Abstract
Background
Apart from surgery, the methods of treatment of HNC are radiotherapy (RTH) and/or chemotherapy (CRTH/CHT). One of the most frequent and serious complications of RTH is oral mucositis (OM). There is a strict correlation between the inflammation and the status of hydration. The aim of the study was to evaluate the changes in hydration, occurring in the course of RTH, measured by means of bioelectrical impedance analysis (BIA) and to analyze them in correlation with the intensification of OM in HNC patients.
Patients and methods
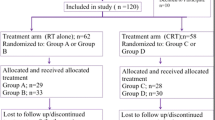
Data from 49 HNC patients (stages I–IV) were analyzed. All of them were irradiated using IMRT technique with the doses of 50–70 Gy. Oral mucositis (OM) was evaluated according to RTOG/EORTC guidelines. BIA was performed using ImpediMed bioimpedance analysis SFB7 BioImp v1.55.
Results
In the fourth week of RTH, 4–5 days before the occurrence of severe OM, it was found that patients with OM grade 3 or higher compared to OM grade 2 or lower had significantly: lower ICW% values (respectively, 53.02% vs 50.72%; p = 0.0047), higher: ECW%: (47.95% vs 46.92%; p = 0.0020), TBW% (respectively, 56.34% vs 51.06%; p = 0.0455), ECW/ICW (respectively, 0.96 vs 0.86; p = 0.0007) and ECW/TBW (respectively, 0.49 vs 0.46, p = 0.0033).
Conclusion
Our study indicates that HNC patients undergo changes in hydration in the course of RTH. We have also confirmed that the intensification of OM leads to ICW decrease and the increase of ECW, TBW as well as ECW/ICW and ECW/TBW values.
Similar content being viewed by others
Background
Head and neck cancer (HNC) is one of the most prevalent malignant epithelial neoplasms in people and the number of newly diagnosed cases of these neoplasms is 650 thousand a year [1].
One of the primary methods of radical HNC treatment is radiotherapy (RTH) used as a standalone therapy or in combination with surgery and/or chemotherapy. One of the most serious complications of RTH is acute radiation reaction in the form of oral mucositis (OM) [2].
OM usually occurs after application of a radiation dose of 10–20 Gy (after 1–2 weeks of RTH) gradually increasing until the completion of RTH [3]. The frequency of occurrence of OM is estimated to be 80–98% in irradiated HNC patients [4,5,6]. Depending on the severity, OM is classified as tolerable (grade 1 and 2 mucositis) and severe (grade 3 or 4), which constitutes a clinical problem [2]. Depending on the RTH scheme and concomitant application of chemotherapy, severe OM is diagnosed in 29–77% patients and is the cause of hospitalization in 16% and discontinuation of treatment in 8–27% patients [4, 6, 7]. OM, especially the severe form, leads to serious eating disorders, dysphagia, dysgeusia, anorexia, pain, and often there is a need for using narcotic analgesics or application of percutaneous endoscopic gastrostomy [2, 4, 5, 8].
Radiation-induced OM develops gradually and in a multi-stage way mainly in result of the activity of reactive oxygen species (ROS), proinflammatory cytokines: TNFα, IL-1β, IL-6 and matrix metalloproteinases (MMPs) as well as change in nuclear factor-κB (NFκB) [2].
There is a close link between the inflammation, including TNFα, IL-6 and MMPs, and the state of hydration [9,10,11]. In studies performed in dialyzed patients, it was determined that the intensification of inflammation is correlated with increased values of extracellular water ECW, ECW/TBW (extracellular water/total body water) indicating the condition of fluid overload [9,10,11].
Current observations indicate that, in the course of irradiation, due to reactions associated with the involvement of proinflammatory cytokines, there may occur changes in the water content in particular spaces. TBW constitutes 73% of fat-free mass (FFM) volume and is present in two spaces as ECW and intracellular water (ICW). ECW includes all body water that exists outside the cell membrane (e.g., interstitial, lymphatic, transcellular fluid and blood) and ICW includes all body water that exists inside the cell membrane [12].
