Abstract
Background and aims
Metabolic dysfunction-associated fatty liver disease (MAFLD) establishes new criteria for diagnosis of fatty liver disease independent of alcohol intake. We aimed to describe the prevalence and compare characteristics and mortality outcomes of persons with nonobese and obese MAFLD.
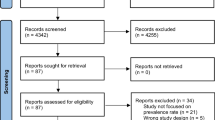
Methods
Using data from 13,640 participants from the third National Health and Nutrition Examination Survey (NHANES III) 1988–1994, we identified participants with fatty liver on ultrasound who had MAFLD and analyzed them by the presence of obesity.
Results
Overall prevalence of MAFLD was 19%; amongst those, 54% were obese and 46% were nonobese. Nonobese MAFLD was more common in participants older than 65 than in younger participants (56.8% vs. 43.2%, p < 0.0001). Nonobese MAFLD was more common in males (63.2% vs. 48.3%, p < 0.0001). Obese MAFLD was more common in females (51.7% vs. 48.3%, p < 0.0001). After adjusting for several demographic factors and alcohol use, older age [adjusted odds ratio (aOR) 1.02, 95% CI 1.00–1.02, p = 0.003] and being male (aOR: 1.65, 95% CI 1.25–2.17, p = 0.001) were independent risk factors for nonobese MAFLD. Nonobese MAFLD participants had a higher 20-year cumulative incidence for all-cause mortality compared to obese MAFLD participants (33.2% vs. 28.8%, p = 0.0137). However, nonobese MAFLD was not independently associated with mortality after adjusting for relevant confounders, while FIB-4 > 1.3 and cardiovascular disease were the strongest risk factors associated with increased mortality [adjusted hazard ratio (aHR) > 2.7 for both, p < 0.0001 for both].
Conclusions
Nonobese MAFLD constitutes about half of the MAFLD in the United States, especially among males and the elderly. Notably, nonobese MAFLD carries higher mortality than obese MAFLD. Screening and diagnosis of MAFLD should be considered in nonobese populations.




Similar content being viewed by others
Abbreviations
- aHR:
-
Adjusted hazard ratio
- aOR:
-
Adjusted odds ratio
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate aminotransferase
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- FIB-4:
-
Fibrosis-4
- GGT:
-
Gamma-glutamyl transferase
- HBA1C:
-
Hemoglobin A1C
- HDL-C:
-
High-density lipoprotein cholesterol
- HOMA-IR:
-
Homeostatic model assessment of insulin resistance
- LDL-C:
-
Low-density lipoprotein cholesterol
- MAFLD:
-
Metabolic dysfunction-associated fatty liver disease
- MetS:
-
Metabolic syndrome
- NAFLD:
-
Nonalcoholic fatty liver disease
- NHANES:
-
National Health and Nutrition Examination Survey
- T2DM:
-
Type 2 diabetes mellitus
References
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84
Le MH, Devaki P, Ha NB, et al. Prevalence of non-alcoholic fatty liver disease and risk factors for advanced fibrosis and mortality in the United States. PLoS ONE. 2017;12(3): e0173499
Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15(1):11–20
Zou B, Yeo YH, Nguyen VH, Cheung R, Ingelsson E, Nguyen MH. Prevalence, characteristics and mortality outcomes of obese, nonobese and lean NAFLD in the United States, 1999–2016. J Intern Med. 2020;288(1):139–151
Younoussi ZM, Stepanova M, Negro F, et al. Nonalcoholic fatty liver disease in lean individuals in the United States. Medicine. 2012;91:319–327
Loomis AK, Kabadi S, Preiss D, et al. Body mass index and risk of nonalcoholic fatty liver disease: two electronic health record propsective studies. J Clin Endocrinal Metab. 2016;101:945–952
Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73(1):202–209
Eslam M, Sarin SK, Wong VWS, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020;14:889–919. https://doi.org/10.1007/s12072-020-10094-2
Feldman A, Eder SK, Felder TK, Kedenko L, Paulweber B, Stadlmayr A, et al. Clinical and metabolic characterization of lean Caucasian subjects with non-alcoholic fatty liver. Am J Gastroenterol. 2017;112:102–110
Cheng YM, Kao JH, Wang CC. The metabolic profiles and body composition of lean metabolic associated fatty liver disease. Hepatol Int. 2022;15:405–412
NCHS. National Health and Nutrition Examination Survey (NHANES). Available at: https://wwwn.cdc.gov/nchs/nhanes/Nhanes3/Default.aspx. Accessed Aug 18, 2021).
National Health and Nutrition Examination Survey, Third National Health and Nutrition Examination Survey: Hepatic/Gallbladder Ultrasound and Hepatic Steatosis (HGUHS). https://wwwn.cdc.gov/nchs/Data/Nhanes3/34A/HGUHS.htm. Accessed Aug 23, 2021.
National Health and Nutrition Examination Survey (NHANES) III, Hepatic Steatosis Ultrasound Images Assessment Procedures Manual 2010. https://www.cdc.gov/nchs/data/nhanes/nhanes3/hepatic_steatosis_ultrasound_procedures_manual.pdf. Accessed Aug 23, 2021.
Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45(4):846–854
Sterling RK, Lissen E, Clumeck N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43(6):1317–1325
NCHS. Key Concepts About Weighting in NHANES. Available at: https://www.cdc.gov/nchs/tutorials/NHANES/SurveyDesign/Weighting/OverviewKey.htm. Accessed Aug 23, 2021.
StataCorp LP. Stata survival analysis and epidemiological tables reference manual; 1985. Accessed Aug 23, 2021.
Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015;62(1 Suppl):S47-64. https://doi.org/10.1016/j.jhep.2014.12.012
Stepanova M, Younossi ZM. Independent association between nonalcoholic fatty liver disease and cardiovascular disease in the US population. Clin Gastroenterol Hepatol. 2012;10:646–650
Lazo M, Hernaez R, Bonekamp S, Kamel IR, Brancati FL, Guallar E, et al. Non-alcoholic fatty liver disease and mortality among US adults: prospective cohort study. BMJ. 2011;343: d6891
Chen F, Esmaili S, Rogers GB, Bugianesi E, Petta S, Marchesini G, et al. Lean NAFLD: a distinct entity shaped by differential metabolic adaptation. Hepatology. 2020;71(4):1213–1227. https://doi.org/10.1002/hep.30908
Alam S, Eslam M, Skm Hasan N, Anam K, Chowdhury MAB, Khan MAS, et al. Risk factors of nonalcoholic fatty liver disease in lean body mass population: a systematic review and meta-analysis. JGH Open. 2021;5(11):1236–1249. https://doi.org/10.1002/jgh3.12658
Golabi P, Paik J, Fukui N, Locklear CT, de Avilla L, Younossi ZM. Patients with lean nonalcoholic fatty liver disease are metabolically abnormal and have a higher risk for mortality. Clin Diabetes. 2019;37(1):65–72. https://doi.org/10.2337/cd18-0026.PMID:30705499;PMCID:PMC6336127
Hagström H, Nasr P, Ekstedt M, Hammar U, Stål P, Hultcrantz R, et al. Fibrosis stage but not NASH predicts mortality and time to development of severe liver disease in biopsy-proven NAFLD. J Hepatol. 2017;67(6):1265–1273. https://doi.org/10.1016/j.jhep.2017.07.027
Dulai PS, Singh S, Patel J, Soni M, Prokop LJ, Younossi Z, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta-analysis. Hepatology. 2017;65(5):1557–1565. https://doi.org/10.1002/hep.29085
Ekstedt M, Hagström H, Nasr P, Fredrikson M, Stål P, Kechagias S, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61(5):1547–1554. https://doi.org/10.1002/hep.27368
Taylor RS, Taylor RJ, Bayliss S, Hagström H, Nasr P, Schattenberg JM, et al. Association between fibrosis stage and outcomes of patients with nonalcoholic fatty liver disease: a systematic review and meta analysis. Gastroenterology. 2020;158(6):1611-1625.e12. https://doi.org/10.1053/j.gastro.2020.01.043
Kim D, Konyn P, Sandhu KK, Dennis BB, Cheung AC, Ahmed A. Metabolic dysfunction-associated fatty liver disease is associated with increased all-cause mortality in the United States. J Hepatol. 2021;75(6):1284–1291. https://doi.org/10.1016/j.jhep.2021.07.035
Younossi ZM, Corey KE, Lim JK. AGA clinical practice update on lifestyle modification using diet and exercise to achieve weight loss in the management of nonalcoholic fatty liver disease: expert review. Gastroenterology. 2021;160(3):912–918. https://doi.org/10.1053/j.gastro.2020.11.051
Paik JM, Mir S, Alqahtani SA, Younossi Y, Ong JP, Younossi ZM. Dietary risks for liver mortality in NAFLD: global burden of disease data. Hepatol Commun. 2021. https://doi.org/10.1002/hep4.1707
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Guarantor of the article: MHN. Specific author contributions: Study design: ADD, VHN, MHN. Data collection: ADD, VHN. Data analysis: ADD, VHN, MHN. Drafting of the article: ADD, VHN, MHN. Data interpretation, review and/or revision of the manuscript: All authors. Study concept and study supervision: MHN.
Corresponding author
Ethics declarations
Conflict of interest
Mindie H. Nguyen: Research support: Pfizer, Enanta, Gilead, Exact Sciences, Vir Biotech, Helio Health, National Cancer Institute, Glycotest, B. K. Kee Foundation; Consulting and/or Advisory Board: Intercept, Exact Science, Gilead, GSK, Eli Lilly, Laboratory of Advanced Medicine, Janssen. Ramsey Cheung: Research support: Gilead. Allen D. Dao, Vy H. Nguyen and Takanori Ito have no relevant financial or non-financial interests to disclose.
Informed consent
All participants gave written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dao, A.D., Nguyen, V.H., Ito, T. et al. Prevalence, characteristics, and mortality outcomes of obese and nonobese MAFLD in the United States. Hepatol Int 17, 225–236 (2023). https://doi.org/10.1007/s12072-022-10436-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-022-10436-2