Abstract
Aim
This study aimed to investigate the utility of C-reactive protein (CRP) and alpha-fetoprotein (AFP) in immunotherapy (CRAFITY) score in hepatocellular carcinoma (HCC) patients receiving atezolizumab and bevacizumab (Atez/Bev).
Methods
This retrospective cohort study included a total of 297 patients receiving Atez/Bev from September 2020 to November 2021 at 21 different institutions and hospital groups in Japan. Patients with AFP ≥ 100 ng/mL and those with CRP ≥ 1 mg/dL were assigned a CRAFITY score of 1 point.
Results
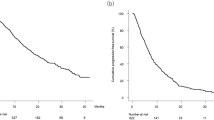
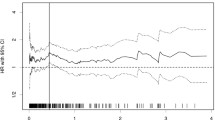
The patients were assigned CRAFITY scores of 0 points (n = 147 [49.5%]), 1 point (n = 111 [37.4%]), and 2 points (n = 39 [13.1%]). AFP ≥ 100 ng/mL and CRP ≥ 1.0 mg/dL were significantly associated with progression-free survival (PFS) and overall survival (OS). The median PFS in the CRAFITY score 0, 1, and 2 groups was 11.8 months (95% confidence interval [CI] 6.4-not applicable [NA]), 6.5 months (95% CI 4.6–8.0), and 3.2 months (95% CI 1.9–5.0), respectively (p < 0.001). The median OS in patients with CRAFITY score 0, 1 and 2 was not reached, 14.3 months (95% CI 10.5-NA), and 11.6 months (95% CI 4.9-NA), respectively. The percentage of patients with grade ≥ 3 liver injury, any grade of decreased appetite, any grade of proteinuria, any grade of fever, and any grade of fatigue was lowest in patients with a CRAFITY score of 0, followed by patients with CRAFITY scores of 1 and 2.
Conclusions
The CRAFITY score is simple and could be useful for predicting therapeutic outcomes and treatment-related adverse events.



Similar content being viewed by others
References
Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382:1894–1905
Gordan JD, Kennedy EB, Abou-Alfa GK, Beg MS, Brower ST, Gade TP, et al. Systemic therapy for advanced hepatocellular carcinoma: ASCO guideline. J Clin Oncol. 2020;38:4317–4345
Vogel A, Martinelli E. Updated treatment recommendations for hepatocellular carcinoma (HCC) from the ESMO Clinical Practice Guidelines. Ann Oncol. 2021;32:801–805
Llovet JM, Villanueva A, Marrero JA, Schwartz M, Meyer T, Galle PR, et al. Trial design and endpoints in hepatocellular carcinoma: AASLD Consensus Conference. Hepatology. 2021;73(Suppl 1):158–191
El-Khoueiry AB, Sangro B, Yau T, Crocenzi TS, Kudo M, Hsu C, et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389:2492–2502
Zhu AX, Finn RS, Edeline J, Cattan S, Ogasawara S, Palmer D, et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): a non-randomised, open-label phase 2 trial. Lancet Oncol. 2018;19:940–952
Finn RS, Ryoo BY, Merle P, Kudo M, Bouattour M, Lim HY, et al. Pembrolizumab as second-line therapy in patients with advanced hepatocellular carcinoma in KEYNOTE-240: A randomized, double-blind, phase III Trial. J Clin Oncol. 2020;38:193–202
Lee MS, Ryoo BY, Hsu CH, Numata K, Stein S, Verret W, et al. Atezolizumab with or without bevacizumab in unresectable hepatocellular carcinoma (GO30140): an open-label, multicentre, phase 1b study. Lancet Oncol. 2020;21:808–820
Li XS, Li JW, Li H, Jiang T. Prognostic value of programmed cell death ligand 1 (PD-L1) for hepatocellular carcinoma: a meta-analysis. 2020. Biosci Rep. https://doi.org/10.1042/BSR20200459
de Galarreta MR, Bresnahan E, Molina-Sánchez P, Lindblad KE, Maier B, Sia D, et al. β-catenin activation promotes immune escape and resistance to anti-PD-1 therapy in hepatocellular carcinoma. Cancer Discov. 2019;9:1124–1141
Sia D, Jiao Y, Martinez-Quetglas I, Kuchuk O, Villacorta-Martin C, de Moura MC, et al. Identification of an immune-specific class of hepatocellular carcinoma, based on molecular features. Gastroenterology. 2017;153:812–826
Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, et al. Hepatocellular carcinoma. Nat Rev Dis Primers. 2021;7:6
Scheiner B, Pomej K, Kirstein MM, Hucke F, Finkelmeier F, Waidmann O, et al. Prognosis of patients with hepatocellular carcinoma treated with immunotherapy - development and validation of the CRAFITY score. J Hepatol. 2022;76(2):353–363
Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33:550–558