Bioelectrical impedance analysis (BIA) is a useful and precise tool for the evaluation of body composition including hydration, also in cancer patients [13, 14]. BIA facilitates reliable evaluation of such parameters as TBW, ECW and ICW [15,16,17]. It additionally allows for the calculation of ECW/TBW ratio, which is an important and highly sensitive indicator of hydration changes [18].
The hypothesis of our study assumes that in irradiated HNC patients, the OM intensity is strongly correlated with the water distribution status in the respective compartments of the organism.
The aim of the study was to evaluate the changes in hydration, occurring in the course of RTH, measured by means of BIA and to analyze them in correlation with the intensification of OM in HNC patients.
Materials and methods
Patient and clinical data
The study included 49 patients (men) with HNC stage I–IV. Table 1 presents detailed patient characteristics and clinical data. The stage of disease was assessed using the 7th edition of TNM classification (UICC). International Statistical Classification of Diseases and Related Health Problems (ICD) was used to evaluate the level of alcohol consumption. It was classified as either occasional or excessive (F10.1 and F10.2).
Radiotherapy
Intensity-modulated radiotherapy (IMRT) with 6-MV photons was used in the treatment of all patients. The therapy was performed with the frequency of one session a day, five fractions per week. All patients were immobilized in supine position using a customized thermosoftening plastic mask. In the planning phase, CT imaging of the area of interest was conducted using slice thickness of 3 mm. Bolus was not used. Target volumes were delineated according to our institutional treatment protocol, which is compatible with international commission on radiation units and measurements (ICRU) 50 and 62. The entire region of neck nodes (including the lower neck nodes and supraclavicular nodes) was treated with IMRT.
IMRT plans were prepared for all patients using Prowess Panther version 5.20 treatment planning system (Prowes, Inc., Concord, USA). All the plans utilized nine fixed-gantry angle coplanar beams with step-and-shoot treatment techniques on a linear accelerator (Siemens Artiste). The prescribed dose applied to the lower neck and supraclavicular fossa was 50 Gy over 25 fractions for prevention, and 60–66–70 Gy over 30–33–35 fractions for therapy. The acceptance criteria for the treatment plans were the following: (1) 95% of any planning target volume (PTV) was at or above the prescribed dose; (2) 99% of any PTV was at or above 90% of the PTV dose. Doses applied to OAR were established according to the framework of radiation therapy oncology group (RTOG) 0225 protocol. All patients completed the course of radiotherapy with the prescribed dose of IMRT without interruption.
Chemoradiation cisplatin was administered in the dose of 100 mg/m2 on days 1, 22 and 43.
Acute toxicity assessment
RTOG/EORTC scale was used to assess OM intensity. The assessment was conducted once a week for the first 3 weeks of RTH. From the fourth week of RTH, the assessment was performed daily (except for Saturdays and Sundays).
Biochemical examinations and body mass index assessment
Once a week, the following examinations were carried out: total blood count, total protein, albumin level, NA, K, ASPAT, ALAT, bilirubin. Body mass index (BMI) was calculated and classified according to the world health organization (WHO) criteria.
BIA
BIA was performed using ImpediMed bioimpedance analysis SFB7 BioImp v1.55 (Pinkenba Qld 4008, Australia). BIA was conducted while the patients were lying supine on a bed, with their legs apart and their arms not touching the torso. All evaluations were conducted on the patients’ right side using four standard surface electrode (tetra polar) technique on the hand and foot.
Statistical analysis
The collected data were analyzed using MedCalc 15.8 Software (MedCalc Software, Belgium). Continuous variables, such as ECW, ICW, TBW values (as well as percentage values for these parameters); ECW/ICW, ECW/TBW, BMI; and body weight, laboratory parameters, were evaluated using nonparametric test (Mann–Whitney U test). If the same variables of continuous character were evaluated in certain intervals (every week, for seven subsequent weeks before the beginning of each course of radiotherapy), the analysis was conducted using nonparametric test (Wilcoxon). The correlation was evaluated using Spearman rank correlation test. Continuous variables were compared in reference to dichotomous or categorized parameters such as: BMI status and the week of radiotherapy.
Results
The results of our studies demonstrate that in the fourth week of radiotherapy there were significant differences in ICW, ECW and TBW values depending on OM intensity (0–2 and > 3). The differences were observed 4–5 days before the occurrence of OM grade 3.
