Abstract
Background/purpose of the study
Although low skeletal muscle mass is associated with non-alcoholic fatty liver disease (NAFLD), it is currently uncertain whether there are associations between weight-adjusted appendicular skeletal muscle (ASM%), severity of histological features of NAFLD, and the patatin-like phospholipase domain-containing 3 (PNPLA3) rs738409 polymorphism. Our aim was to test for a possible influence of the PNPLA3 rs738409 variant on the association between ASM% and severity of NAFLD histological features.
Methods
We enrolled 401 Chinese male with biopsy-proven NAFLD. Using a bioelectrical-impedance body composition analyzer (BIA, Inbody 720, Japan Inc., Tokyo), we calculated the ASM% as the percentage of total appendicular skeletal muscle mass (ASM, kg)/total body mass (kg) × 100.
Results
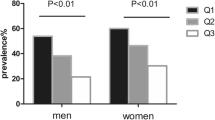
Compared to those with high ASM%, patients with low ASM% (≤ 30.6, i.e., the median value of distribution of the whole sample) had a greater severity of individual histological features of NAFLD. These patients also had a higher risk of severe steatosis and non-alcoholic steatohepatitis (NASH) (adjusted-odds ratio [OR] 2.34, 95% CI 1.39–3.93, and adjusted-OR 2.22, 95% CI 1.30–3.77) even after adjusting for age, body mass index, diabetes, and serum creatinine levels. Carriage of the G allele of PNPLA3 rs738409 plus low ASM% was associated with a higher risk of severe steatosis and presence of liver fibrosis (OR 3.02, 95% CI 1.46–6.26, p = 0.003 and OR 2.18, 95% CI 1.03–4.60, p = 0.041 respectively), and there was a non-significant but borderline increased risk of NASH (OR 2.00, 95% CI 0.98–4.06, p = 0.056).
Conclusions
Low ASM% and the presence of a G allele within PNPLA3 rs738409 is associated with more severe histological features of NAFLD.



Similar content being viewed by others
Abbreviations
- NAFLD:
-
Non-alcoholic fatty liver disease
- BMI:
-
Body mass index
- ASM%:
-
Weight-adjusted appendicular skeletal muscle
- HOMA-IR:
-
Homeostasis model assessment-insulin resistance
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- GGT:
-
γ-Glutamyltranspeptidase
- ALP:
-
Alkaline phosphatase
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- CK-18:
-
Cytokeratin-18
- PNPLA3 :
-
Patatin-like phospholipase domain-containing 3
- NAS:
-
NAFLD activity score
- NASH:
-
Non-alcoholic steatohepatitis
- BIA:
-
Bioelectrical impedance analyzer
- CI:
-
Confidence interval
- NASH-CRN:
-
NASH-Clinical Research Network
- OR:
-
Odds ratio
References
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016;64:73–84
Yilmaz Y. Review article: is non-alcoholic fatty liver disease a spectrum, or are steatosis and non-alcoholic steatohepatitis distinct conditions? Aliment Pharmacol Ther 2012;36:815–823
Powell EE, Wong VW, Rinella M. Non-alcoholic fatty liver disease. Lancet 2021;397:2212–2224
Liu HH, Cao YX, Jin JL, Guo YL, Zhu CG, Wu NQ, et al. Metabolic-associated fatty liver disease and major adverse cardiac events in patients with chronic coronary syndrome: a matched case-control study. Hepatol Int 2021;15:1337–1346
Sun DQ, Jin Y, Wang TY, Zheng KI, Rios RS, Zhang HY, et al. MAFLD and risk of CKD. Metabolism 2021;115: 154433
Wang TY, Wang RF, Bu ZY, Targher G, Byrne CD, Sun DQ, et al. Association of metabolic dysfunction-associated fatty liver disease with kidney disease. Nat Rev Nephrol 2022;18:259–268
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019;48:16–31
Sinclair M, Gow PJ, Grossmann M, Angus PW. Review article: sarcopenia in cirrhosis–aetiology, implications and potential therapeutic interventions. Aliment Pharmacol Ther 2016;43:765–777
Hong HC, Hwang SY, Choi HY, Yoo HJ, Seo JA, Kim SG, et al. Relationship between sarcopenia and nonalcoholic fatty liver disease: the Korean Sarcopenic obesity study. Hepatology 2014;59:1772–1778
