Abstract
Purpose
To retrospectively assess outcomes and to identify prognostic factors in patients diagnosed with intermediate-risk (IR) prostate cancer (PCa) treated with primary external beam radiotherapy (EBRT).
Materials and methods
Data were obtained from the multi-institutional Spanish RECAP database, a population-based prostate cancer registry in Spain. All IR patients (NCCN criteria) who underwent primary EBRT were included. The following variables were assessed: age; prostate-specific antigen (PSA); Gleason score; clinical T stage; percentage of positive biopsy cores (PPBC); androgen deprivation therapy (ADT); and radiotherapy dose. The patients were stratified into one of three risk subcategories: (1) favourable IR (FIR; GS 6, ≤ T2b or GS 3 + 4, ≤ T1c), (2) marginal IR (MIR; GS 3 + 4, T2a–b), and (3) unfavourable IR (UIR; GS 4 + 3 or T2c). Biochemical relapse-free survival (BRFS), disease-free survival (DFS), cancer-specific survival (CSS), and overall survival (OS) were assessed.
Results
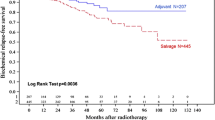
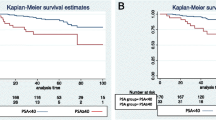
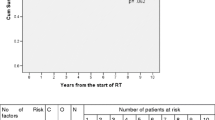
A total of 1754 patients from the RECAP database were included and stratified by risk group: FIR, n = 781 (44.5%); MIR, n = 252 (14.4%); and UIR, n = 721 (41.1%). Mean age was 71 years (range 47–86). Mean PSA was 10.4 ng/ml (range 6–20). The median radiotherapy dose was 74 Gy, with mean doses of 72.5 Gy (FIR), 73.4 Gy (MIR), and 72.8 Gy (UIR). Most patients (88%) received ADT for a median of 7.1 months. By risk group (FIR, MIR, UIR), ADT rates were, respectively, 88.9, 86.5, and 86.9%. Only patients with ≥ 24 months of follow-up post-EBRT were included in the survival analysis (n = 1294). At a median follow-up of 52 months (range 24–173), respective 5- and 10-year outcomes were: OS 93.6% and 79%; BRFS 88.9% and 71.4%; DFS 96.1% and 89%; CSS 98.9% and 94.6%. Complication rates (≥ grade 3) were: acute genitourinary (GU) 2%; late GU 1%; acute gastrointestinal (GI) 2%; late GI 1%. There was no significant association between risk group and BRFS or OS. However, patients with favourable-risk disease had significantly better 5- and 10-year DFS than patients with UIR: 98.7% vs. 92.4% and 92% vs. 85.8% (p = 0.0005). CSS was significantly higher (p = 0.0057) in the FIR group at 5 (99.7% vs. 97.3%) and 10 years (96.1% vs. 93.4%). On the multivariate analyses, the following were significant predictors of survival: ADT (BRFS and DFS); dose ≥ 74 Gy (BRFS); age (OS).
Conclusions
This is the first nationwide study in Spain to report long-term outcomes of patients with intermediate-risk PCa treated with EBRT. Survival outcomes were good, with a low incidence of both acute and late toxicity. Patients with unfavourable risk characteristics had significantly lower 5- and 10-year disease-free survival rates. ADT and radiotherapy dose ≥ 74 Gy were both significant predictors of treatment outcomes.




Similar content being viewed by others
References
Mohler JL, Kantoff PW, Armstrong AJ, Bahnson RR, Cohen M, D’Amico AV, et al. Prostate cancer, version 2.2014. J Natl Compr Cancer Netw. 2014;12:686–718.
Grossfeld GD, Latini DM, Lubeck DP, Mehta SS, Carroll PR. Predicting recurrence after radical prostatectomy for patients with high risk prostate cancer. J Urol. 2003;169:157–63.
D’Amico AV. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280:969. https://doi.org/10.1001/jama.280.11.969.
Zumsteg ZS, Spratt DE, Pei I, Zhang Z, Yamada Y, Kollmeier M, et al. A new risk classification system for therapeutic decision making with intermediate-risk prostate cancer patients undergoing dose-escalated external-beam radiation therapy. Eur Urol. 2013;64:895–902. https://doi.org/10.1016/j.eururo.2013.03.033.
Castle KO, Hoffman KE, Levy LB, Lee AK, Choi S, Nguyen QN, et al. Is androgen deprivation therapy necessary in all intermediate-risk prostate cancer patients treated in the dose escalation era? Int J Radiat Oncol Biol Phys. 2013;85:693–9. https://doi.org/10.1016/j.ijrobp.2012.06.030.
Jung J-W, Lee JK, Hong SK, Byun S-S, Lee SE. Stratification of patients with intermediate-risk prostate cancer. BJU Int. 2015;115:907–12. https://doi.org/10.1111/bju.12703.
Keane FK, Chen M-H, Zhang D, Loffredo MJ, Kantoff PW, Renshaw AA, et al. The likelihood of death from prostate cancer in men with favorable or unfavorable intermediate-risk disease. Cancer. 2014;120:1787–93. https://doi.org/10.1002/cncr.28609.