Significantly lower ICW% values were found in patients with OM grade 3 or higher compared to those, in which OM was classified as grade 2 or lower (respectively, 53.02% vs 50.72%; p = 0.0047; Fig. 1). Significantly lower ICW% values were observed 4 days before the identification of OM grade 3 in patients. In the same, fourth, week of follow-up, significantly lower ECW% values were found in patients with OM grade 3 or higher compared to those, in which OM was classified as grade 2 or lower (respectively, 47.95% vs 46.92%; p = 0.0020; Fig. 1). Significantly higher ECW% values were observed 5 days before the identification of OM grade 3 in patients.
Similar correlation: higher values in patients with OM grade 3 or higher were observed in case of: TBW% parameter (respectively, 56.34% vs 51.06%; p = 0.0455; Fig. 1); indicators: ECW/ICW (respectively, 0.96 vs 0.86; p = 0.0007; Fig. 2) and ECW/TBW (respectively, 0.49 vs 0.46 p = 0.0033; Fig. 2). Significantly higher TBW% values occurred 4 days before the identification of OM grade 3 in patients.
In other weeks of observation, i.e., from first to third and from fifth to seventh, no statistically significant differences in the studied patient hydration parameters depending on the OM grade of advancement were found.
No statistically significant differences were observed in relation to age, fitness level, histopathological finding, stage of disease, neoplasm location, smoking or abuse of alcohol, application of chemotherapy and the levels of selected laboratory parameters: transferrin, prealbumin and total protein, body weight and BMI depending on the intensity of OM in subsequent weeks of follow-up. Only in the case of albumin in the first week of radiotherapy, higher albumin values were observed in patients with OM grade lower than 2 (respectively, 3.46 vs 3.31, p = 0.0331).
No statistically significant differences in the distribution of patient hydration parameter values were observed in relation to such factors as: age, fitness level, histopathological finding, stage of disease, neoplasm location, smoking or abuse of alcohol, application of chemotherapy and the week in which the assessment was made (seven consecutive weeks of radiotherapy).
Discussion
Despite the known risk factors such as older age and male gender, poor oral hygiene, higher total dose of radiation, smoking, systemic disease, more aggressive RTH method and combined radiochemotherapy, no factors have been identified so far that would allow for precise estimation of the risk of occurrence of OM and the degree of its intensity [4].
In our study, we used BIA to assess the state of fluid volume of HNC patients in the course of RTH and we demonstrated that there is a correlation between the hydration and OM intensity.
We demonstrated that, in the course of RTH, there occur changes in the values of ICW, ECW, TBW as well as ECW/ICW and ECW/TBW. We observed that, in the fourth week of radiotherapy, in patients with severe OM (grade 3 or higher) ICW values were lower, while ECW, TBW as well as ECW/ICW and ECW/TBW were significantly higher than in patients with OM grade 0–2.
To our knowledge, this is the first study involving patients subjected to radiotherapy due to HNC, in which the hydration status was evaluated using BIA We are the first to discuss the behavior of hydration in extracellular spaces and we confirmed the existence of strict correlation between hydration and OM intensity. It is also the first study, in which the accurate evaluation of hydration was performed using BIA once a week throughout the duration of RTH (at beginning every week and then almost every day).
The mechanism of action of ionizing radiation is based on cell, tissue and blood vessel damage directly through the activity of reactive oxygen species (ROS) or indirectly through a cascade of reactions with the involvement of proinflammatory cytokines [2]. Immediately after the application of ionizing radiation, there occurs DNA breakage in epithelial cells. This releases ROS which affect other tissues to stimulate transcription factors (NFκB) in subsequent phases [2]. In the next phase, the activated NFκB enhances the production of TNFα, IL-1β, and IL-6, and their activity causes apoptosis and tissue damage. At the same time, DNA breakage and ROS stimulate the production of sphingomyelinase and/or ceramide synthase and, by fibronectin breakup, activate macrophages and MMPs. This leads to further damage of tissues and enhances apoptosis. In the next phase, the so-called amplification, the feedback phenomenon can be observed. The damaged tissues intensify the activity of TNFα, IL-1β, IL-6 and, through caspase and ceramide pathway activation, also MMPs and NFκB, which leads to further tissue damage. In consequence, serious tissue damage occurs including the loss of epithelium integrity [2].