Lee YH, Kim SU, Song K, Park JY, Kim DY, Ahn SH, et al. Sarcopenia is associated with significant liver fibrosis independently of obesity and insulin resistance in nonalcoholic fatty liver disease: nationwide surveys (KNHANES 2008–2011). Hepatology 2016;63:776–786
Lee YH, Jung KS, Kim SU, Yoon HJ, Yun YJ, Lee BW, et al. Sarcopaenia is associated with NAFLD independently of obesity and insulin resistance: nationwide surveys (KNHANES 2008–2011). J Hepatol 2015;63:486–493
Koo BK, Kim D, Joo SK, Kim JH, Chang MS, Kim BG, et al. Sarcopenia is an independent risk factor for non-alcoholic steatohepatitis and significant fibrosis. J Hepatol 2017;66:123–131
Petta S, Ciminnisi S, Di Marco V, Cabibi D, Camma C, Licata A, et al. Sarcopenia is associated with severe liver fibrosis in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther 2017;45:510–518
Liu Z, Zhang Y, Graham S, Wang X, Cai D, Huang M, et al. Causal relationships between NAFLD, T2D and obesity have implications for disease subphenotyping. J Hepatol 2020;73:263–276
Meffert PJ, Repp KD, Volzke H, Weiss FU, Homuth G, Kuhn JP, et al. The PNPLA3 SNP rs738409: G allele is associated with increased liver disease-associated mortality but reduced overall mortality in a population-based cohort. J Hepatol 2018;68:858–860
Xia MF, Lin HD, Chen LY, Wu L, Ma H, Li Q, et al. The PNPLA3 rs738409 C > G variant interacts with changes in body weight over time to aggravate liver steatosis, but reduces the risk of incident type 2 diabetes. Diabetologia 2019;62:644–654
Xia MF, Chen LY, Wu L, Ma H, Li Q, Aleteng Q, et al. The PNPLA3 rs738409 C > G variant influences the association between low skeletal muscle mass and NAFLD: the Shanghai Changfeng study. Aliment Pharmacol Ther 2019;50:684–695
Liu WY, Zheng KI, Pan XY, Ma HL, Zhu PW, Wu XX, et al. Effect of PNPLA3 polymorphism on diagnostic performance of various noninvasive markers for diagnosing and staging nonalcoholic fatty liver disease. J Gastroenterol Hepatol 2020;35:1057–1064
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–419
Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005;41:1313–1321
Brunt EM. Nonalcoholic fatty liver disease: pros and cons of histologic systems of evaluation. Int J Mol Sci 2016;17(1):97
Bhanji RA, Narayanan P, Allen AM, Malhi H, Watt KD. Sarcopenia in hiding: the risk and consequence of underestimating muscle dysfunction in nonalcoholic steatohepatitis. Hepatology 2017;66:2055–2065
Gan D, Wang L, Jia M, Ru Y, Ma Y, Zheng W, et al. Low muscle mass and low muscle strength associate with nonalcoholic fatty liver disease. Clin Nutr 2020;39:1124–1130
Tanaka M, Okada H, Hashimoto Y, Kumagai M, Nishimura H, Oda Y, et al. Relationship between nonalcoholic fatty liver disease and muscle quality as well as quantity evaluated by computed tomography. Liver Int 2020;40:120–130
Pan X, Han Y, Zou T, Zhu G, Xu K, Zheng J, et al. Sarcopenia contributes to the progression of nonalcoholic fatty liver disease- related fibrosis: a meta-analysis. Dig Dis 2018;36:427–436
Seko Y, Mizuno N, Okishio S, Takahashi A, Kataoka S, Okuda K, et al. Clinical and pathological features of sarcopenia-related indices in patients with non-alcoholic fatty liver disease. Hepatol Res 2019;49:627–636
Shen J, Wong GL, Chan HL, Chan RS, Chan HY, Chu WC, et al. PNPLA3 gene polymorphism and response to lifestyle modification in patients with nonalcoholic fatty liver disease. J Gastroenterol Hepatol 2015;30:139–146
Lee MJ, Kim EH, Bae SJ, Kim GA, Park SW, Choe J, et al. Age-related decrease in skeletal muscle mass is an independent risk factor for incident nonalcoholic fatty liver disease: a 10-year retrospective cohort study. Gut Liver 2019;13:67–76