NCCN (2018) Clinical Practice Guidelines for Prostate Cancer, v. 4. https://www.nccn.org/professionals/physician_gls/default.aspx#prostate.
Sanda MG, Cadeddu JA, Kirkby E, Chen RC, Crispino T, Fontanarosa J, et al. Clinically localized prostate cancer: AUA/ASTRO/SUO guideline. Part I: risk stratification, shared decision making, and care options. J Urol. 2018;199:683–90.
Boladeras A, Martinez E, Ferrer F, Gutierrez C, Villa S, Pera J, et al. Localized prostate cancer treated with external beam radiation therapy: long-term outcomes at a European comprehensive cancer centre. Rep Pract Oncol Radiother. 2016;21:181–7.
Dearnaley DP, Sydes MR, Graham JD, Aird EG, Bottomley D, Cowan RA, et al. Escalated-dose versus standard-dose conformal radiotherapy in prostate cancer: first results from the MRC RT01 randomised controlled trial. Lancet Oncol. 2007;8:475–87.
Zietman AL, Bae K, Slater JD, Shipley WU, Efstathiou JA, Coen JJ, et al. Randomized trial comparing conventional-dose with high-dose conformal radiation therapy in early-stage adenocarcinoma of the prostate: long-term results from proton radiation oncology group/american college of radiology 95-09. J Clin Oncol. 2010;28:1106–11. https://doi.org/10.1200/JCO.2009.25.8475.
Raldow AC, Zhang D, Chen M-H, Braccioforte MH, Moran BJ, D’amico AV. Risk Group and death from prostate cancer implications for active surveillance in men with favorable intermediate-risk prostate cancer. http://www.prostatecancerreports.org/fulltext/2015/Raldow_AC150600.pdf (2017)
Bracci S, Osti MF, Agolli L, Bertaccini L, De Sanctis V, Valeriani M. Different outcomes among favourable and unfavourable intermediate-risk prostate cancer patients treated with hypofractionated radiotherapy and androgen deprivation therapy. Radiat Oncol. 2016;11:78.
Zumsteg ZS, Chen Z, Howard LE, Amling CL, Aronson WJ, Cooperberg MR, et al. Number of unfavorable intermediate-risk factors predicts pathologic upstaging and prostate cancer-specific mortality following radical prostatectomy: results from the SEARCH database. Prostate. 2017;77:154–63.
Zumsteg ZS, Zelefsky MJ. Short-term androgen deprivation therapy for patients with intermediate-risk prostate cancer undergoing dose-escalated radiotherapy: the standard of care? Lancet Oncol. 2012;13:e259–69.
Serrano NA, Fastro MSAF, Anscher MS. Favorable vs unfavorable intermediate-risk prostate cancer: a review of the new classification system and its impact on treatment recommendations. Oncology. 2016;30:1–11.
Zumsteg ZS, Zelefsky MJ, Woo KM, Spratt DE, Kollmeier MA, McBride S, et al. Unification of favourable intermediate-, unfavourable intermediate-, and very high-risk stratification criteria for prostate cancer. BJU Int. 2017;120:E87–95. https://doi.org/10.1111/bju.13903.
Zapatero A, Guerrero A, Maldonado X, Alvarez A, Gonzalez San Segundo C, Cabeza Rodríguez MA, et al. High-dose radiotherapy with short-term or long-term androgen deprivation in localised prostate cancer (DART01/05 GICOR): a randomised, controlled, phase 3 trial. Lancet. Oncol. 2015;16:320–7.
Hamdy FC, Donovan JL, Lane JA, Mason M, Metcalfe C, Holding P, et al. 10 year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med. 2016;375:1415–24. https://doi.org/10.1056/NEJMoa1606220.
Zelefsky MJ, Pei X, Chou JF, Schechter M, Kollmeier M, Cox B, et al. Dose escalation for prostate cancer radiotherapy: predictors of long-term biochemical tumor control and distant metastases-free survival outcomes. Eur Urol. 2011;60:1133–9.
Hjälm-Eriksson M, Ullén A, Johansson H, Levitt S, Nilsson S, Kälkner K-M. Comorbidity as a predictor of overall survival in prostate cancer patients treated with external beam radiotherapy combined with HDR brachytherapy boosts. Acta Oncol. 2017;56:21–6.
Jeldres C, Suardi N, Perrotte P, Capitanio U, Walz J, Hutterer GC, et al. Survival after radical prostatectomy and radiotherapy for prostate cancer: a population-based study. Can Urol Assoc J. 2009;3:13–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors state that they have no relationships, conditions or circumstances that present potential conflicts of interest with this study.
Ethical approval
The retrospective review of medical records was approved by the local ethics committees.
Informed consent
Informed consent was obtained from all live individual participants included in the study.
Rights and permissions
About this article
Cite this article
Hervás, A., Pastor, J., González, C. et al. Outcomes and prognostic factors in intermediate-risk prostate cancer: multi-institutional analysis of the Spanish RECAP database. Clin Transl Oncol 21, 900–909 (2019). https://doi.org/10.1007/s12094-018-02000-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-018-02000-y