Abstract
Background
Until now, there is no clear conclusion on the relationship between the surgical margin status after radical prostatectomy (RP) and prostate cancer-specific mortality (PCSM). Therefore, we conducted this systematic review and meta-analysis based on all eligible case–control studies.
Methods
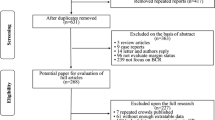
A systematic and comprehensive literature search was performed based on PUBMED and EMBASE to identify all of the potentially relevant publications which were published before September 2019. Hazard ratio (HR) for PCSM was independently extracted by two reviewers from all eligible studies. Pooled HR estimates with their corresponding 95% confidence intervals (95% CIs) were computed by Stata12.0.
Results
Total 15 eligible studies were included in this meta-analysis. The pooled results showed that patients with positive surgical margin (PSM) after RP may have higher PCSM than those who had a negative surgical margin (HR 1.44, P = 0.043). In the subgroup analysis, we found that no matter whether the pathological stage of the patients is T2 or T3, PSM is indicative of a high PCSM and that the PCSM of T3 is higher than T2 (Pathological stage T3, HR 1.77, P = 0.032; Pathological stage T2, HR 1.56, P = 0.003). In addition, by performing the subgroup analysis of Gleason score, we concluded that both Gleason score 8–10 and Gleason score ≤ 7 would increase the risk of PCSM, and the former was more significant than the latter (Gleason score 8–10, HR 1.88, P < 0.001; Gleason score ≤ 7, HR 1.38, P = 0.039). Moreover, PSM increased PCSM regardless of whether the patients received radiation therapy or not (radiation therapy, HR 1.92, P < 0.001; no radiation therapy, HR 1.42, P < 0.001).
Conclusions
This meta-analysis demonstrated that patients with PSM after RP may have an elevated PCSM. However, to evaluate these correlations in more details, it is necessary to conduct further studies on a larger sample size.







Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics. CA. 2019;69(1).
Mehralivand S, van der Poel H, Winter A, Choyke PL, Pinto PA, Turkbey B. Sentinel lymph node imaging in urologic oncology. Transl Androl Urol. 2018;7(5):887–902.
Yossepowitch O, Bjartell A, Eastham JA, Graefen M, Guillonneau BD, Karakiewicz PI, Montironi R, Montorsi F. Positive surgical margins in radical prostatectomy: outlining the problem and its long-term consequences. Eur Urol. 2009;55(1):87–99.
Chalfin HJ, Dinizo M, Trock BJ, Feng Z, Partin AW, Walsh PC, Humphreys E, Han M. Impact of surgical margin status on prostate-cancer-specific mortality. BJU Int. 2012;110(11):1684–9.
Hashimoto T, Yoshioka K, Horiguchi Y, Inoue R, Yoshio O, Nakashima J, Tachibana M. Clinical effect of a positive surgical margin without extraprostatic extension after robot-assisted radical prostatectomy. Urol Oncol. 2015;33(12):503.e501–.e506.
Sammon JD, Trinh Q-D, Sukumar S, Ravi P, Friedman A, Sun M, Schmitges J, Jeldres C, Jeong W, Mander N, et al. Risk factors for biochemical recurrence following radical perineal prostatectomy in a large contemporary series: a detailed assessment of margin extent and location. Urol Oncol. 2013;31(8):1470–6.
Mithal P, Howard LE, Aronson WJ, Terris MK, Cooperberg MR, Kane CJ, Amling C, Freedland SJ. Positive surgical margins in radical prostatectomy patients do not predict long-term oncological outcomes: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) cohort. BJU Int. 2016;117(2):244–8.
Simon RM, Howard LE, Freedland SJ, Aronson WJ, Terris MK, Kane CJ, Amling CL, Cooperberg MR, Vidal AC. Adverse pathology and undetectable ultrasensitive prostate-specific antigen after radical prostatectomy: Is adjuvant radiation warranted? BJU Int. 2016;117(6):897–903.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Heering M, Berg KD, Brasso K, Iversen P, Røder MA. Radical prostatectomy in Denmark: survival analysis and temporal trends in clinicopathological parameters with up to 20 years of follow-up. Surg Oncol. 2017;26(1):21–7.
