Abstract
Objective
To determine the effectiveness of whole-body diffusion-weighted magnetic resonance imaging (WB-DW-MRI) in detecting metastases by comparing the results with those from choline-positron emission tomography-computed tomography (choline-PET/CT) in patients with biochemical relapse after primary treatment, and no metastases in bone scintigraphy, CT and/or pelvic MRI, or metastatic/oligometastatic prostate cancer (PCa). Patients with this disease profile who could benefit from treatment with stereotactic body radiation therapy (SBRT) were selected and their responses to these techniques were rated.
Materials and methods
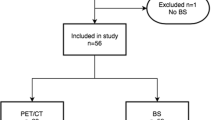
This was a prospective, controlled, unicentric study, involving 46 consecutive patients from our centre who presented biochemical relapse after adjuvant, salvage or radical treatment with external beam radiotherapy, or brachytherapy. After initial tests (bone scintigraphy, CT, pelvic MRI), 35 patients with oligometastases or without them were selected. 11 patients with multiple metastases were excluded from the study. WB-DW-MRI and choline-PET/CT was then performed on each patient within 1 week. The results were interpreted by specialists in nuclear medicine and MRI. If they were candidates for treatment with ablative SBRT (SABR), they were then evaluated every three months with both tests.
Results
Choline-PET/CT detected lesions in 16 patients that were not observable using WB-DW-MRI. The results were consistent in seven patients and in three cases, a lesion was observed using WB-DW-MRI that was not detected with choline-PET/CT. The Kappa value obtained was 0.133 (p = 0.089); the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of WB-DW-MRI were estimated at 44.93, 64.29, 86.11, and 19.15%, respectively. For choline-PET/CT patients, the sensitivity, specificity, PPV, and NPV were 97.10, 58.33, 93.06, and 77.78%, respectively.
Conclusions
Choline-PET/CT has a high global sensitivity while WB-DW-MRI has a high specificity, and so they are complementary techniques. Future studies with more enrolled patients and a longer follow-up period will be required to confirm these data. The initial data show that the best technique for evaluating response after SBRT is choline-PET/CT.
Trial registration number NCT02858128.


Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A. Cancer statistics. CA Cancer J Clin. 2012;62:10–29. doi:10.3322/caac.20138.
Bubendorf L, Schöpfer A, Wagner U, Sauter G, Moch H, Willi N, et al. Metastatic patterns of prostate cancer: an autopsy study of 1,589 patients. Hum Pathol. 2000;31:578–83.
Saad F, Pantel K. The current role of circulating tumor cells in the diagnosis and management of bone metastases in advanced prostate cancer. Future Oncol. 2012;8:321–31. doi:10.2217/fon.12.3.
Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol. 1995;13:8–10.
Niibe Y, Hayakawa K. Oligometastases and oligo-recurrence: the new era of cáncer therapy. Jpn J Clin Oncol. 2010;40:107–11. doi:10.1093/jjco/hyp167.
Gillessen S, Omlin A, Attard G, de Bono JS, Efstathiou E, Fizazi K, et al. Management of patients with advanced prostate cancer: recommendations of the St gallen advanced prostate cancer consensus conference (APCCC) 2015. Ann Oncol. 2015;26:1589–604. doi:10.1093/annonc/mdv257.
Evangelista L, Cimitan M, Zattoni F, Guttilla A, Zattoni F, Saladini G. Comparison between conventional imaging (abdominal–pelvic computed tomography and bone scan) and [18F]choline positron emission tomography/computed tomography imaging for the initial staging of patients with intermediate-tohigh-risk prostate cancer: a retrospective analysis. Scand J Urol. 2015;49:345–53. doi:10.3109/21681805.2015.1005665.
Soyka JD, Muster MA, Schmid DT, Seifert B, Schick U, Miralbell R, et al. Clinical impact of 18F-choline PET/CT in patients with recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2012;39:936–43. doi:10.1007/s00259-012-2083-2.
Abuzallouf S, Dayes I, Lukka H. Baseline staging of newly diagnosed prostate cancer: a summary of the literature. J Urol. 2004;171:2122–7.
Hricak H, Choyke P, Eberhardt SC, Leibel SA, Scardino PT. Imaging prostate cancer: a multidisciplinary perspective. Radiology. 2007;243:28–53.