Hiraoka A, Michitaka K, Kumada T, Izumi N, Kadoya M, Kokudo N, et al. Validation and potential of albumin-bilirubin grade and prognostication in a nationwide survey of 46,681 hepatocellular carcinoma patients in Japan: The need for a more detailed evaluation of hepatic function. Liver Cancer. 2017;6:325–336
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48:452–458
Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012;55:2005–2023
Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–209
Ridder DA, Weinmann A, Schindeldecker M, Urbansky LL, Berndt K, Gerber TS, et al. Comprehensive clinicopathologic study of alpha fetoprotein-expression in a large cohort of patients with hepatocellular carcinoma. Int J Cancer. 2021;150(6):1053–1066
Mazzaferro V, Sposito C, Zhou J, Pinna AD, De Carlis L, Fan J, et al. Metroticket 2.0 model for analysis of competing risks of death after liver transplantation for hepatocellular carcinoma. Gastroenterology. 2018;154:128–139
Lee DH, Lee JM, Lee JY, Kim SH, Yoon JH, Kim YJ, et al. Radiofrequency ablation of hepatocellular carcinoma as first-line treatment: long-term results and prognostic factors in 162 patients with cirrhosis. Radiology. 2014;270:900–909
N’Kontchou G, Mahamoudi A, Aout M, Ganne-Carrié N, Grando V, Coderc E, et al. Radiofrequency ablation of hepatocellular carcinoma: long-term results and prognostic factors in 235 Western patients with cirrhosis. Hepatology. 2009;50:1475–1483
Takayasu K, Arii S, Kudo M, Ichida T, Matsui O, Izumi N, et al. Superselective transarterial chemoembolization for hepatocellular carcinoma. Validation of treatment algorithm proposed by Japanese guidelines. J Hepatol. 2012;56:886–892
Mehta N, Dodge JL, Roberts JP, Yao FY. Validation of the prognostic power of the RETREAT score for hepatocellular carcinoma recurrence using the UNOS database. Am J Transplant. 2018;18:1206–1213
Kudo M, Finn RS, Qin S, Han KH, Ikeda K, Piscaglia F, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391:1163–1173
Bruix J, Qin S, Merle P, Granito A, Huang YH, Bodoky G, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389:56–66
Hoshida Y, Nijman SM, Kobayashi M, Chan JA, Brunet JP, Chiang DY, et al. Integrative transcriptome analysis reveals common molecular subclasses of human hepatocellular carcinoma. Cancer Res. 2009;69:7385–7392
Yamashita T, Forgues M, Wang W, Kim JW, Ye Q, Jia H, et al. EpCAM and alpha-fetoprotein expression defines novel prognostic subtypes of hepatocellular carcinoma. Cancer Res. 2008;68:1451–1461
Galle PR, Foerster F, Kudo M, Chan SL, Llovet JM, Qin S, et al. Biology and significance of alpha-fetoprotein in hepatocellular carcinoma. Liver Int. 2019;39:2214–2229
Montal R, Andreu-Oller C, Bassaganyas L, Esteban-Fabró R, Moran S, Montironi C, et al. Molecular portrait of high alpha-fetoprotein in hepatocellular carcinoma: implications for biomarker-driven clinical trials. Br J Cancer. 2019;121:340–343
Oyama T, Ran S, Ishida T, Nadaf S, Kerr L, Carbone DP, et al. Vascular endothelial growth factor affects dendritic cell maturation through the inhibition of nuclear factor-kappa B activation in hemopoietic progenitor cells. J Immunol. 1998;160:1224–1232
Gabrilovich DI, Chen HL, Girgis KR, Cunningham HT, Meny GM, Nadaf S, et al. Production of vascular endothelial growth factor by human tumors inhibits the functional maturation of dendritic cells. Nat Med. 1996;2:1096–1103
Borgström P, Hughes GK, Hansell P, Wolitsky BA, Sriramarao P. Leukocyte adhesion in angiogenic blood vessels. Role of E-selectin, P-selectin, and beta2 integrin in lymphotoxin-mediated leukocyte recruitment in tumor microvessels. J Clin Invest. 1997;99:2246–2253
Hegde PS, Wallin JJ, Mancao C. Predictive markers of anti-VEGF and emerging role of angiogenesis inhibitors as immunotherapeutics. Semin Cancer Biol. 2018;52:117–124
Wallin JJ, Bendell JC, Funke R, Sznol M, Korski K, Jones S, et al. Atezolizumab in combination with bevacizumab enhances antigen-specific T-cell migration in metastatic renal cell carcinoma. Nat Commun. 2016;7:12624
Voron T, Colussi O, Marcheteau E, Pernot S, Nizard M, Pointet AL, et al. VEGF-A modulates expression of inhibitory checkpoints on CD8+ T cells in tumors. J Exp Med. 2015;212:139–148
Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9:162–174
Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15:e493-503
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–444
Morris-Stiff G, Gomez D, Prasad KR. C-reactive protein in liver cancer surgery. Eur J Surg Oncol. 2008;34:727–729
Sieghart W, Pinter M, Hucke F, Graziadei I, Schöniger-Hekele M, Müller C, et al. Single determination of C-reactive protein at the time of diagnosis predicts long-term outcome of patients with hepatocellular carcinoma. Hepatology. 2013;57:2224–2234
Meischl T, Rasoul-Rockenschaub S, Györi G, Sieghart W, Reiberger T, Trauner M, et al. C-reactive protein is an independent predictor for hepatocellular carcinoma recurrence after liver transplantation. PLoS ONE. 2019;14: e0216677
Hayashi T, Shibata M, Oe S, Miyagawa K, Honma Y, Harada M. C-reactive protein can predict dose intensity, time to treatment failure and overall survival in HCC treated with lenvatinib. PLoS ONE. 2020;15: e0244370
Riedl JM, Barth DA, Brueckl WM, Zeitler G, Foris V, Mollnar S, et al. C-Reactive Protein (CRP) levels in immune checkpoint inhibitor response and progression in advanced non-small cell lung cancer: a bi-center study. Cancers (Basel). 2020;12:2319
Iivanainen S, Ahvonen J, Knuuttila A, Tiainen S, Koivunen JP. Elevated CRP levels indicate poor progression-free and overall survival on cancer patients treated with PD-1 inhibitors. ESMO Open. 2019;4: e000531
Laino AS, Woods D, Vassallo M, Qian X, Tang H, Wind-Rotolo M, et al. Serum interleukin-6 and C-reactive protein are associated with survival in melanoma patients receiving immune checkpoint inhibition. J Immunother Cancer. 2020;8: e000842
Yoshida T, Ichikawa J, Giuroiu I, Laino AS, Hao Y, Krogsgaard M, et al. C reactive protein impairs adaptive immunity in immune cells of patients with melanoma. J Immunother Cancer. 2020;8: e000234
Zhang L, Liu SH, Wright TT, Shen ZY, Li HY, Zhu W, et al. C-reactive protein directly suppresses Th1 cell differentiation and alleviates experimental autoimmune encephalomyelitis. J Immunol. 2015;194:5243–5252
Jimenez RV, Kuznetsova V, Connelly AN, Hel Z, Szalai AJ. C-reactive protein promotes the expansion of myeloid derived cells with suppressor functions. Front Immunol. 2019;10:2183
Roxburgh CS, McMillan DC. Cancer and systemic inflammation: treat the tumour and treat the host. Br J Cancer. 2014;110:1409–1412
Abolhassani AR, Schuler G, Kirchberger MC, Heinzerling L. C-reactive protein as an early marker of immune-related adverse events. J Cancer Res Clin Oncol. 2019;145:2625–2631
Pfister D, Núñez NG, Pinyol R, Govaere O, Pinter M, Szydlowska M, et al. NASH limits anti-tumour surveillance in immunotherapy-treated HCC. Nature. 2021;592:450–456
Haber PK, Puigvehí M, Castet F, Lourdusamy V, Montal R, Tabrizian P, et al. Evidence-based management of hepatocellular carcinoma: Systematic review and meta-analysis of randomized controlled trials (2002–2020). Gastroenterology. 2021;161:879–898
Hatanaka T, Kakizaki S, Nagashima T, Namikawa M, Ueno T, Tojima H, et al. Lenvatinib for hepatocellular carcinoma patients with nonviral infection who were unlikely to respond to immunotherapy: a retrospective, comparative study. Oncology. 2021;99:641–651
Hiraoka A, Kumada T, Tada T, Tani J, Kariyama K, Fukunishi S, et al. Efficacy of lenvatinib for unresectable hepatocellular carcinoma based on background liver disease etiology: multi-center retrospective study. Sci Rep. 2021;11:16663
Shimose S, Hiraoka A, Nakano M, Iwamoto H, Tanaka M, Tanaka T, et al. First-line sorafenib sequential therapy and liver disease etiology for unresectable hepatocellular carcinoma using inverse probability weighting: a multicenter retrospective study. Cancer Med. 2021;10:8530–8541
Acknowledgement
RELPEC study group member includes Takeshi Hatanaka, Satoru Kakizaki, Atsushi Hiraoka, Toshifumi Tada, Kazuya Kariyama, Koichi Takaguchi, Ei Itobayashi, Kunihiko Tsuji, Toru Ishikawa, Satoshi Yasuda, Hidenori Toyoda, Noritomo Shimada, Takaaki Tanaka, Hideko Ohama, Kazuhiro Nouso, Akemi Tsutsui, Takuya Nagano, Michitaka Imai, Atsushi Naganuma, Shinichiro Nakamura, Takashi Kumada.