It is well known, inter-alia on the basis of many studies with dialyzed subjects, that there is a strict correlation between the inflammation involving TNFα, IL-1β, IL-6 and MMPs and hydration changes [9,10,11]. In a cross-sectional study, including 159 patients subjected to peritoneal dialysis, Unal et al. [19] demonstrated that in hypervolemic patients compared with euvolemic patients, hs-CRP value levels were significantly higher. The ECW/TBW ratio positively correlated with hs-CRP. While Jacobs et al. [20] observed that serum concentrations of cardiac troponin T, high-sensitive C-reactive protein, brain natriuretic peptide and N-terminal proBNP were significantly correlated, showing a complex link between overhydration, malnutrition, inflammation and cardiac biomarkers in dialyzed patients. In a study involving 99 thousand patients, ECW was significantly higher, while ICW was lower in the group of patients with the presence of medically unexplained symptoms than in group without symptoms, and ECW correlated positively with serum hs-CRP [21].
One of the reasons of occurrence of hydration disturbances in the course of inflammation is the degradation of glycocalyx. Administration of TNFα for 10 min at a constant rate of 4 ng/ml perfusate causes massive destruction of the glycocalyx in isolated animal heart preparations [22]. Also in a prospective cohort study in trauma patients, it was demonstrated that a high level of circulating syndecan-1, a marker of endothelial glycocalyx degradation, was correlated with high levels of IL-6, IL-10 [23]. Glomerular endothelial cell glycocalyx is destroyed by ROS disrupted through a direct mechanism of action without affecting the glycosaminoglycan biosynthetic pathway [24]. Glycocalyx degradation takes place through the action of MMPs activated by proinflammatory cytokines [24]. In a study involving hemodialyzed patients, MMPs and IL6 were significantly linked with ECW/TBW, which confirms the correlation between endothelial injury and fluid overload [25].
The changes in hydration during inflammation also occur through changes in aquaporin function. In an in vitro study performed on human bronchial epithelial cells (BEAS-2B), Mezzasoma et al. [27] demonstrated that, in inflammation, TNFα induced a decrease of atrial natriuretic peptide, natriuretic peptide receptor-1, aquaporin-1 and aquaporin-5 and an increase of brain natriuretic peptide with involvement of different NFκB and mitogen-activated protein kinases signaling pathway activation.
Despite a large quantity of data, the complete pathophysiological mechanism of occurrence of fluid overload in patients with the symptoms of inflammation has not been fully understood [20, 26]. The studies mainly concern dialyzed patients, while there are no studies analyzing the reasons and mechanisms of hydration changes in irradiated patients. Studies on animals only demonstrated that, after the whole-body irradiation using sublethal dose, there occur changes in TBC, EBW, plasma volume, plasma sodium concentration and hemoconcentration [28].
In our study performed in irradiated HNC patients, we observed the development of OM and changes of ECW, ICW and TBW. We also demonstrated a significant correlation between OM and ECW/TBW. It is important because ECW/TBW is an important indicator of hydration [18]. The fluid overload we observed in the study subjects may result from the damage of glycocalyx by TNFα, ROS, MMPs or IL-6 or from aquaporin function disorder. However, the confirmation of these correlations requires further studies.
In the study, we have used BIA, a well-established method of evaluation of the state of nutrition and hydration [13,14,15,16,17]. Although the values of ICW and ECW and ECW/ICW index merely provide information about particular water compartments, the ECW/TBW ratio is regarded as the most important hydration index established by the BIA method [18]. Because ECW/TBW values may be influenced by age and sex [29], the study involved a group of patients uniform in respect to sex and quite uniform in respect of age (median 64 years ± 8).
Our study confirmed that the BIA method is a highly sensitive and specific method of evaluating hydration in HNC patients subjected to RTH. From the clinical point of view, it is important that the BIA method is relatively inexpensive, easily accessible and possible to perform in any hospital.
The limitation of the study was a small number of patients. However, the group was quite homogeneous in terms of sex, age, HNC location, the stage of progression and the treatment method. A big advantage was the fact that BIA examination was carried out several times: at baseline and in each week of RTH.