Cirillo S, Petracchini M, Scotti L, Gallo T, Macera A, Bona MC, et al. Endorectal magnetic resonance imaging at 1.5 tesla to assess local recurrence following radical prostatectomy using T2-weighted and contrast-enhanced imaging. Eur Radiol. 2009;19:761–9. doi:10.1007/s00330-008-1174-8.
Casciani E, Polettini E, Carmenini E, Floriani I, Masselli G, Bertini L, et al. Endorectal and dynamic contrast enhanced MRI for detection of local recurrence after radical prostatectomy. AJR Am J Roentgenol. 2008;190:1187–92. doi:10.2214/AJR.07.3032.
Sciarra A, Panebianco V, Salciccia S, Osimani M, Lisi D, Ciccariello M, et al. Role of dynamic contrast-enhanced magnetic resonance (MR) imaging and proton MR spectroscopic imaging in the detection of local recurrence after radical prostatectomy for prostate cancer. Eur Urol. 2008;54:589–600. doi:10.1016/j.eururo.2007.12.034.
Panebianco V, Barchetti F, Sciarra A, Musio D, Forte V, Gentile V, et al. Prostate cancer recurrence after radical prostatectomy: the role of 3-T diffusion imaging in multiparametric magnetic resonance imaging. Eur Radiol. 2013;23:1745–52. doi:10.1007/s00330-013-2768-3.
Lecouvet FE, Geukens D, Stainier A, Jamar F, Jamart J, d’Othée BJ, et al. Magnetic resonance imaging of the axial skeleton for detecting bone metastases in patients with high-risk prostate cancer: diagnostic and cost-effectiveness and comparison with current detection strategies. J Clin Oncol. 2007;1(25):3281–7.
Kitajima K, Murphy RC, Nathan MA, Froemming AT, Hagen CE, Takahashi N, et al. Detection of recurrent prostate cancer after radical prostatectomy: comparison of 11C-choline better CT with pelvic multiparametric MR imaging with endorectal coil. J Nucl Med. 2014;55:223–32. doi:10.2967/jnumed.113.123018.
Schilling D, Schlemmer HP, Wagner PH, Böttcher P, Merseburger AS, Aschoff P, et al. Histological verification of 11C choline positron emission/computed tomography-positive lymph nodes in patients with biochemical failure after treatment for localized prostate cancer. BJU Int. 2008;102:446–51. doi:10.1111/j.1464-410X.2008.07592.x.
Fortuin A, de Rooij M, Zamecnik P, Haberkorn U, Barentsz J. Molecular and functional imaging for detection of lymph node metastases in prostate cancer. Int J Mol Sci. 2013;14:13842–75. doi:10.3390/ijms140713842.
Rinnab L, Mottaghy FM, Simon J, Volkmer BG, de Petriconi R, Hautmann RE, et al. [11C]Choline PET/CT for targeted salvage lymph node dissection in patients with biochemical recurrence after primary curative therapy for prostate cancer. Preliminary results of a prospective study. Urol Int. 2008;81:191–7. doi:10.1159/000144059.
Scattoni V, Picchio M, Suardi N, Messa C, Freschi M, Roscigno M, et al. Detection of lymph-node metastases with integrated [11C]choline PET/CT in patients with PSA failure after radical retropubic prostatectomy: results confirmed by open pelvic-retroperitoneal lymphadenectomy. Eur Urol. 2007;52:423–9. doi:10.1016/j.eururo.2007.03.032.
Hövels AM, Heesakkers RA, Adang EM, Jager GJ, Strum S, Hoogeveen YL, et al. The diagnostic accuracy of CT and MRI in the staging of pelvic lymph nodes in patients with prostate Cancer: a meta-analysis. Clin Radiol. 2008;63:387–95. doi:10.1016/j.crad.2007.05.022 DOI: 18325358.
Even-Sapir E, Metser U, Mishani E, Lievshitz G, Lerman H, Leibovitch I. The detection of bone metastases in patients with high-risk prostate cancer: 99mTc-MDP Planar bone scintigraphy, single and multi-field-of-view SPECT, 18F-fluoride PET, and 18F-fluoride PET/CT. J Nucl Med. 2006;47:287–97.
