicles for in vivo imaging of myeloma xenotransplants. Oncotarget. 2016;7(16):21076.
Zhang X, Wang J, Chen Z, et al. Engineering PD-1-presenting platelets for cancer immunotherapy. Nano Lett. 2018;18(9):5716–25.
Yao H, Lan J, Li C, et al. Inhibiting PD-L1 palmitoylation enhances T-cell immune responses against tumours. Nat Biomed Eng. 2019;3(4):306–17.
Li L, Fu J, Wang X, et al. Biomimetic “Nanoplatelets” as a Targeted Drug Delivery Platform for Breast Cancer Theranostics. ACS Appl Mater Interfaces. 2021;13(3):3605–21.
Wang H, Wu J, Williams GR, et al. Platelet-membrane-biomimetic nanoparticles for targeted antitumor drug delivery. J Nanobiotechnol. 2019;17(1):1–16.
Kim MW, Lee G, Niidome T, et al. Platelet-like gold nanostars for cancer therapy: the ability to treat cancer and evade immune reactions. Front Bioeng Biotechnol. 2020;8:133.
Mei D, Gong L, Zou Y, et al. Platelet membrane-cloaked paclitaxel-nanocrystals augment postoperative chemotherapeutical efficacy. J Control Release. 2020;324:341–53.
Pei W, Huang B, Chen S, et al. Platelet-mimicking drug delivery nanoparticles for enhanced chemo-photothermal therapy of breast cancer. Int J Nanomed. 2020;15:10151.
Zarrin A, Foroozesh M, Hamidi M. Carrier erythrocytes: recent advances, present status, current trends and future horizons. Expert Opin Drug Deliv. 2014;11(3):433–47.
Peters D, Kastantin M, Kotamraju VR, et al. Targeting atherosclerosis by using modular, multifunctional micelles. Proc Natl Acad Sci. 2009;106(24):9815–9.
Geranpayehvaghei M, Dabirmanesh B, Khaledi M, et al. Cancer-associated-platelet-inspired nanomedicines for cancer therapy. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2021;13(5):e1702.
Li S, Zhang Y, Wang J, et al. Nanoparticle-mediated local depletion of tumour-associated platelets disrupts vascular barriers and augments drug accumulation in tumours. Nat Biomed Eng. 2017;1(8):667–79.
Zhao G, Rodriguez BL. Molecular targeting of liposomal nanoparticles to tumor microenvironment. Int J Nanomed. 2013;8:61.
Lei Q, Wang D, Sun K, et al. Resistance mechanisms of anti-PD1/PDL1 therapy in solid tumors. Front Cell Dev Biol. 2020;8:672.
Kim H-D, Song G-W, Park S, et al. Association between expression level of PD1 by tumor-infiltrating CD8+ T cells and features of hepatocellular carcinoma. Gastroenterology. 2018;155(6):1936–50.
Han X, Li H, Zhou D, et al. Local and targeted delivery of immune checkpoint blockade therapeutics. Acc Chem Res. 2020;53(11):2521–33.
Huang L, Li Y, Du Y, et al. Mild photothermal therapy potentiates anti-PD-L1 treatment for immunologically cold tumors via an all-in-one and all-in-control strategy. Nat Commun. 2019;10(1):1–15.
Stroncek DF, Rebulla P. Platelet transfusions. The Lancet. 2007;370(9585):427–38.
Han X, Chen J, Chu J, et al. Platelets as platforms for inhibition of tumor recurrence post-physical therapy by delivery of anti-PD-L1 checkpoint antibody. J Control Release. 2019;304:233–41.
Zuo H, Tao J, Shi H, et al. Platelet-mimicking nanoparticles co-loaded with W18O49 and metformin alleviate tumor hypoxia for enhanced photodynamic therapy and photothermal therapy. Acta Biomater. 2018;80:296–307.
Zhou M, Lai W, Li G, et al. Platelet membrane-coated and VAR2CSA malaria protein-functionalized nanoparticles for targeted treatment of primary and metastatic cancer. ACS Appl Mater Interfaces. 2021;13(22):25635–48.
Zhang Y, Liu G, Wei J, et al. Platelet membrane-based and tumor-associated platelet-targeted drug delivery systems for cancer therapy. Front Med. 2018;12(6):667–77.
Ding K, Zheng C, Sun L, et al. NIR light-induced tumor phototherapy using ICG delivery system based on platelet-membrane-camouflaged hollow bismuth selenide nanoparticles. Chin Chem Lett. 2020;35(5):1168–72.
Vinholt P, Frederiksen H, Hvas AM, et al. Measurement of platelet aggregation, independently of patient platelet count: a flow-cytometric approach. J Thromb Haemost. 2017;15(6):1191–202.
Gillet J-P, Gottesman M M, Mechanisms of multidrug resistance in cancer. In Multi-drug Rresist Cancer, Springer, New york: 2010; pp 47–76.
