Abstract
Background and purpose
A previous study of cancer-related neuropathic pain (NP) found that a 10-fold increase in pregabalin (PGB) use increased patients’ satisfaction with treatment. Further research of PGB vs. non-pregabalin (non-PGB) treatment was carried out to assess if the use of more specific NP-targeting drugs, such as PGB, in combined therapy, in patients with cancer-related NP, provides better health outcomes.
Patients and methods
Post hoc analysis of PGB-vs. non-PGB-treated patients in a 2-month epidemiological, prospective, multicentre study to assess NP prevalence and management in cancer pain patients visiting radiotherapy oncologic units. Patients undertook the Brief Pain Inventory (BPI), Hospital Anxiety and Depression Scale (HADS), the Medical Outcomes Sleep Scale (MOS-Sleep) and the short form (SF-12) Health Survey.
Results
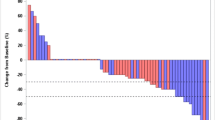
A total of 273 patients with no previous PGB treatment: 162 were treated with PGB polytherapy and 111 with other treatments. At 8 weeks, satisfaction with treatment was 92.6% (PGB) vs. 78.9% (non-PGB), p=0.0024, and benzodiazepine use 37.8% (non-PGB) vs. 19.8% (PGB), p=0.0009. The decreases in BPI total pain intensity and total interference with activities and in MOS overall sleep problems index were signifi cantly larger in the PGB group.
Conclusions
The addition of more specifi c NP-targeting drugs to usual treatment, such as PGB, in NP cancer patients provides more satisfaction with treatment and better outcomes in terms of pain intensity, interference with activities and sleep than treatments without specific NP-targeting drugs. Anxiolytic profile of PGB could allow for less use of benzodiazepines.
Similar content being viewed by others
References
IASP (1994) Part III: pain terms, a current list with definitions and notes on usage. In: Classification of chronic pain, 2nd edition. IASP Press, Seattle, pp 209–213
Chang VT, Janjan N, Jain S, Chau C (2006) Update in cancer pain syndromes. J Palliat Med 9:1414–1434
Caraceni A, Portenoy RK (1999) An international survey of cancer pain characteristics and syndromes. IASP task force on cancer pain. International Association for the Study of Pain. Pain 82:263–274
Stute P, Soukup J, Menzel M et al (2003) Analysis and treatment of different types of neuropathic cancer pain. J Pain Symptom Manage 26:1123–1131
Burton AW, Fanciullo GJ, Beasley RD, Fisch MJ (2007) Chronic pain in the cancer survivor: a new frontier. Pain Med 8:189–198
Twycross R, Harcourt J, Bergl S (1996) A survey of pain in patients with advanced cancer. J Pain Symptom Manage 12:273–282
Fan G, Hadi S, Chow E (2007) Symptom clusters in patients with advanced-stage cancer referred for palliative radiation therapy in an outpatient setting. Support Cancer Ther 4:157–162
Walsh D, Rybicki L (2006) Symptom clustering in advanced cancer. Support Care Cancer 14:831–836
Horowitz SH (2007) The diagnostic workup of patients with neuropathic pain. Med Clin North Am 91:21–30
Stacey BR (2005) Management of peripheral neuropathic pain. Am J Phys Med Rehab 84:S4–16
Sun V, Borneman T, Piper B et al (2008) Barriers to pain assessment and management in cancer survivorship. J Cancer Surviv 2:65–71
Sinnott C (2002) Problems recruiting cancer patients to a comparative clinical trial of drug treatments for neuropathic pain in palliative care. J Pain Symptom Manage 23:270–272
Backonja MM, Serra J (2004) Pharmacologic management part 1: better-studied neuropathic pain diseases. Pain Med 5[Suppl 1]:S28–47
Portenoy RK, Foley KM, Inturrisi CE (1990) The nature of opioid responsiveness and its implications for neuropathic pain: new hypotheses derived from studies of opioid infusions. Pain 43:273–286
Mercadante S, Gebbia V, David F et al (2009) Tools for identifying cancer pain of predominantly neuropathic origin and opioid responsiveness in cancer patients. J Pain 10:594–600
Levy MH, Chwistek M, Mehta RS (2008) Management of chronic pain in cancer survivors. Cancer J 14:401–409
Montero Homs J, Gutierrez-Rivas E, Pardo Fernandez J, Navarro Darder C (2005) [Epidemiological study of prevalence, incidence and neuropathic pain characterization in neurology units. Prevadol study]. Neurologia 20:385–389
Perez C, Saldana MT, Navarro A et al (2009) Prevalence and characterization of neuropathic pain in a primary-care setting in Spain: a crosssectional, multicentre, observational study. Clin Drug Investig 29:441–450
Obermann M, Yoon MS, Sensen K et al (2008) Effi cacy of pregabalin in the treatment of trigeminal neuralgia. Cephalalgia 28:174–181
Zareba G (2005) Pregabalin: a new agent for the treatment of neuropathic pain. Drugs Today (Barc) 41:509–516
