Abstract
Purpose
Accumulated evidences have reminded us that since the prognosis of retroperitoneal fibrosis (RPF) secondary to non-urology carcinoma is poor it is essential to distinguish this condition from others. The objective of this study is to investigate the clinical features and outcomes of this infrequent but life-threatening disease.
Methods
A total of 97 patients diagnosed with RPF secondary to non-urology carcinoma were enrolled in this retrospective study. The baseline information, history of carcinoma, clinical presentation, laboratory results, diagnosis, treatment and prognosis of the patients were collected and analyzed.
Results
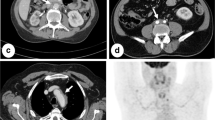
The mean age was 62.32 ± 11.22 years (range 31–85 years). It took 16.72 ± 7.11 days (range 3–34 days) for the patients with originally unexplained hydronephrosis to get a definite diagnosis of RPF secondary to non-urology carcinoma. Imaging-confirmed RPF [confirmed by computed tomography (CT) or magnetic resonance imaging (MRI)] was found in 91 patients. Fifty-seven patients were diagnosed with histological-confirmed malignant RPF. Sixty-six patients received surgical interventions. Cystoscopy and double J tube were performed in 68 cases (102 sides, 172 times) and was failed in 93 times (54.07%). Pyelostomy was performed in 72 patients (92 sides) without a single failure. Furthermore, eighty patients received chemotherapy and/or radiotherapy. The 6-month survival since RPF secondary to non-urology carcinoma was confirmed was 30%.
Conclusions
All patients with newly diagnosed unexplained hydronephrosis should undergo an age-appropriate carcinoma screening. The prognosis of RPF secondary to non-urology carcinoma was dismal. When dealing with hydronephrosis affecting renal function, pyelostomy instead of double J tube catheterization should be performed ahead of time.





Similar content being viewed by others
References
Higgins PM, Bennett-Jones DN, Naish PF, Aber GM. Non-operative management of retroperitoneal fibrosis. Br J Surg. 1988;75(6):573–7.
Kottra JJ, Dunnick NR. Retroperitoneal fibrosis. Radiol Clin N Am. 1996;34(6):1259–75.
Lepor H, Walsh PC, Lepor H, Walsh PC. Idiopathic retroperitoneal fibrosis. J Urol. 1979;122(1):1–6.
van Bommel EF. Retroperitoneal fibrosis. Neth J Med. 2002;60(6):231.
Yokoyama R, Tazaki R, Morita H, Nishitani H, Ariumi S, Osuga S, et al. Retroperitoneal fibrosis in a patient with gastric cancer manifested by lower extremity edema and hydrocele. Intern Med (Tokyo, Jpn). 2012;51(16):2157–60.
Kuhn W, Loos W, Graeff H. Hydronephrosis as the first manifestation of primary metastatic breast cancer. Geburtshilfe Frauenheilkd. 1994;54(5):308–10. https://doi.org/10.1055/s-2007-1022846.
Kane AJ, Wang ZJ, Qayyum A, Yeh BM, Webb EM, Coakley FV. Frequency and etiology of unexplained bilateral hydronephrosis in patients with breast cancer: results of a longitudinal CT study. Clin Imaging. 2012;36(4):263–6. https://doi.org/10.1016/j.clinimag.2011.10.001.
Gilkeson GS, Allen NB. Retroperitoneal fibrosis. A true connective tissue disease. Rheum Dis Clin N Am. 1996;22(1):23.
Stone JR. Aortitis, periaortitis, and retroperitoneal fibrosis, as manifestations of IgG4-related systemic disease. Curr Opin Rheumatol. 2011;23(1):88–94. https://doi.org/10.1097/BOR.0b013e3283412f7c.
Vaglio A, Palmisano A, Alberici F, Maggiore U, Ferretti S, Cobelli R, et al. Prednisone versus tamoxifen in patients with idiopathic retroperitoneal fibrosis: an open-label randomised controlled trial. Lancet (Lond, Engl). 2011;378(9788):338–46. https://doi.org/10.1016/s0140-6736(11)60934-3.
Ormond JK. Bilateral ureteral obstruction due to envelopment and compression by an inflammatory retroperitoneal process. J Urol. 1948;59(6):1072–9.
Vaglio A, Salvarani C, Buzio C. Retroperitoneal fibrosis. Lancet (Lond, Engl). 2006;367(9506):241–51. https://doi.org/10.1016/s0140-6736(06)68035-5.
Thomas MH, Chisholm GD. Retroperitoneal fibrosis associated with malignant disease. Br J Cancer. 1973;28(5):453–8.
Dohmen K, Mizukami Y, Tanaka K, Nakamura H, Arase K, Yokogawa Y, et al. Retroperitoneal fibrosis associated with scirrhous gastric cancer. Gastroenterol Jpn. 1993;28(5):699–705.
Terry MB, Gaudet MM, Gammon MD. The epidemiology of gastric cancer. Semin Radiat Oncol. 2002;12(2):111–27. https://doi.org/10.1053/srao.30814.
Sano T, Sasako M, Yamamoto S, Nashimoto A, Kurita A, Hiratsuka M, et al. Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy—Japan Clinical Oncology Group study 9501. J Clin Oncol. 2004;22(14):2767–73. https://doi.org/10.1200/jco.2004.10.184.
Yashiro M, Chung YS, Nishimura S, Inoue T, Sowa M. Fibrosis in the peritoneum induced by scirrhous gastric cancer cells may act as “soil” for peritoneal dissemination. Cancer. 1996;77(8 Suppl):1668–75. https://doi.org/10.1002/(sici)1097-0142(19960415)77:8%3c1668:aid-cncr37%3e3.0.co;2-w.
Yamauchi S, Nakagawa T, Kasahara M, Sugimoto H, Ishiba T, Tamura N, et al. A case of metastatic breast cancer with bilateral hydronephrosis effectively treated with capecitabine. Gan to kagaku ryoho Cancer & Chemother. 2012;39(12):2077–9.
Urban ML, Palmisano A, Nicastro M, Corradi D, Buzio C, Vaglio A. Idiopathic and secondary forms of retroperitoneal fibrosis: a diagnostic approach. La Revue de medecine interne. 2015;36(1):15–21. https://doi.org/10.1016/j.revmed.2014.10.008.
Chisholm GD, Shackman R. Malignant obstructive uraemia. Br J Urol. 1968;40(6):720–6.
Rose PG, Ali S, Whitney CW, Lanciano R, Stehman FB. Impact of hydronephrosis on outcome of stage IIIB cervical cancer patients with disease limited to the pelvis, treated with radiation and concurrent chemotherapy: a Gynecologic Oncology Group study. Gynecol Oncol. 2010;117(2):270–5. https://doi.org/10.1016/j.ygyno.2010.01.045.
Acknowledgements
We appreciate a grant from Shandong Province Key Research and Development Program (No.2016GGB14312) and a grant from Shandong Province Medicine Heath Science Technology Development Program (No. 2016WS0425) for supporting our study. Besides, we thank Zhao Liu from Department of Urology, Qilu Hospital of Shandong University for proof reading of our manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was conducted in compliance with ethical principles based on the 1964 Declaration of Helsinki and with the approval of the ethics committee of Shandong Provincial Hospital Shandong University.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Rights and permissions
About this article
Cite this article
Chen, T., Tian, L., Fan, D. et al. Retroperitoneal fibrosis secondary to non-urology carcinomas: a clinical and outcome analysis of 97 cases. Clin Transl Oncol 21, 373–379 (2019). https://doi.org/10.1007/s12094-018-1936-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-018-1936-y