Abstract
Background and aims
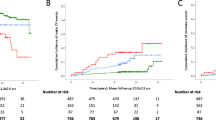
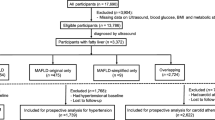
The new metabolic dysfunction-associated fatty liver disease (MAFLD) criteria include the following three distinct subtypes: MAFLD with diabetes mellitus (DM), overweight/obese (OW), or lean/normal weight with metabolic dysfunction. We investigated whether long-term cardiovascular disease outcomes differ across the MAFLD subtypes.
Methods
From a nationwide health screening database, we included 8,412,730 participants (48.6% males) aged 40–64 years, free of cardiovascular disease history, between 2009 and 2010. Participants were categorized into non-MAFLD, OW-MAFLD, lean-MAFLD, and DM-MAFLD. The primary outcome was a composite cardiovascular disease event, including myocardial infarction, ischemic stroke, heart failure, or cardiovascular disease-related death. The presence of advanced liver fibrosis was estimated using a BARD score ≥ 2.
Results
Among the study participants, 3,087,640 (36.7%) had MAFLD, among which 2,424,086 (78.5%), 170,761 (5.5%), and 492,793 (16.0%) had OW-MAFLD, lean-MAFLD, and DM-MAFLD, respectively. Over a median follow-up period of 10.0 years, 169,433 new cardiovascular disease events occurred. With the non-MAFLD group as reference, multivariable-adjusted hazard ratios (95% confidence intervals) for cardiovascular disease events were 1.16 (1.15–1.18), 1.23 (1.20–1.27), and 1.82 (1.80–1.85) in the OW-MAFLD, lean-MAFLD, and DM-MAFLD groups, respectively. Participants with lean-MAFLD or DM-MAFLD had a higher cardiovascular disease risk than those with OW-MAFLD, irrespective of metabolic abnormalities or comorbidities. The presence of advanced liver fibrosis was significantly associated with a higher cardiovascular disease risk in each MAFLD subtype.
Conclusion
Long-term cardiovascular disease outcomes differed across the MAFLD subtypes. Further studies are required to investigate whether preventive or therapeutic interventions should be optimized according to the MAFLD subtypes.



Similar content being viewed by others
References
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. https://doi.org/10.1002/hep.28431
Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73(1):202–209. https://doi.org/10.1016/j.jhep.2020.03.039
Eslam M, Sanyal AJ, George J. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020;158(7):1999-2014.e1991. https://doi.org/10.1053/j.gastro.2019.11.312
Lee H, Lee YH, Kim SU, Kim HC. Metabolic dysfunction-associated fatty liver disease and incident cardiovascular disease risk: a nationwide cohort study. Clin Gastroenterol Hepatol. 2021;19(10):2138-2147.e2110. https://doi.org/10.1016/j.cgh.2020.12.022
Lee H, Lee HW, Kim SU, Chang Kim H. Metabolic dysfunction-associated fatty liver disease increases colon cancer risk: a nationwide cohort study. Clin Transl Gastroenterol 2022;13(1):e00435. https://doi.org/10.14309/ctg.0000000000000435
Tsutsumi T, Eslam M, Kawaguchi T, Yamamura S, Kawaguchi A, Nakano D, et al. MAFLD better predicts the progression of atherosclerotic cardiovascular risk than NAFLD: generalized estimating equation approach. Hepatol Res. 2021;51(11):1115–1128. https://doi.org/10.1111/hepr.13685
Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017;7(9): e016640. https://doi.org/10.1136/bmjopen-2017-016640
EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 2016;64(6):1388–1402. https://doi.org/10.1016/j.jhep.2015.11.004
Lee YH, Bang H, Park YM, Bae JC, Lee BW, Kang ES, et al. Non-laboratory-based self-assessment screening score for non-alcoholic fatty liver disease: development, validation and comparison with other scores. PLoS ONE. 2014;9(9): e107584. https://doi.org/10.1371/journal.pone.0107584
Vilar-Gomez E, Chalasani N. Non-invasive assessment of non-alcoholic fatty liver disease: clinical prediction rules and blood-based biomarkers. J Hepatol. 2018;68(2):305–315. https://doi.org/10.1016/j.jhep.2017.11.013
Lee H, Yano Y, Cho SMJ, Park JH, Park S, Lloyd-Jones DM, et al. Cardiovascular risk of isolated systolic or diastolic hypertension in young adults. Circulation. 2020;141(22):1778–1786. https://doi.org/10.1161/CIRCULATIONAHA.119.044838
Seo HJ, Oh IH, Yoon SJ. A comparison of the cancer incidence rates between the national cancer registry and insurance claims data in Korea. Asian Pac J Cancer Prev. 2012;13(12):6163–6168. https://doi.org/10.7314/apjcp.2012.13.12.6163
Fan JG, Saibara T, Chitturi S, Kim BI, Sung JJ, Chutaputti A, et al. What are the risk factors and settings for non-alcoholic fatty liver disease in Asia-Pacific? J Gastroenterol Hepatol. 2007;22(6):794–800. https://doi.org/10.1111/j.1440-1746.2007.04952.x
Bhatnagar A. Environmental determinants of cardiovascular disease. Circ Res. 2017;121(2):162–180. https://doi.org/10.1161/CIRCRESAHA.117.306458
Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: a meta-analysis. J Hepatol. 2016;65(3):589–600. https://doi.org/10.1016/j.jhep.2016.05.013