Sommer M, Bachmann CG, Liebetanz KM et al (2007) Pregabalin in restless legs syndrome with and without neuropathic pain. Acta Neurol Scand 115:347–350
Finnerup NB, Jensen TS (2007) Clinical use of pregabalin in the management of central neuropathic pain. Neuropsychiatr Dis Treat 3:885–891
Pohl RB, Feltner DE, Fieve RR, Pande AC (2005) Efficacy of pregabalin in the treatment of generalized anxiety disorder: double-blind, placebo-controlled comparison of bid versus tid dosing. J Clin Psychopharmacol 25:151–158
Sabatowski R, Galvez R, Cherry DA et al (2004) Pregabalin reduces pain and improves sleep and mood disturbances in patients with post-herpetic neuralgia: results of a randomised, placebo-controlled clinical trial. Pain 109:26–35
Pae CU (2009) Pregabalin augmentation to antidepressants in patients with major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry 33:577–578
Fairchild A, Chow E (2007) Role of radiation therapy and radiopharmaceuticals in bone metastases. Curr Opin Support Palliat Care 1:169–173
Chow E (2007) Update on radiation treatment for cancer pain. Curr Opin Support Palliat Care 1:11–15
Mañas A, Monroy JL, Ramos AA et al (2010) Prevalence of neuropathic pain in radiotherapy oncology units. Int J Radiat Oncol Biol Phys [Epub ahead of print]
Bouhassira D, Attal N, Alchaar H et al (2005) Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (dn4). Pain 114:29–36
Badia X, Muriel C, Gracia A et al (2003) [Validation of the Spanish version of the brief pain inventory in patients with oncological pain]. Med Clin (Barc) 120:52–59
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Rejas J, Ribera MV, Ruiz M, Masrramon X (2007) Psychometric properties of the MOS (Medical Outcomes Study) sleep scale in patients with neuropathic pain. Eur J Pain 11:329–340
Badia X, Salamero M, Alonso J (2002) La medida de la salud. Guía de escalas de medición en español. In: Edimac con Fundación Lilly, Barcelona
Saif MW, Hashmi S (2008) Successful amelioration of oxaliplatin-induced hyperexcitability syndrome with the antiepileptic pregabalin in a patient with pancreatic cancer. Cancer Chemother Pharmacol 61:349–354
Ravnefjord A, Brusberg M, Larsson H et al (2008) Effects of pregabalin on visceral pain responses and colonic compliance in rats. Br J Pharmacol 155:407–416
Ling B, Coudore F, Decalonne L et al (2008) Comparative antiallodynic activity of morphine, pregabalin and lidocaine in a rat model of neuropathic pain produced by one oxaliplatin injection. Neuropharmacology 55:724–728
Chiechio S, Zammataro M, Caraci F et al (2009) Pregabalin in the treatment of chronic pain: an overview. Clin Drug Investig 29:203–213
Cloos JM, d'Ferreira V (2009) Current use of benzodiazepines in anxiety disorders. Curr Opin Psychiatry 22:90–95
Hidalgo RB, Tupler LA, Davidson JR (2007) An effect-size analysis of pharmacologic treatments for generalized anxiety disorder. J Psychopharmacol 21:864–872
Twycross R (1994) The risks and benefi ts of corticosteroids in advanced cancer. Drug Saf 11:163–178
Gibbs M (2009) The role of transdermal fentanyl patches in the effective management of cancer pain. Int J Palliat Nurs 15:354–359
Radbruch L, Elsner F (2004) Clinical experience with transdermal fentanyl for the treatment of cancer pain in germany. Keio J Med 53:23–29
Kim SW, Shin IS, Kim JM et al (2008) Effectiveness of mirtazapine for nausea and insomnia in cancer patients with depression. Psychiatry Clin Neurosci 62:75–83
Theobald DE, Kirsh KL, Holtsclaw E et al (2002) An open-label, crossover trial of mirtazapine (15 and 30 mg) in cancer patients with pain and other distressing symptoms. J Pain Symptom Manage 23:442–447
Cankurtaran ES, Ozalp E, Soygur H et al (2008) Mirtazapine improves sleep and lowers anxiety and depression in cancer patients: superiority over imipramine. Support Care Cancer 16:1291–1298
Freynhagen R, Grond S, Schupfer G et al (2007) Efficacy and safety of pregabalin in treatment refractory patients with various neuropathic pain entities in clinical routine. Int J Clin Pract 61:1989–1996
Hays RD, Martin SA, Sesti AM, Spritzer KL (2005) Psychometric properties of the medical outcomes study sleep measure. Sleep Med 6:41–44
Hindmarch I, Dawson J, Stanley N (2005) A double-blind study in healthy volunteers to assess the effects on sleep of pregabalin compared with alprazolam and placebo. Sleep 28:187–193
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mañas, A., Ciria, J.P., Fernández, M.C. et al. Post hoc analysis of pregabalin vs. non-pregabalin treatment in patients with cancer-related neuropathic pain: better pain relief, sleep and physical health. Clin Transl Oncol 13, 656–663 (2011). https://doi.org/10.1007/s12094-011-0711-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-011-0711-0