Our study has demonstrated that statistically significant changes in hydration occur 4–5 days before the manifestation of severe OM. We did not observe any changes in body weight, edemas or other clinical symptoms of fluid overload at that time. The fact that the changes in hydration parameters precede severe OM, which occurs a few days later, has enormous clinical implications. It shows that the application of BIA in daily clinical practice in irradiated HNC patients would facilitate the selection of patients with increased risk of OM and the implementation of treatment before the occurrence of symptoms. Knowing the possible causes of fluid overload, including the damage of glycocalyx, in the future, it may be justified to use medicines with potential glycocalyx protection activity, e.g., polyethylene glycol, adenosine agonists, TNF-A inhibitors, allopurinol, heparin, hyaluronan and glucocorticoids [30].
To sum up, our study has proved that HNC patients undergo changes in hydration in the course of radiotherapy. We have also confirmed that the intensification of OM leads to ICW decrease and the increase of ECW, TBW as well as ECW/ICW and ECW/TBW values.
Additionally, we have demonstrated that changes in hydration occur several days before the clinical manifestation of severe OM. The BIA method applied by us for the first time in a group of HNC patients turned out to be an effective tool for the evaluation of hydration as a predictive factor of severe OM. Further observations are needed to implement the BIA as a diagnostic tool in prediction of severe OM in this group of patients in clinical practice.
References
Siegel RL, Miller KD, Jemal A. A Cancer statistics 2017. CA Cancer J Clin. 2017;67:7–30.
Sonis ST. Oral mucositis in head and neck cancer: risk, biology, and management. Am Soc Clin Oncol Educ Book. 2013. https://doi.org/10.1200/edbook_am.2013.33.e236.
Epstein JB, Schubert MM. Oropharyngeal mucositis in cancer therapy. Oncology. 2003;17(12):1767–76.
Vera-Llonch M, Oster G, Hagiwara M, Sonis S. Oral mucositis in patients undergoing radiation treatment for head and neck carcinoma. Cancer. 2006;106(2):329–36.
Gautam AP, Fernandes DJ, Vidyasagar MS, Maiya AG, Vadhiraja BM. Low level laser therapy for concurrent chemoradiotherapy induced oral mucositis in head and neck cancer patients—a triple blinded randomized controlled trial. Radiother Oncol. 2012;104:349–54.
Trotti A, Bellm LA, Epstein JB, et al. Mucositis incidence, severity and associated outcomes in patients with head and neck cancer receiving radiotherapy with or without chemotherapy: a systematic literature review. Radiother Oncol. 2003;66:253–62.
Traynor AM, Richards GM, Hartig GK, et al. Comprehensive IMRT plus weekly cisplatin for advanced head and neck cancer: the University of Wisconsin experience. Head Neck. 2010;32:599–606.
Al-Othman MO, Amdur RJ, Morris CG, Hinerman RW, Mendenhall WM. Does feeding tube placement predict for long-term swallowing disability after radiotherapy for head and neck cancer? Head Neck. 2003;25(9):741–7.
Vicenté-Martínez M, Martínez-Ramírez L, Muñoz R, et al. Inflammation in patients on peritoneal dialysis is associated with increased extracellular fluid volume. Arch Med Res. 2004;35:220–4.
Avila-Díaz M, Ventura MD, Valle D, et al. Inflammation and extracellular volume expansion are related to sodium and water removal in patients on peritoneal dialysis. Perit Dial Int. 2006;26:574–80.
Demirci MS, Demirci C, Ozdogan O, et al. Relations between malnutrition-inflammation-atherosclerosis and volume status. The usefulness of bioimpedance analysis in peritoneal dialysis patients. Nephrol Dial Transplant. 2011;26(5):1708–16.
Sheng HP, Huggins RA. A review of body composition studies with emphasis on total body water and fat. Am J Clin Nutr. 1979;32(3):630–47.
Simons JP, Schols AM, Westerterp KR, ten Velde GP, Wouters EF. The use of bioelectrical impedance analysis to predict total body water in patients with cancer cachexia. Am J Clin Nutr. 1995;61:741–5.
Małecka-Massalska T, Smolen A, Morshed K. Altered tissue electrical properties in squamous cell carcinoma in head and neck tumors: preliminary observations. Head Neck. 2013;35(8):1101–5.
