Abstract
Purpose
Patients presenting with lymphovascular space invasion (LVSI) had an absolute decrease in survival. In our present study, the potential roles of LVSI on tumor characteristics was explored to predict the difference in the prognosis of ER and HER2 positive T1 tumors.
Methods
A total of 142 breast cancer patients diagnosed with ER+ and HER2+ tumors whose tumor size was ≤ 2 cm were included in this analysis. One hundred forty-two patients were divided into four groups, group 1 (lymph nodes+ and LVSI+), group 2 (lymph nodes+ and LVSI−), group 3 (lymph nodes− and LVSI+), group 4 (lymph nodes− and LVSI−). Univariate and multivariate Cox proportional hazard models were used to identify independent prognostic factors and calculate the HR and 95% CI. Kaplan–Meier and Cox regression models were used to test the prognostic significance.
Results
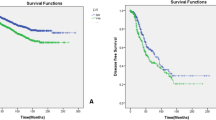
LVSI positivity was significantly associated with patient age, menopausal status, tumor size, lymph node status, Ki67, PR, and tumor grade. In the univariate and multivariate model, LVSI, PR, and Ki67 were significantly associated with DFS, and LVSI, lymph node status, PR, and Ki67 were significantly associated with OS. LVSI was significantly related to increased risk of DFS and OS only in the PR-negative and low-positive subgroups. It was a prognostic factor for DFS but not for OS in women with low Ki67 and was associated with DFS and OS in high-Ki67 tumors. Furthermore, patients who presented with only LVSI had a significantly worse survival rate than those with lymph node metastasis without LVSI in small tumors.
Conclusion
The presence of LVSI was highlighted as a variable significant to survival. In further clinical practice, patients with LVSI may need more intensive treatment in certain populations.





Similar content being viewed by others
References
Alvarez Goyanes RI, Escobar Perez X, Camacho Rodriguez R, et al. Hormone receptors and other prognostic factors in breast cancer in Cuba. MEDICC Rev. 2010;12(1):36–40.
Saurel CA, Patel TA, Perez EA. Changes to adjuvant systemic therapy in breast cancer: a decade in review. Clin Breast Cancer. 2010;10(3):196–208.
Perou CM, Sorlie T, Eisen MB, et al. Molecular portraits of human breast tumours. Nature. 2000;406:747–52.
Sawe RT, Kerper M, Badve S, et al. Aggressive breast cancer in western Kenya has early onset, high proliferation, and immune cell infiltration. BMC Cancer. 2016;16:204.
Mohammed RA, Martin SG, Mahmmod AM, et al. Objective assessment of lymphatic and blood vascular invasion in lymph node-negative breast carcinoma: findings from a large case series with long-term follow-up. J Pathol. 2011;223:358–65.
Coates AS, Winer EP, Goldhirsch A, Gelber RD, Gnant M, Piccart-Gebhart M, et al. Panel Members: Tailoring therapies—improving the management of early breast cancer: St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol. 2015;8:1533–46.
André F, Baselga J, Bergh J, Bonnefoi H, Brucker SY, Cardoso F, et al. De-escalating and escalating treatments for early-stage breast cancer: the St. Gallen International Expert Consensus Conference on the Primary Therapy of Early Breast Cancer 2017. Ann Oncol. 2017;28:1700–12.
Arpino G, Weiss H, Lee AV, Schiff R, De Placido S, Osborne CK, Elledge RM. Estrogen receptor-positive, progesterone receptor-negative breast cancer: association with growth factor receptor expression and tamoxifen resistance. J Natl Cancer Inst. 2005;97:1254–61.
Shen SD, Xiao GF, Du RC, et al. Predictors of lymphovascular invasion identified from pathological factors in Chinese patients with breast cancer. Oncotarget. 2018;9(2):2468–74.
Sayed S, Moloo Z, Wasike R, Bird P, Oigara R, Govender D, Kibera J, Carrara H, Saleh M. Is breast cancer from sub Saharan Africa truly receptor poor? Prevalence of ER/PR/HER2 in breast cancer from Kenya. Breast. 2014;23(5):591–6.
Ignatov T, Eggemann H, Burger E, Costa SD, Ignatov A. Management of small T1a/b breast cancer by tumor subtype. Breast Cancer Res Treat. 2017;163(1):111–8.