Kim G, Lee SE, Lee YB, Jun JE, Ahn J, Bae JC, et al. Relationship between relative skeletal muscle mass and nonalcoholic fatty liver disease: a 7-year longitudinal study. Hepatology 2018;68:1755–1768
Wei JL, Leung JC, Loong TC, Wong GL, Yeung DK, Chan RS, et al. Prevalence and severity of nonalcoholic fatty liver disease in non-obese patients: a population study using proton-magnetic resonance spectroscopy. Am J Gastroenterol 2015;110:1306–1314
Seo DH, Lee YH, Park SW, Choi YJ, Huh BW, Lee E, et al. Sarcopenia is associated with non-alcoholic fatty liver disease in men with type 2 diabetes. Diabetes Metab 2020;46:362–369
Hashimoto Y, Osaka T, Fukuda T, Tanaka M, Yamazaki M, Fukui M. The relationship between hepatic steatosis and skeletal muscle mass index in men with type 2 diabetes. Endocr J 2016;63:877–884
Bredella MA. Sex differences in body composition. Adv Exp Med Biol 2017;1043:9–27
Gheller BJ, Riddle ES, Lem MR, Thalacker-Mercer AE. Understanding age-related changes in skeletal muscle metabolism: differences between females and males. Annu Rev Nutr 2016;36:129–156
Bosy-Westphal A, Jensen B, Braun W, Pourhassan M, Gallagher D, Muller MJ. Quantification of whole-body and segmental skeletal muscle mass using phase-sensitive 8-electrode medical bioelectrical impedance devices. Eur J Clin Nutr 2017;71:1061–1067
Kuwashiro T, Takahashi H, Hyogo H, Ogawa Y, Imajo K, Yoneda M, et al. Discordant pathological diagnosis of non-alcoholic fatty liver disease: a prospective multicenter study. JGH Open 2020;4:497–502
Leung HH, Puspanathan P, Chan AW, Nik Mustapha NR, Wong VW, Chan WK. Reliability of the nonalcoholic steatohepatitis clinical research network and steatosis activity fibrosis histological scoring systems. J Gastroenterol Hepatol 2022;37(6):1131–1138
Funding
This work was supported by grants from the National Natural Science Foundation of China (82070588), High Level Creative Talents from Department of Public Health in Zhejiang Province and Project of New Century 551 Talent Nurturing in Wenzhou. GT is supported in part by grants from the School of Medicine, University of Verona, Verona, Italy. CDB is supported in part by the Southampton NIHR Biomedical Research Centre (IS-BRC-20004), UK. XYP is supported in part by grants from Wenzhou science and technology Bureau (Y20180141).
Author information
Authors and Affiliations
Contributions
Guarantor of the article: M-HZ. Authors’ contributions: Study concept and design: X-YP, W-YL and M-HZ. Acquisition of data: P-WZ, GL, L-JT, O-YH, H-YY. Pathology analysis: X-DW. Drafting of the manuscript: X-YP and W-YL. Critical revision and comment: GT and CDB. Statistical analysis: X-YP, W-YL, FG. Study supervision: M-HZ. All authors contributed to the manuscript for important intellectual content and approved the submission.
Corresponding author
Ethics declarations
Conflict of interest
All the authors (Xiao-Yan Pan, Wen-Yue Liu, Pei-Wu Zhu, Gang Li, Liang-Jie Tang, Feng Gao, Ou-Yang Huang, Hai-Yang Yuan, Giovanni Targher, Christopher D. Byrne, Xiao-Dong Wang, Ming-Hua Zheng) declare that they do not have anything to disclose regarding any funding or conflict of interest with respect to this manuscript.
Ethical approval
Ethical approval for the study was obtained from the ethics committee of the First Affiliated Hospital of Wenzhou Medical University. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Written informed consent was obtained from all participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pan, XY., Liu, WY., Zhu, PW. et al. Low skeletal muscle mass is associated with more severe histological features of non-alcoholic fatty liver disease in male. Hepatol Int 16, 1085–1093 (2022). https://doi.org/10.1007/s12072-022-10384-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-022-10384-x