Funding
There is no funding sources.
Author information
Authors and Affiliations
Consortia
Contributions
TH, SK, AH, TTad, AN, and TK conceived the study, and participated in its design and coordination. TH, SK, AH, TTad, MH, KKar, JT, MA, KTak, EI, SF, KTs, TI, KTaj, HOc, SY, HT, CO, TNi, NS, KKaw, TTan, HOh, KN, AM, AT, TNa, NI, TO, TA, MI, AN, YK, SN, KJ, HI, and YH performed data curation. TH performed statistical analyses and interpretation. TH, SK, AH, TTad, AN, TK, HK, and MK drafted the text. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Takeshi Hatanaka received lecture fees from Eisai. Atsushi Hiraoka received lecture fees from Bayer, Eisai, Eli Lilly, Otsuka, and Chugai. Takashi Kumada received lecture fees from Eisai.Satoru Kakizaki, Toshifumi Tada, Masashi Hirooka, Kazuya Kariyama, Joji Tani, Masanori Atsukawa, Koichi Takaguchi, Ei Itobayashi, Shinya Fukunishi, Kunihiko Tsuji, Toru Ishikawa, Kazuto Tajiri, Hironori Ochi, Satoshi Yasuda, Hidenori Toyoda, Chikara Ogawa, Takashi Nishimura, Noritomo Shimada, Kazuhito Kawata, Hisashi Kosaka, Takaaki Tanaka, Hideko Ohama, Kazuhiro Nouso, Asahiro Morishita, Akemi Tsutsui, Takuya Nagano, Norio Itokawa, Tomomi Okubo, Taeang Arai, Michitaka Imai, Atsushi Naganuma, Yohei Koizumi, Shinichiro Nakamura, Kouji Joko, Masaki Kaibori, Hiroko Iijima,and Yoichi Hiasa, have no potential conflicts of interest to declare.
Ethical approval
The study protocol was granted approval by the Institutional Ethics Committee of Ehime Prefectural Central Hospital (IRB No. 30–66) (UMIN000043219). All procedures were performed in accordance with the Declaration of Helsinki.
Informed consent
Written informed consent was obtained from all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The RELPEC study group member are mentioned in the Acknowledgement section.
Supplementary Information
Below is the link to the electronic supplementary material.
12072_2022_10358_MOESM1_ESM.tif
(a) The correlation between CRP and the ALBI score (r=0.44, p<0.001). (b) Receiver operating curve analysis. The cutoff value of the ALBI score for CRP ≥1 mg/dL was -2.348; the area under the receiver operating curve was 0.736 (95% CI 0.670-0.803; specificity, 0.648; sensitivity, 0.746). The present cutoff value was close to that of mALBI grade 2a and 2b (i.e., -2.27) (TIF 750 KB)
12072_2022_10358_MOESM2_ESM.tif
(a) PFS in patients with BCLC early and intermediate stage according to the CRAFITY score. The median PFS in the patients with CRAFITY scores of 0, 1, and 2 points was 11.8 months (95% CI 7.0-NA), 7.8 months (95% CI 6.5-12.5), and 3.2 months (95% CI 0.8-9.7), respectively. The PFS was significantly longer in the patients with a CRAFITY score of 0, followed by those with a CRAFITY score of 1, and those with a CRAFITY score of 2 points (p<0.001). (b) The PFS in patients with BCLC advanced and terminal stage according to CRAFITY score. The median PFS in the patients with CRAFITY scores of 0, 1, and 2 points was 6.8 months (95% CI 5.1-NA), 5.3 months (95% CI 3.5-7.6), and 3.0 months (95% CI 1.8-4.6), respectively, which amounted to a statistically significant difference (p=0.011). (c) The PFS in patients receiving Atez/Bev as front-line treatment according to CRAFITY score. The median PFS in the patients with CRAFITY score of 0, 1, and 2 points was 11.8 months (95% CI 6.2-NA), 6.5 months (95% CI 3.5-9.0), and 3.2 months (95% CI 1.6-NA), respectively (p=0.003). (d) The PFS in patients receiving Atez/Bev as later-line treatment according to CRAFITY score. The median PFS in the patients with CRAFITY score of 0, 1, and 2 points was 7.4 months (95% CI 6.1-NA), 6.7 months (95% CI 4.4-8.0), and 3.3 months (95% CI 1.5-5.8), respectively (p=0.001). Atez/Bev, atezolizumab and bevacizumab; BCLC, Barcelona Clinic Liver Cancer; CI, confidence interval; CRAFITY score, C-reactive protein and alpha-fetoprotein in immunotherapy; NA, not applicable; PFS, progression-free survival (TIF 1173 KB)