Vaz-Luis I, Ottesen RA, Hughes ME, et al. Outcomes by tumor subtype and treatment pattern in women with small, node-negative breast cancer: a multi-institutional study. J Clin Oncol. 2014;32(20):2142–50.
Hammond ME, Hayes DF, Dowestt M, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer (unabridged version). Arch Pathol Lab Med. 2010;134(7):e48–e72.
Sauter G, Lee J, Bartlett JM, Slamon DJ, Press MF. Guidelines for human epidermal growth factor receptor 2 testing: biologic and methodologic considerations. J Clin Oncol. 2009;27:1323–33.
Cheang MC, Chia SK, Voduc D, Gao D, Leung S, Snider J, Watson M, Davies S, Bernard PS, Parker JS. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009;101:736–50.
Rosen PP. Tumor emboli in intramammary lymphatics in breast carcinoma: pathologic criteria for diagnosis and clinical significance. Pathol Annu. 1983;18:215–32.
Hoda Syed A, Hoda Rana S, Scott M, et al. Issues relating to lymphovascular invasion in breast cancer. Adv Anat Pathol. 2006;13:308–15.
Bauer K, Parise C, Caggiano V. Use of ER/PR/HER2 subtypes in conjunction with the 2007 St Gallen Consensus Statement for early breast cancer. BMC Cancer. 2010;10:228.
Ugras S, Stempel M, Patil S, Morrow M. Estrogen receptor, progesterone receptor, and HER2 status predict lymphovascular invasion and lymph node involvement. Ann Surg Oncol. 2014;21:3780–6.
Sara MT, William TB, Hao G, et al. Seven-year (yr) follow-up of adjuvant paclitaxel (T) and trastuzumab (H) (APT trial) for node-negative, HER2-positive breast cancer (BC). J Clin Oncol. 2017;35(15):511.
Colleoni M, Rotmensz N, Maisonneuve P, et al. Prognostic role of the extent of peritumoral vascular invasion in operable breast cancer. Ann Oncol. 2007;18:1632–40.
Zhao Y, Zhang DW. Biomarker alteration to neoadjuvant chemotherapy predict pathological response and prognosis in breast cancer patients. Cancer Genet Epigenet. 2018;6(1):1–12.
Prat A, Cheang MC, Martín M, et al. Prognostic significance of progesterone receptor-positive tumor cells within immunohistochemically defined luminal A breast cancer. J Clin Oncol. 2013;31(2):203–9.
Yerushalmi R, Woods R, Ravdin PM, Hayes MM, Gelmon KA. Ki67 in breast cancer: prognostic and predictive potential. Lancet Oncol. 2010;11:174–83.
Elkablawy MA, Albasri AM, Mohammed RA, Hussainy AS, Nouh MM, Alhujaily AS. Ki67 expression in breast cancer correlation with prognostic markers and clinicopathological parameters in Saudi patients. Saudi Med J. 2016;37:137–41.
Milam MR, Frumovitz M, dos Reis R, et al. Preoperative lymph-vascular space invasion is associated with nodal metastases in women with early-stage cervical cancer. Gynecol Oncol. 2007;106:12–5.
Ferrandina G, Pedone Anchora L, Gallotta V, et al. Can we define the risk of lymph node metastasis in early-stage cervical cancer patients? A large-scale, retrospective study. Ann Surg Oncol. 2017;24:2311–8.
Acknowledgements
We would like to extend our sincere gratitude to our departmental chair for all their support. In addition, we would like to give many thanks to our physicians, engineers, and nurses as well as other staff of the department.
Funding
Heilongjiang Province of Science and Technology (Grant 201716), and the Harbin Science and Technology Bureau (Grant 2017RAXQJ067).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflicts of interest in this work.
Ethical approval
Ethical approval was provided by the Institutional Review Board of Harbin Medical University.
Informed consent
Informed consent was obtained from all patients included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhao, Y., Yang, N., Wang, X. et al. Potential roles of lymphovascular space invasion based on tumor characteristics provide important prognostic information in T1 tumors with ER and HER2 positive breast cancer. Clin Transl Oncol 22, 2275–2285 (2020). https://doi.org/10.1007/s12094-020-02369-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-020-02369-9