Kyle UG, Bosaeus I, De Lorenzo AD, et al. Bioelectrical impedance analysis—part I: review of principles and method. Clin Nutr. 2004;23(5):1226–43.
Kyle UG, Bosaeus I, De Lorenzo AD, et al. Bioelectrical impedance analysis—part II: utilization in clinical practice. Clin Nutr. 2004;23(6):1430–53.
Malbrain ML, Huygh J, Dabrowski W, De Waele JJ, Staelens A, Wauters J. The use of bio-electrical impedance analysis (BIA) to guide fluid management, resuscitation and deresuscitation in critically ill patients: a bench-to-bedside review. Anaesthesiol Intensive Ther. 2014;46(5):381–91.
Inal S, Erten Y, Okyay GU, et al. Association between bioimpedance analysis parameters and left ventricular hypertrophy in peritoneal dialysis patients. Int Urol Nephrol. 2014;46(9):1851–6.
Unal A, Kavuncuoglu F, Duran M, et al. Inflammation is associated to volume status in peritoneal dialysis patients. Ren Fail. 2015;37(6):935–40. https://doi.org/10.3109/0886022X.2015.1040337.
Jacobs LH, van de Kerkhof JJ, Mingels AM, et al. Inflammation, overhydration and cardiac biomarkers in haemodialysis patients: a longitudinal study. Nephrol Dial Transplant. 2010;25(1):243–8.
Tsigos C, Stefanaki C, Lambrou GI, Boschiero D, Chrousos GP. Stress and inflammatory biomarkers and symptoms are associated with bioimpedance. Eur J Clin Investig. 2015;45(2):126–34.
Chappell D, Hofmann-Kiefer K, Jacob M, et al. TNF-α induced shedding of the endothelial glycocalyx is prevented by hydrocortisone and antithrombin. Basic Res Cardiol. 2009;104(1):78–89.
Johansson PI, Stensballe J, Rasmussen LS, Ostrowski SR. A high admission syndecan-1 level, a marker of endothelial glycocalyx degradation, is associated with inflammation, protein C depletion, fibrinolysis, and increased mortality in trauma patients. Ann Surg. 2011;254(2):194–200.
Singh A, Ramnath RD, Foster RR, et al. Reactive oxygen species modulate the barrier function of the human glomerular endothelial glycocalyx. PLoS One. 2013;8(2):e55852.
Nugent WH, Mishra N, Strauss JF 3rd, Walsh SW. Matrix metalloproteinase 1 causes vasoconstriction and enhances vessel reactivity to angiotensin II via protease-activated receptor 1. Reprod Sci. 2016;23(4):542–8.
Mitsides N, Cornelis T, Broers NJH, et al. Extracellular overhydration linked with endothelial dysfunction in the context of inflammation in haemodialysis dependent chronic kidney disease. PLoS One. 2017;12(8):e0183281.
Mezzasoma L, Cagini L, Antognelli C, Puma F, Pacifico E, Talesa VN. TNF-α regulates natriuretic peptides and aquaporins in human bronchial epithelial cells BEAS-2B. Mediat Inflamm. 2013;2013:159349.
Geraci JP, Jackson KL, Mariano MS. Fluid and sodium loss in whole-body-irradiated rats. Radiat Res. 1987;111(3):518–32.
Lopot F, Nejedlý B, Novotná H, Macková M, Sulková S. Age-related extracellular to total body water volume ratio (Ecv/TBW)—can it be used for “dry weight” determination in dialysis patients? Application of multifrequency bioimpedance measurement. Int J Artif Organs. 2002;25(8):762–9.
Alphonsus CS, Rodseth RN. The endothelial glycocalyx: a review of the vascular barrier. Anaesthesia. 2014;69(7):777–84.
Funding
No funding was necessary for this project
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The design of the study was accepted by Bioethical Commission at the Medical University in Lublin (KE-0254/232/2014).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Brzozowska, A., Mlak, R., Gołębiowski, P. et al. Status of hydration assessed by bioelectrical impedance analysis: a valuable predictive factor for radiation-induced oral mucositis in head and neck cancer patients. Clin Transl Oncol 21, 615–620 (2019). https://doi.org/10.1007/s12094-018-1963-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-018-1963-8