Beheshti M, Vali R, Waldenberger P, F Fitz, Nader M, Hammer J, et al. The use of F-18 to be PET in the assessment of bone metastases in prostate cancer: correlation with morphological changes on CT. Mol Imaging Biol. 2009;11:446–54. doi:10.1007/s11307-009-0217-0.
Kitajima K, Murphy RC, Nathan MA. Choline PET/CT for imaging prostate cancer: an update. Ann Nucl Med. 2013;27:581–91. doi:10.1007/s12149-013-0731-7.
Piccardo A, Paparo F, Piccazzo R, Naseri M, Ricci P, Marziano A, et al. Value of fused 18F choline PET/MRI to evaluate prostate cancer relapse in patients showing biochemical recurrence after EBRT: preliminary results. Biomed Res Int. 2014; doi:10.1155/2014/103718.
Rigatti P, Suardi N, Briganti A, Da Pozzo LF, Tutolo M, Villa L, et al. Pelvic/retroperitoneal salvage lymph node dissection for patients treated with radical prostatectomy with biochemical recurrence and nodal recurrence detected by (11C)choline positron emission tomography/computed tomography. Eur Urol. 2011;60:935–43. doi:10.1016/j.eururo.2011.07.060.
Würschmidt F, Petersen C, Wahl A, Dahle J, Kretschmer M. [18F]fluoroethylcholine-PET/CT imaging for radiation treatment planning of recurrent and primary prostate cancer with dose escalation to PET/CT-positive lymph nodes. Radiat Oncol. 2011;6:44. doi:10.1186/1748-717X-6-44.
Picchio M, Berardi G, Fodor A, Busnardo E, Crivellaro C, Giovacchini G, et al. (11)C-choline PET/CT as a guide to radiation treatment planning of lymph-node relapses in prostate cancer patients. Eur J Nucl Med Mol Imaging. 2014;41:1270–9. doi:10.1007/s00259-014-2734-6.
Fisher CG, CP DiPaola, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the spine oncology study group. Spine. 2010;35(22):E1221–9. doi:10.1097/BRS.0b013e3181e16ae2.
Sánchez-Jurado R, Devis M, Sanz R, Aguilar JE, del Puig Cózar M, Ferrer-Rebolleda J. Whole-Body PET/CT studies with lowered 18F-FDG doses: the influence of body mass index in dose reduction. J. Nucl. Med. Technol. 2014;42:62–7. doi:10.2967/jnmt.113.130393.
Phase II Study of SBRTSG 05 as Treatment for Oligometastases in Prostate Cancer. Antonio J Conde Moreno, MD, Hospital Provincial de Castellon. https://clinicaltrials.gov/ct2/show/NCT0219278. Accessed 3 Aug 2016.
Mottet N, Bellmunt J, Briers E, Bolla M, Cornford P, De Santis M, et al. Prostate Cancer-European Association of Urology. https://uroweb.org/wp-content/uploads/EAU-Guidelines-Prostate-Cancer-2016.pdf. Accessed 1 Mar 2016.
Luboldt W, Küfer R, Blumstein N, Toussaint TL, Kluge A, Seemann MD, et al. Prostate carcinoma: diffusion-weighted imaging as potential alternative to conventional MR and 11C-choline PET/CT for detection of bone metastases. Radiology. 2008;249(3):1017–25. doi:10.1148/radiol.2492080038.
Budiharto T, Joniau S, Lerut E, Van den Bergh L, Mottaghy F, Deroose CM, et al. Prospective evaluation of 11C-choline positron emission tomography/computed tomography and diffusion-weighted magnetic resonance imaging for the nodal staging of prostate cancer with a high risk of lymph node metastases. Eur Urol. 2011;60:125–30. doi:10.1016/j.eururo.2011.01.015.
Eiber M, Holzapfel K, Ganter C, Epple K, Metz S, Geinitz H, et al. Whole-body MRI including diffusion-weighted imaging (DWI) for patients with recurring prostate cancer: technical feasibility and assessment of lesion conspicuity in DWI. J Magn Reson Imaging. 2011;33:1160–70. doi:10.1002/jmri.22542.
Shen G, Deng H, Hu S, Jia Z. Comparison of choline-PET/CT, MRI, SPECT, and bone scintigraphy in the diagnosis of bone metastases in patients with prostate Cancer: a meta-analysis. Skeletal Radiol. 2014;43:1503–13. doi:10.1007/s00256-014-1903-9.
