Abstract
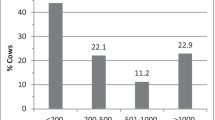
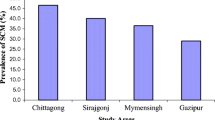
Subclinical mastitis (SCM) represents a major proportion of the burden of mastitis. Determining somatic cell count (SCC) and electrical conductivity (EC) of milk are useful approaches to detect SCM. In order to correlate grades of SCM with the load of five major mastitis pathogens, 246 milk samples from a handful of organized and unorganized sectors were screened. SCC (>5 × 105/mL) and EC (>6.5 mS/cm) identified 110 (45 %) and 153 (62 %) samples, respectively, to be from SCM cases. Randomly selected SCM-negative samples as well as 186 samples positive by either SCC or EC were then evaluated for isolation of five major mastitis-associated bacteria. Of the 323 isolates obtained, 95 each were S. aureus and coagulase-negative staphylococci (CoNS), 48 were E. coli and 85 were streptococci. There was no association between the distribution of organisms and (a) the different groups of SCC, or (b) organised farms and unorganised sectors. By contrast, there was a significant difference in the distribution of CoNS, and not other species, between organized farms and unorganized sectors. In summary, bacteria were isolated irrespective of the density of somatic cells or the type of farm setting, and the frequency of isolation of CoNS was higher with organized farms. These results suggest the requirement for fine tuning SCC and EC limits and the higher probability for CoNS to be associated with SCM in organized diary sectors, and have implications for the identification, management and control of mastitis in India.


Similar content being viewed by others
References
Wilson DJ, Gonzales RN, Das HH (1997) Bovine mastitis pathogens in New York and effects on somatic cell count and milk production. J Dairy Sci 80:2592–2598
Oliver SP, Calvinho LF (1995) Influence of inflammation on mammary gland metabolism and milk composition. J Anim Sci 73:18–33
Singh PJ, Singh PB (1994) A study of economic losses due to mastitis in India. Ind J Dairy Sci 47:265–272
Bansal BK, Gupta DK (2009) Economic analysis of bovine mastitis in India and Punjab. Ind J Dairy Sci 62:337–345
Hayakawa Y, Akagi M, Hayashi M, Shimango T, Komae H, Funaki O, Kaidoh T, Takeuchi S (2000) Antibody response to toxic shock syndrome toxin-1 of Staphylococcus aureus in dairy cows. Vet Microbiol 72:321–327
Pyorala S (2003) Indicators of inflammation in the diagnosis of mastitis. Vet Res 34:565–578
Sharma N, Singh NK, Bhadwal MS (2011) Relationship of somatic cell count and mastitis: an overview. Asian-Australas J Anim Sci 24:429–438
Mitra M, Ghosh D, Ali K, Guha C, Pramanic AK (1995) Prevalence of subclinical mastitis in an organized buffalo farm at Haringhata. Ind Vet J 72:1310–1311
Mallikarjunaswamy MC, Krishnamurthy GV (1997) Antibiogram of bacterial pathogens isolated from bovine subclinical mastitis cases. Ind Vet J 74:885–886
Datta S, Rangnekar A (2001) Subclinical mastitis in a Jersey herd. Ind Vet J 78:161–162
Kumari MP, Ramgupta JB (2002) Diagnosis and therapy of subclinical mastitis in post parturient cows. Ind Vet J 79:89
Rajeev NK, Isloor S, Rathnamma D, Shridhar NB (2009) Characterization of Staphylococcus aureus and E. coli of bovine mastitis. Ind Vet J 86:883–885
Collee JG, Miles RS, Watt B (2008) Tests for identification of bacteria. In: Collee JG, Fraser AG, Marmion BP, Simmons A (eds) Mackie and McCartney Practical Medical Microbiology. Churchill Livingstone, London
Anonymous (1971) A monograph on bovine mastitis. In: International Dairy Federation Bulletin, Brussels, Belgium
Paape MJ, Contreras A (1997) Historical perspective on the evaluation of the milk somatic cell count. Flem Vet J Suppl 66:93–105
Sargeant JM, Leslie KE, Shirley JE, Pulkrabek JL, Liim GH (2001) Sensitivity and specificity of somatic cell count and California mastitis test for identifying intramammary infection in early lactation. J Dairy Sci 84:2018–2024