Herforth C, Stroup SP, Chen Z, Howard LE, Freedland SJ, Moreira DM, Terris MK, Aronson WJ, Cooperberg MR, Amling CL, et al. Radical prostatectomy and the effect of close surgical margins: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) database. BJU Int. 2018;122(4):592–8.
Knoedler JJ, Karnes RJ, Thompson RH, Rangel LJ, Bergstralh EJ, Boorjian SA. The association of tumor volume with mortality following radical prostatectomy. Prostate Cancer Prostatic Dis. 2014;17(2):144–8.
Lewinshtein D, Teng B, Valencia A, Gibbons R, Porter CR. The long-term outcomes after radical prostatectomy of patients with pathologic Gleason 8–10 disease. Adv Urol. 2012;2012:428098.
Mauermann J, Fradet V, Lacombe L, Dujardin T, Tiguert R, Tetu B, Fradet Y. The impact of solitary and multiple positive surgical margins on hard clinical end points in 1712 adjuvant treatment-naive pT2-4 N0 radical prostatectomy patients. Eur Urol. 2013;64(1):19–25.
Mitchell CR, Boorjian SA, Umbreit EC, Rangel LJ, Carlson RE, Karnes RJ. 20-Year survival after radical prostatectomy as initial treatment for cT3 prostate cancer. BJU Int. 2012;110(11):1709–13.
Moschini M, Sharma V, Zattoni F, Boorjian SA, Frank I, Gettman MT, Thompson RH, Tollefson MK, Kwon ED, Karnes RJ. Risk stratification of pN+ prostate cancer after radical prostatectomy from a large single institutional series with long-term followup. J Urol. 2016;195(6):1773–8.
Ploussard G, Agamy MA, Alenda O, Allory Y, Mouracade P, Vordos D, Hoznek A, Abbou C-C, de la Taille A, Salomon L. Impact of positive surgical margins on prostate-specific antigen failure after radical prostatectomy in adjuvant treatment-naïve patients. BJU Int. 2011;107(11):1748–54.
Preisser F, Mazzone E, Knipper S, Nazzani S, Bandini M, Shariat SF, Tian Z, Saad F, Montorsi F, Zorn KC, et al. Rates of positive surgical margins and their effect on cancer-specific mortality at radical prostatectomy for patients with clinically localized prostate cancer. Clin Genitourin Cancer. 2019;17(1):e130–e139139.
Retèl VP, Bouchardy C, Usel M, Neyroud-Caspar I, Schmidlin F, Wirth G, Iselin C, Miralbell R, Rapiti E. Determinants and effects of positive surgical margins after prostatectomy on prostate cancer mortality: a population-based study. BMC Urol. 2014;14:86.
Stephenson AJ, Eggener SE, Hernandez AV, Klein EA, Kattan MW, Wood DP, Rabah DM, Eastham JA, Scardino PT. Do margins matter? The influence of positive surgical margins on prostate cancer-specific mortality. Eur Urol. 2014;65(4):675–80.
Touijer KA, Mazzola CR, Sjoberg DD, Scardino PT, Eastham JA. Long-term outcomes of patients with lymph node metastasis treated with radical prostatectomy without adjuvant androgen-deprivation therapy. Eur Urol. 2014;65(1):20–5.
Viers BR, Sukov WR, Gettman MT, Rangel LJ, Bergstralh EJ, Frank I, Tollefson MK, Thompson RH, Boorjian SA, Karnes RJ. Primary Gleason grade 4 at the positive margin is associated with metastasis and death among patients with Gleason 7 prostate cancer undergoing radical prostatectomy. Eur Urol. 2014;66(6):1116–24.
Wright JL, Dalkin BL, True LD, Ellis WJ, Stanford JL, Lange PH, Lin DW. Positive surgical margins at radical prostatectomy predict prostate cancer specific mortality. J Urol. 2010;183(6):2213–8.