12072_2022_10358_MOESM3_ESM.tif
(a) The overall survival in patients with BCLC early and intermediate stage according to the CRAFITY score. The median OS in patients with CRAFITY score 0 was not reached and it was 14.3 months (95% CI 10.0-NA) in patients with CRAFITY score 1 and 11.9 months (95% CI 1.57-NA) in patients with CRAFITY score 2, which amounted to a statistically significant difference (p=0.030). The 6-month and 12-month OS rates were 96.3% (95% CI 85.8-99.1) and 89.9% (95% CI 74.3-96.2), respectively, in patients with CRAFITY score 0, 92.3% (95% CI 78.1-97.5) and 58.6% (95% CI 35.7-75.8) in patients with CRAFITY score 1, and 78.7% (95% CI 38.1-94.3) and 39.4% (95% CI 5.9-73.6) in patients with CRAFITY score 2. (b) Overall survival in patients with BCLC advanced and terminal stage according to the CRAFITY score. The median OS was not reached in patients with CRAFITY scores of 0 and 1, while it was 7.6 months (95% CI 4.4-NA) in patients with CRAFITY score of 2; this difference was statistically significant (p<0.001). The 6-month and 12-month OS rates were 92.9% (95% CI 82.1-97.3) and 74.3% (95% CI 51.4-87.6), respectively, in patients with CRAFITY score of 0, 93.3% (95% CI 83.2-97.4) and 67.6% (95% CI 46.8-81.7) in patients with CRAFITY score of 1, and 57.7% (95% CI 35.1-74.9) and 46.6% (95% CI 24.7-65.9) in patients with CRAFITY score of 2. (c) Overall survival in patients receiving Atez/Bev as front line treatment according to the CRAFITY score. The median OS was not reached in patients with CRAFITY scores of 0, 1, and 2. The 6-month and 12-month OS rates were 91.3% (95% CI 81.4-96.1) and 84.9% (95% CI 72.4-92.1), respectively, in patients with CRAFITY score of 0, 93.1% (95% CI 79.6-97.8) and 58.1% (95% CI 29.9-78.4) in patients with CRAFITY score of 1, and 64.8% (95% CI 37.3-82.6) and 56.7% (95% CI 29.0-77.0) in patients with CRAFITY score of 2 (p=0.009). (d) Overall survival in patients receiving Atez/Bev as later line treatment according to the CRAFITY score. The median OS was not reached in patients with CRAFITY scores of 0, while it was 14.3 months (95% CI 10.5-NA) in patients with CRAFITY score of 1 and 11.6 months (95% CI 4.3-NA) in patients with CRAFITY score of 2. The 6-month and 12-month OS rates were 100% (95% CI NA-NA) and 78.2% (95% CI 47.1-92.3), respectively, in patients with CRAFITY score of 0, 92.8% (95% CI 82.0-97.3) and 65.8% (95% CI 47.6-79.0) in patients with CRAFITY score of 1, and 62.3% (95% CI 33.8-81.3) and 26.7% (95% CI 4.8-56.3) in patients with CRAFITY score of 2 (p<0.001).Atez/Bev, atezolizumab and bevacizumab; BCLC, Barcelona Clinic Liver Cancer; CI, confidence interval; CRAFITY score, C-reactive protein and alpha-fetoprotein in immunotherapy; NA, not applicable; OS, overall survival (TIF 1093 KB)
Rights and permissions
About this article
Cite this article
Hatanaka, T., Kakizaki, S., Hiraoka, A. et al. Prognostic impact of C-reactive protein and alpha-fetoprotein in immunotherapy score in hepatocellular carcinoma patients treated with atezolizumab plus bevacizumab: a multicenter retrospective study. Hepatol Int 16, 1150–1160 (2022). https://doi.org/10.1007/s12072-022-10358-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-022-10358-z