Mansell PD, Seguya A (2003) The use of a hand-held conductivity meter for the diagnosis of subclinical mastitis in dairy cows during late lactation. New Zealand Vet J 51:21–25
Hamann J, Nipp B, Zecconi A (1998) Evaluation of the electrical conductivity of milk as a mastitis indicator. In: International Dairy Federation Bulletin, Brussels, Belgium
Jensen NE, Knudsen K (1991) Inter-quarter comparison of markers of subclinical mastitis: somatic cell count, electrical conductivity, N-acetyl-D-glucosaminidase and antitrypsin. J Dairy Res 58:389–399
Botrel MA, Haenni M, Morignat E, Madec JY, Calavas D (2010) Distribution and antimicrobial resistance of clinical and subclinical mastitis pathogens in dairy cows in Rhône-Alpes, France. Foodborne Pathog Dis 7:479–487
Schukken YH, Grommers FJ, van de Geer D, Brand A, van degeer D (1989) Incidence of clinical mastitis on farms with low somatic cell counts in bulk milk. Vet Rec 125:60–63
Bhatt VD, Ahir VB, Koringa PG, Jakhesara SJ, Rank DN, Nauriyal DS, Kunjadi AP, Joshi CG (2012) Milk microbiome signatures of subclinical mastitis-affected cattle analysed by shotgun sequencing. J Appl Microbiol 112:639–650
Odierno L, Calvinho L, Traverssa P, Lasagno M, Bogni C, Reinoso E (2006) Conventional identification of Streptococcus uberis isolated from bovine mastitis in Argentinean dairy herds. J Dairy Sci 89:3886–3890
Gonano M, Winter P (2008) Phenotypic and molecular identification of Streptococcal species isolated from milk of intra mammary infected Dairy cows in Austria. In: Proceedings of international conference on Mastitis control: from science to practice, September 30th–2nd October 2008, The Hague, Netherlands
Khan IU, Hassan AA, Abdulmawjood A, Lammler C, Wolter W, Zschock M (2003) Identification and epidemiological characterization of Streptococcus uberis isolated from bovine mastitis using conventional and molecular methods. J Vet Sci 4:213–224
King JS (1981) Streptococcus uberis: a review of its role as a causative organism of bovine mastitis. Br Vet J 137:160–165
Calvinho LF, Vitulich CA, Zurbriggen MA, Canavesio VR, Tarabla HD (1991) Prevalencia de microorganismos patogenos de la ubre en rodeos de la cuenca lechera santafesina. [Prevalence of microorganisms as udder pathogens in the dairy herds of Santa Fe]. Therios 18:189–196
Thoerberg BM (2008) Coagulase negative staphylococci in bovine subclinical mastitis. Master’s Thesis, Swedish University of Agricultural Sciences, Uppsala, Sweden
Euzeby JP (2008) List of prokaryotic names with standing in nomenclature. http://www.bacterio.cict.fr/. Accessed 8 July 2012
Lim GH, Leslie KE, Kelton DF, Duffield TF, Timms LL, Dingwell RT (2007) Adherence and efficacy of an external sealant to prevent new intramammary infections in the dry period. J Dairy Sci 90:1289–1300
Taponen S (2008) Bovine mastitis caused by coagulase negative staphylococci. Dissertation, University of Helsinki, Finland
Tenhagen BA, Koster G, Wallman J, Henwieser W (2006) Pathogens and their resistance against antimicrobial agents in dairy cows in Brandenburg, Germany. J Dairy Sci 89:2542–2551
Pitkala A, Haveri M, Pyorala S, Myllys V, Buzalski HT (2004) Bovine mastitis in Finland 2001-prevalence, distribution of bacteria, and antimicrobial resistance. J Dairy Sci 87:2433–2441
Trinidad P, Nickerson SC, Adkinson RW (1990) Histopathology of Staphylococcal mastitis in inbred dairy heifers. J Dairy Sci 73:639–647
Acknowledgments
This work was funded by the Indian Council of Agricultural Research under the National Agriculture Innovation Projects Scheme. We thank Avinash Bhat, Dept. of Pharmacology, Veterinary College, Bengaluru, for assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hegde, R., Isloor, S., Prabhu, K.N. et al. Incidence of Subclinical Mastitis and Prevalence of Major Mastitis Pathogens in Organized Farms and Unorganized Sectors. Indian J Microbiol 53, 315–320 (2013). https://doi.org/10.1007/s12088-012-0336-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12088-012-0336-1