Tan PH, Cheng L, Srigley JR, Griffiths D, Humphrey PA, van der Kwast TH, Montironi R, Wheeler TM, Delahunt B, Egevad L, et al: International Society of Urological Pathology (ISUP) Consensus Conference on Handling and Staging of Radical Prostatectomy Specimens. Working group 5: surgical margins. Mod Pathol. 2011;24(1):48–57.
Hsu M, Chang SL, Ferrari M, Nolley R, Presti JC, Brooks JD. Length of site-specific positive surgical margins as a risk factor for biochemical recurrence following radical prostatectomy. Int J Urol. 2011;18(4):272–9.
Bong GW, Ritenour CWM, Osunkoya AO, Smith MT, Keane TE. Evaluation of modern pathological criteria for positive margins in radical prostatectomy specimens and their use for predicting biochemical recurrence. BJU Int. 2009;103(3):327–31.
Lu J, Wirth GJ, Wu S, Chen J, Dahl DM, Olumi AF, Young RH, McDougal WS, Wu C-L. A close surgical margin after radical prostatectomy is an independent predictor of recurrence. J Urol. 2012;188(1):91–7.
May M, Brookman-May S, Weißbach L, Herbst H, Gilfrich C, Papadopoulos T, Roigas J, Hofstädter F, Wieland WF, Burger M. Solitary and small (≤3 mm) apical positive surgical margins are related to biochemical recurrence after radical prostatectomy. Int J Urol. 2011;18(4):282–9.
Psutka SP, Feldman AS, Rodin D, Olumi AF, Wu C-L, McDougal WS. Men with organ-confined prostate cancer and positive surgical margins develop biochemical failure at a similar rate to men with extracapsular extension. Urology. 2011;78(1):121–5.
Shikanov S, Marchetti P, Desai V, Razmaria A, Antic T, Al-Ahmadie H, Zagaja G, Eggener S, Brendler C, Shalhav A. Short (≤1 mm) positive surgical margin and risk of biochemical recurrence after radical prostatectomy. BJU Int. 2013;111(4):559–63.
Beauval J-B, Roumiguié M, Filleron T, Benoit T, de la Taille A, Malavaud B, Salomon L, Soulié M, Ploussard G. Biochemical recurrence-free survival and pathological outcomes after radical prostatectomy for high-risk prostate cancer. BMC Urol. 2016;16(1):26.
Fontenot PA, Mansour AM. Reporting positive surgical margins after radical prostatectomy: time for standardization. BJU Int. 2013;111(8):E290–E299299.
Huang JG, Pedersen J, Hong MKH, Harewood LM, Peters J, Costello AJ, Hovens CM, Corcoran NM. Presence or absence of a positive pathological margin outperforms any other margin-associated variable in predicting clinically relevant biochemical recurrence in Gleason 7 prostate cancer. BJU Int. 2013;111(6):921–7.
Kanehira M, Takata R, Ishii S, Ito A, Ikarashi D, Matsuura T, Kato Y, Obara W. Predictive factors for short-term biochemical recurrence-free survival after robot-assisted laparoscopic radical prostatectomy in high-risk prostate cancer patients. Int J Clin Oncol. 2019;24(9):1099–104.
van Oort IM, Bruins HM, Kiemeney LALM, Knipscheer BC, Witjes JA. Hulsbergen-van de Kaa CA: the length of positive surgical margins correlates with biochemical recurrence after radical prostatectomy. Histopathology. 2010;56(4):464–71.
Zhang L, Wu B, Zha Z, Zhao H, Jiang Y, Yuan J. Positive surgical margin is associated with biochemical recurrence risk following radical prostatectomy: a meta-analysis from high-quality retrospective cohort studies. World J Surg Oncol. 2018;16(1):124.
Yossepowitch O, Briganti A, Eastham JA, Epstein J, Graefen M, Montironi R, Touijer K. Positive surgical margins after radical prostatectomy: a systematic review and contemporary update. Eur Urol. 2014;65(2):303–13.
Zhang L, Wu B, Zha Z, Zhao H, Yuan J, Jiang Y, Yang W. Surgical margin status and its impact on prostate cancer prognosis after radical prostatectomy: a meta-analysis. World J Urol. 2018;36(11):1803–15.