Fox CS, Coady S, Sorlie PD, D’Agostino RB Sr, Pencina MJ, Vasan RS, et al. Increasing cardiovascular disease burden due to diabetes mellitus: the Framingham Heart Study. Circulation. 2007;115(12):1544–1550. https://doi.org/10.1161/circulationaha.106.658948
King RJ, Grant PJ. Diabetes and cardiovascular disease: pathophysiology of a life-threatening epidemic. Herz. 2016;41(3):184–192. https://doi.org/10.1007/s00059-016-4414-8
Yoneda M, Yamamoto T, Honda Y, Imajo K, Ogawa Y, Kessoku T, et al. Risk of cardiovascular disease in patients with fatty liver disease as defined from the metabolic dysfunction associated fatty liver disease or nonalcoholic fatty liver disease point of view: a retrospective nationwide claims database study in Japan. J Gastroenterol. 2021;56(11):1022–1032. https://doi.org/10.1007/s00535-021-01828-6
Golabi P, Paik J, Fukui N, Locklear CT, de Avilla L, Younossi ZM. Patients with lean nonalcoholic fatty liver disease are metabolically abnormal and have a higher risk for mortality. Clin Diabetes. 2019;37(1):65–72. https://doi.org/10.2337/cd18-0026
Yoshitaka H, Hamaguchi M, Kojima T, Fukuda T, Ohbora A, Fukui M. Nonoverweight nonalcoholic fatty liver disease and incident cardiovascular disease: a post hoc analysis of a cohort study. Medicine (Baltimore). 2017;96(18): e6712. https://doi.org/10.1097/md.0000000000006712
Lu FB, Hu ED, Xu LM, Chen L, Wu JL, Li H, et al. The relationship between obesity and the severity of non-alcoholic fatty liver disease: systematic review and meta-analysis. Expert Rev Gastroenterol Hepatol. 2018;12(5):491–502. https://doi.org/10.1080/17474124.2018.1460202
Ahmed OT, Gidener T, Mara KC, Larson JJ, Therneau TM, Allen AM. Natural history of nonalcoholic fatty liver disease with normal body mass index: a population-based study. Clin Gastroenterol Hepatol. 2022;20(6):1374-1381.e1376. https://doi.org/10.1016/j.cgh.2021.07.016
Han E, Lee YH, Kim YD, Kim BK, Park JY, Kim DY, et al. Nonalcoholic fatty liver disease and sarcopenia are independently associated with cardiovascular risk. Am J Gastroenterol 2020;115(4):584–595. https://doi.org/10.14309/ajg.0000000000000572
Tamaki N, Kurosaki M, Takahashi Y, Itakura Y, Inada K, Kirino S, et al. Liver fibrosis and fatty liver as independent risk factors for cardiovascular disease. J Gastroenterol Hepatol. 2021;36(10):2960–2966. https://doi.org/10.1111/jgh.15589
Kim Y, Han E, Lee JS, Lee HW, Kim BK, Kim MK, et al. Cardiovascular risk is elevated in lean subjects with nonalcoholic fatty liver disease. Gut Liver. 2021. https://doi.org/10.5009/gnl210084
Han E, Lee YH, Lee BW, Kang ES, Lee IK, Cha BS. Anatomic fat depots and cardiovascular risk: a focus on the leg fat using nationwide surveys (KNHANES 2008–2011). Cardiovasc Diabetol. 2017;16(1):54. https://doi.org/10.1186/s12933-017-0536-4
Polesel J, Zucchetto A, Montella M, Dal Maso L, Crispo A, La Vecchia C, et al. The impact of obesity and diabetes mellitus on the risk of hepatocellular carcinoma. Ann Oncol. 2009;20(2):353–357
Sohn W, Kwon HJ, Chang Y, Ryu S, Cho YK. Liver fibrosis in Asians with metabolic dysfunction-associated fatty liver disease. Clin Gastroenterol Hepatol. 2021. https://doi.org/10.1016/j.cgh.2021.06.042
Chen X, Chen S, Pang J, Tang Y, Ling W. Are the different MAFLD subtypes based on the inclusion criteria correlated with all-cause mortality? J Hepatol. 2021;75(4):987–989. https://doi.org/10.1016/j.jhep.2021.06.013
Lee JI, Lee HW, Lee KS, Lee HS, Park JY. Effects of statin use on the development and progression of nonalcoholic fatty liver disease: a nationwide nested case–control study. Am J Gastroenterol 2021;116(1):116–124. https://doi.org/10.14309/ajg.0000000000000845
Funding
This study was supported by the Technology Innovation Program (20013712) funded by the Ministry of Trade, Industry and Energy (MOTIE, Korea) and by a new faculty research seed money grant of Yonsei University College of Medicine (2022-32-0090). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors conceived and designed the study. Hokyou Lee conducted statistical analyses, and all authors interpreted the findings. Hokyou Lee and Tae Seop Lim drafted the manuscript. Seung Up Kim and Hyeon Chang Kim critically reviewed the manuscript for key intellectual content. All authors approved the final manuscript. Seung Up Kim and Hyeon Chang Kim are the guarantors, and as such, had full access to the data and take responsibility for its integrity and accuracy.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. The study protocol was approved by the Institutional Review Board of Yonsei University Health System, Seoul, Korea (#Y-2019–0081) with a waiver of informed consent because this was a retrospective study of de-identified, routinely collected data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, H., Lim, T.S., Kim, S.U. et al. Long-term cardiovascular outcomes differ across metabolic dysfunction-associated fatty liver disease subtypes among middle-aged population. Hepatol Int 16, 1308–1317 (2022). https://doi.org/10.1007/s12072-022-10407-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-022-10407-7