Abstract
Objective
To observe the dynamic changes of blood perfusion and hypoxic status with CT perfusion imaging and hypoxia imaging in patients of non-small-cell lung cancer (NSCLC) who were treated with recombinant human endostatin (RHES).
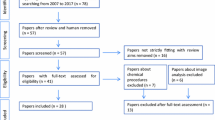
Methods
Fifteen previously untreated patients with histologically or cytologically confirmed NSCLC were enrolled. They were randomly divided into research group (n=10) and negative control group (n=5). The patients of the research group continuously used RHES for ten days, and simultaneously had CT perfusion imaging and hypoxia imaging performed on days 1, 5 and 10, respectively. The remaining 5(control) only had CT perfusion imaging and hypoxia imaging, without using RHES, on days 1, 5 and 10, respectively. According to the above results, we could obtain a “time window” during which RHES improves blood perfusion and hypoxia of lung cancer.
Results
In the research group, after using RHES, capillary permeability surface (PS) and tumour to normal tissue (T/N) decreased at first, and then increased. Their lowest points occurred on about the fifth day with statistical significance compared with the first day (T/N, p=0.00; PS, p<0.01). Blood flow (BF) was first increased and then decreased. Its highest point occurred on about the fifth day with statistical significance compared with the first and tenth day (all p<0.01). The PS, BF and T/N peaked on the fifth day in the research group with statistical significance compared with the negative control group as well (all p<0.01). The above results suggested that RHES’s “time window” was within about one week after administration.
Conclusion
RHES’s “time window” is within about one week after administration, which provides an important experimental basis for combining RHES with radiotherapy in human tumours.
Similar content being viewed by others
References
Wu DS, Wu CM, Huang TH, Xie QD (2008) Combined effects of radiotherapy and endostatin gene therapy in melanoma tumor model. Radiat Environ Biophys 47:285–291
Dings RP, Loren M, Heun H et al (2007) Scheduling of radiation with angiogenesis inhibitors anginex and Avastin improves therapeutic outcome via vessel normalization. Clin Cancer Res 13:3395–3402
Peng F, Wang J, Zou Y et al (2011) Recombinant human endostatin improves tumor vasculature and alleviates hypoxia in Lewis lung carcinoma. Chin J Radiat Oncol 20:69–72
Folkman J (1971) Tumor angiogenesis therapeutic implications. N Engl J Med 285: 1182–1186
Folkman J (1996) Tumor angiogenesis and tissue factor. Nat Med 2:209–215
Folkman J (1995) Angiogenesis in cancer vascular rheumatoid and other disease. Nat Med 1:27–31
Folkman J (2002) Role of angiogenesis in tumor growth and metastasis. Semin Oncol 29[6 Suppl 16]:15–18
O’Reilly MS, Boehm T, Shing Y et al (1997) Endostatin: an endogenous inhibitor of angiogenesis and tumor growth. Cell 88:277–285
Wang J-W, Sun Y, Liu Y-Y et al (2005) Results of randomized, multicenter, double-blind phase III trial of rh-endostatin (YH-16) in treatment of advanced non-small cell lung cancer patients. Chin J Oncol 8:283–290
Ling CH, Ji C, Chen YB et al (2004) Combined effects of endostatin gene transfer and ionizing radiation on lung adenocarcinoma model of A549 cells. Chin J Tuberc Respir Dis 27:683–686
Luo X, Andres ML, Timiryasova TM et al (2005) Radiation-enhanced endostatin gene expression and effects of combination treatment. Technol Cancer Res Treat 4:193–202
Jain RK (2005) Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science 307:58–62
Winkler F, Kozin SV, Tong RT et al (2004) Kinetics of vascular normalization by VEGFR2 blockade governs brain tumor response to radiation: role of oxygenation. Angiopoietin-1, and matrix metalloproteinases. Cancer Cell 6:553–563
Huang G, Chen L (2010) Recombinant human endostatin improves anti-tumor efficacy of paclitaxel by normalizing tumor vasculature in Lewis lung carcinoma. J Cancer Res Clin Oncol 136:1201–1211
Jiang X-D, Dai P, Wu J et al (2011) The inhibitory effects of radiotherapy combined with weekly dosage endostain on the growth of transplanted human lung cancer cell line A549 in nude mice. Lung Cancer 72:165–171
Batchelor TT, Sorensen AG, di Tomaso E et al (2007) AZD2171, a pan-VEGF receptor tyrosine kinase inhibitor, normalizes tumor vasculature and alleviates edema in glioblastoma patients. Cancer Cell 11:83–95
Author information
Authors and Affiliations
Corresponding author
Additional information
These authors contributed equally to this work
Rights and permissions
About this article
Cite this article
Jiang, XD., Dai, P., Qiao, Y. et al. Clinical study on the recombinant human endostatin regarding improving the blood perfusion and hypoxia of non-small-cell lung cancer. Clin Transl Oncol 14, 437–443 (2012). https://doi.org/10.1007/s12094-012-0821-3
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s12094-012-0821-3