Bolton DM, Papa N, Ta AD, Millar J, Davidson AJ, Pedersen J, Syme R, Patel MI, Giles GG. Predictors of prostate cancer specific mortality after radical prostatectomy: 10 year oncologic outcomes from the Victorian Radical Prostatectomy Registry. BJU Int. 2015;116(Suppl 3):66–72.
Fleshner NE, Evans A, Chadwick K, Lawrentschuk N, Zlotta A. Clinical significance of the positive surgical margin based upon location, grade, and stage. Urol Oncol. 2010;28(2):197–204.
Jang WS, Kim LHC, Yoon CY, Rha KH, Choi YD, Hong SJ, Ham WS. Effect of Preoperative Risk Group stratification on oncologic outcomes of patients with adverse pathologic findings at radical prostatectomy. PLoS ONE. 2016;11(10):e0164497.
Mithal P, Howard LE, Aronson WJ, Kane CJ, Cooperberg MR, Terris MK, Amling CL, Freedland SJ. Prostate-specific antigen level, stage or Gleason score: which is best for predicting outcomes after radical prostatectomy, and does it vary by the outcome being measured? Results from Shared Equal Access Regional Cancer Hospital database. Int J Urol. 2015;22(4):362–6.
Atsushi K, Shintaro N, Taketoshi N, Koichiro T, Sohei K, Kazuyuki N, Hiroshi T, Atsushi M, Mingguo H, Mitsuru S. Incidence and location of positive surgical margin among open, laparoscopic and robot-assisted radical prostatectomy in prostate cancer patients: a single institutional analysis. Jpn J Clin Oncol. 2018.
Schröder FH, Hugosson J, Roobol MJ, Tammela TLJ, Auvinen A. Screening and prostate-cancer mortality in a randomized european study. N Engl J Med. 2009;360(13):1320–8.
Baack Kukreja J, Bathala TK, Reichard CA, Troncoso P, Delacroix S, Davies B, Eggener S, Smaldone M, Minhaj Siddiqui M, Tollefson M, et al. Impact of preoperative prostate magnetic resonance imaging on the surgical management of high-risk prostate cancer. Prostate Cancer Prostatic Dis. 2020;23(1):172–8.
Kozikowski M, Zagożdżon B, Gola M, Dobruch J. Prostate imaging reporting and data system in prostate cancer staging and planning for radical prostatectomy. Wideochir Inne Tech Maloinwazyjne. 2019;14(2):262–70.
Lee T, Hoogenes J, Wright I, Matsumoto ED, Shayegan B. Utility of preoperative 3 Tesla pelvic phased-array multiparametric magnetic resonance imaging in prediction of extracapsular extension and seminal vesicle invasion of prostate cancer and its impact on surgical margin status: Experience at a Canadian academic tertiary care centre. Can Urol Assoc J. 2017;11(5):E174-8.
Schiavina R, Bianchi L, Borghesi M, Dababneh H, Chessa F, Pultrone CV, Angiolini A, Gaudiano C, Porreca A, Fiorentino M, et al. MRI displays the prostatic cancer anatomy and improves the bundles management before robot-assisted radical prostatectomy. J Endourol. 2018;32(4):315–21.
Schieda N, Lim CS, Idris M, Lim RS, Morash C, Breau RH, Flood TA, McInnes MDF. MRI assessment of pathological stage and surgical margins in anterior prostate cancer (APC) using subjective and quantitative analysis. J Magn Reson Imaging. 2017;45(5):1296–303.
Silberstein JL, Eastham JA. Significance and management of positive surgical margins at the time of radical prostatectomy. Indian J Urol. 2014;30(4):423–8.
Funding
Tianjin science and technology plan project (19ZXDBSY00050).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors state that there are no potential competing interests in this manuscript.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Consent for publication
All authors agree to publish this article.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, B., Zhou, J., Wu, S. et al. The impact of surgical margin status on prostate cancer-specific mortality after radical prostatectomy: a systematic review and meta-analysis. Clin Transl Oncol 22, 2087–2096 (2020). https://doi.org/10.1007/s12094-020-02358-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-020-02358-y