Jr Garzon Garcia, Riera E, Valls E, Soler M, Bassa P, Moragas M, et al. 18F-fluoride PET/CT in a patient with discordant bone scintigraphy and 11C-choline PET/CT. Clin Nucl Med. 2013;38(2):120–4. doi:10.1097/RLU.0b013e31827a20d3.
Pasqualetti F, Panichi M, Sainato A, Matteucci F, Galli L, Cocuzza P, et al. [18F]Choline PET/CT and stereotactic body radiotherapy on treatment decision making of oligometastatic prostate cancer patients: preliminary results. Radiat Oncol. 2016;11:9. doi:10.1186/s13014-016-0586-x.
Ost P, Jereczek-Fossa BA, As NV, Zilli T, Muacevic A, Olivier K, et al. Progression-free survival following stereotactic body radiotherapy for oligometastatic prostate cancer treatment-naive recurrence: a multi-institutional analysis. Eur Urol. 2016;69:9–12. doi:10.1016/j.eururo.2015.07.004.
Afshar-Oromieh A, Zechmann CM, Malcher A, Eder M, Eisenhut M, Linhart HG, et al. Comparison of PET imaging with a (68)Ga-labelled PSMA ligand and (18)F-choline-based PET/CT for the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2014;41:11–20. doi:10.1007/s00259-013-2525-5.
Morigi JJ, Stricker PD, van Leeuwen PJ, Tang R, Ho B, Nguyen Q, et al. Prospective comparison of 18F-fluoromethylcholine versus 68 Ga-PSMA PET/CT in prostate cancer patients who have rising PSA after curative treatment and are being considered for targeted therapy. J Nucl Med. 2015;56:1185–90. doi:10.2967/jnumed.115.160382.
Maurer, T. et al. PET imaging with 68Gallium-labelled ligand of prostate-specific membrane antigen (68Ga-HBED-PSMA) for staging of biochemical recurrent prostate cancer after radical prostatectomy. J Clin Oncol. 2015;33(15_suppl):5023.
Maurer, T. et al. PET imaging with of prostate-specific membrane antigen (PSMA) for staging of primary prostate cancer with 68Ga-HBED-PSMA. J Clin Oncol. 2015;33(suppl):e16038.
Ost P, Decaestecker K, Lambert B, Fonteyne V, Delrue L, Lumen N, et al. Prognostic factors influencing prostate cancer-specific survival in non-castrate patients with metastatic prostate cancer. Prostate. 2014;74:297–305. doi:10.1002/pros.22750.
Ferrer Albiach C, Conde Moreno AJ, Albert Antequera M, et al. Bioclínic retrospective observational study of profiling of mRNAs in patients with cancer próstate oligo-metastases and oligorecurrence. Radiotherapy Oncology Hospital Provincial de Castellón (EudraCT number: 2015-005620-26).
GAP6-Oligometastatic prostate cancer. https://gap6.fluidreview.com. Accessed 22 Jan 2016.
Acknowledgements
The authors wish to thank the Provincial Hospital of Castellón Foundation for their assistance in the development of this manuscript and the Eresa Foundation for the grant that has allowed to fund this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Declarations
This study was approved by our internal institutional review board, and written informed consent with guarantees of confidentiality was obtained from all human participants.
Consent for publication
We declare that we have obtained consent to publish from the patients to report patients data.
Availability of data and materials
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
Funding
This study has been made possible thanks to the funds granted prior public call for research proposals of the Eresa Foundation. Award Number: BF13004. Grant recipient: Antonio José Conde Moreno M.D. Ph.D. The role of the funding was the cost of the explorations and the costs of statistical analysis.
Conflict of interest
None of the authors have any competing interests in the manuscript.
Rights and permissions
About this article
Cite this article
Conde-Moreno, A.J., Herrando-Parreño, G., Muelas-Soria, R. et al. Whole-body diffusion-weighted magnetic resonance imaging (WB-DW-MRI) vs choline-positron emission tomography-computed tomography (choline-PET/CT) for selecting treatments in recurrent prostate cancer. Clin Transl Oncol 19, 553–561 (2017). https://doi.org/10.1007/s12094-016-1563-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-016-1563-4