Bhattacharya DS, Svechkarev D, Bapat A, et al. Sulfation modulates the targeting properties of hyaluronic acid to P-selectin and CD44. ACS Biomater Sci Eng. 2020;6(6):3585–98.
Song Y, Huang Z, Liu X, et al. Platelet membrane-coated nanoparticle-mediated targeting delivery of Rapamycin blocks atherosclerotic plaque development and stabilizes plaque in apolipoprotein E-deficient (ApoE−/−) mice. Nanomed Nanotechnol Biol Med. 2019;15(1):13–24.
Zhang F, Cao J, Chen X, et al. Noninvasive dynamic imaging of tumor early response to nanoparticle-mediated photothermal therapy. Theranostics. 2015;5(12):1444.
Wu L, Xie W, Zan H-M, et al. Platelet membrane-coated nanoparticles for targeted drug delivery and local chemo-photothermal therapy of orthotopic hepatocellular carcinoma. J Mater Chem B. 2020;8(21):4648–59.
Kasashima H, Duran A, Cid-Diaz T, et al. An orthotopic implantation mouse model of hepatocellular carcinoma with underlying liver steatosis. STAR Protoc. 2020;1(3):100185.
Zhang N, Zhu H, Dong Y, et al. Establishment of an insufficient radiofrequency ablation orthotopic nude mouse model of hepatocellular carcinoma to study the invasiveness and metastatic potential of residual cancer. Oncol Lett. 2019;18(3):2548–53.
Vines J, Lim D, Park H. Contemporary polymer-based nanoparticle systems for photothermal therapy. Polymers. 2018;10(12):1357.
Cheng K, Zhang R, Yang X, et al. One-for-all nanoplatform for synergistic mild cascade-potentiated ultrasound therapy induced with targeting imaging-guided photothermal therapy. ACS Appl Mater Interface. 2020;12(36):40052–66.
Everts P, Onishi K, Jayaram P, et al. Platelet-rich plasma: new performance understandings and therapeutic considerations in 2020. Int J Mol Sci. 2020;21(20):77945.
Hayashi T, Aminaka R, Fujimura Y, et al. A more efficient preparation system for HLA-eliminated platelets. Vox Sang. 2020;115(2):159–66.
Du Y, Chen B. Combination of drugs and carriers in drug delivery technology and its development. Drug Des Dev Ther. 2019;13:1401–8.
Wang X, Liang G, Hao X, et al. Bioinspired drug delivery carrier for enhanced tumor-targeting in melanoma mice model. J Biomed Nanotechnol. 2019;15(7):1482–91.
Kailashiya J, Gupta V, Dash D. Engineered human platelet-derived microparticles as natural vectors for targeted drug delivery. Oncotarget. 2019;10(56):5835–46.
Sarkar S, Alam M, Shaw J, et al. Drug delivery using platelet cancer cell interaction. Pharm Res. 2013;30(11):2785–94.
Wang S, Li Z, Xu R. Human cancer and platelet interaction, a potential therapeutic target. Int J Mol Sci. 2018;19(4):1246.
Sharma D, Brummel-Ziedins K, Bouchard B, et al. Platelets in tumor progression: a host factor that offers multiple potential targets in the treatment of cancer. J Cell Physiol. 2014;229(8):1005–15.
Koupenova M, Clancy L, Corkrey H, et al. Circulating platelets as mediators of immunity, inflammation, and thrombosis. Circ Res. 2018;122(2):337–51.
Van Der Meijden P, Heemskerk J. Platelet biology and functions: new concepts and clinical perspectives. Nat Rev Cardiol. 2019;16(3):166–79.
Suzuki-Inoue K. Platelets and cancer-associated thrombosis: focusing on the platelet activation receptor CLEC-2 and podoplanin. Hematol Am Soc Hematol Educ Program. 2019;2019(1):175–81.
Paliwal R, Babu R, Palakurthi S. Nanomedicine scale-up technologies feasibilities and challenges. AAPS PharmSciTech. 2014;15(6):1527–34.
Acknowledgements
This work was supported by the Scientific and Technological Innovation Major Base of Guangxi (No. 2018-15-Z04), the State Project for Essential Drug Research and Development (No. 2019ZX09301132), Guangxi Key Research and Development Project (No. AB20117001). Since we have been funded by the following funding number, add a funding number: National Natural Science Foundation of China (No.82060562).
Author information
Authors and Affiliations
Contributions
Writing—original draft preparation: GX, ZZ, QC. Writing—review and editing: TW, WS, LG, XL, YH, ML. YZ, PW: Funding acquisition, LZ, JH: Critically revised.
Corresponding author
Ethics declarations
Conflict of interests
The authors have declared that no competing interest exists.
Ethical approval
This manuscript does not contain any human or animals related research, and does not involve any ethical experiments.
Informed consent
Not Applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xiao, G., Zhang, Z., Chen, Q. et al. Platelets for cancer treatment and drug delivery. Clin Transl Oncol 24, 1231–1237 (2022). https://doi.org/10.1007/s12094-021-02771-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-021-02771-x