Abstract
Background and aims
A consensus of experts suggests that nonalcoholic fatty liver disease (NAFLD) does not appropriately reflect current knowledge and metabolic-associated fatty liver disease (MAFLD) is supposed to be a more suitable overarching concept. However, the association of MAFLD with cardiovascular outcomes in patients with coronary artery disease has not been examined yet. Thus, this study aimed to assess the impact of MAFLD on major adverse cardiac events (MACEs) in patients with chronic coronary syndrome (CCS).
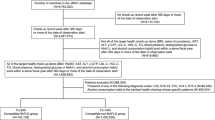
Methods
This study included 3306 patients with CCS who were diagnosed with MAFLD. Controls without MAFLD were matched (1:1) to cases by age and gender. All participants were followed up for the occurrence of MACEs. Finally, the association between MAFLD and the risk of MACEs was assessed.
Results
During an average of 55.09 ± 19.92 months follow-up, 376 and 248 MACEs were observed in MAFLD and control groups, respectively. When compared with controls, Kaplan–Meier analysis showed that patients with MAFLD had significantly lower event-free survival rate and multivariate Cox regression analysis further revealed that MAFLD group had significantly increased MACEs risk (both p < 0.05). Stratification analysis suggested that patients with MAFLD overlapped with NAFLD or MAFLD-only had 1.33-fold and 2.32-fold higher risk of MACEs respectively compared with controls (both p < 0.05).
Conclusion
This study firstly showed that MAFLD was significantly associated with the risk of MACEs in patients with CCS. Moreover, this relationship remained unchanged irrespective of whether satisfying the NAFLD criteria, providing novel evidence for the good utility of MAFLD criteria in clinical practice.
Graphic abstract



Similar content being viewed by others
Availability of data and material
The data that support the findings of this study are available from the corresponding author on reasonable request.
References
Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15(1):11–20 (Epub 2017/09/21)
European Association for the Study of the L, European Association for the Study of D, European Association for the Study of O. EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J |Hepatol. 2016;64(6):1388–1402
Sun DQ, Jin Y, Wang TY, et al. MAFLD and risk of CKD. Metabolism. 2021;115:154433
Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73(1):202–209
Fouad Y, Elwakil R, Elsahhar M, et al. The NAFLD-MAFLD debate: eminence vs evidence. Liver Int. 2021;41(2):255–260
Eslam M, Sanyal AJ, George J, et al. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020;158(7):1999–2014 (Epub 2020/02/12)
Fukunaga S, Nakano D, Kawaguchi T, et al. Non-obese MAFLD is associated with colorectal adenoma in health check examinees: a multicenter retrospective study. Int J Mol Sci. 2021;22(11):5462
Chun HS, Kim MN, Lee JS, et al. Risk stratification using sarcopenia status among subjects with metabolic dysfunction-associated fatty liver disease. J Cachexia Sarcopenia Muscle. 2021. https://doi.org/10.1002/jcsm.12754
Han AL. Association between metabolic associated fatty liver disease and osteoarthritis using data from the Korean national health and nutrition examination survey (KNHANES). Inflammopharmacology. 2021;29(4):1111–1118
Huang Q, Zou X, Wen X, et al. NAFLD or MAFLD: which has closer association with all-cause and cause-specific mortality? Results from NHANES III. Front Med. 2021;8:693507
Guerreiro GTS, Longo L, Fonseca MA, et al. Does the risk of cardiovascular events differ between biopsy-proven NAFLD and MAFLD? Hepatol Int. 2021;15(2):380–391
Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015;62(1 Suppl):S47–S64
Lee H, Lee YH, Kim SU, et al. Metabolic dysfunction-associated fatty liver disease and incident cardiovascular disease risk: a nationwide cohort study. Clin Gastroenterol Hepatol. 2020. https://doi.org/10.1016/j.cgh.2020.12.022
Niriella MA, Ediriweera DS, Kasturiratne A, et al. Outcomes of NAFLD and MAFLD: results from a community-based, prospective cohort study. PLoS ONE. 2021;16(2):e045762
Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–477 (Epub 2019/09/11)
Yamamura S, Eslam M, Kawaguchi T, et al. MAFLD identifies patients with significant hepatic fibrosis better than NAFLD. Liver Int. 2020;40(12):3018–3030
Lee JH, Kim D, Kim HJ, et al. Hepatic steatosis index: a simple screening tool reflecting nonalcoholic fatty liver disease. Digest Liver Dis. 2010;42(7):503–508
George J, Gish RG, Geier A. MAFLD and cardiovascular events: what does the evidence show? Clin Gastroenterol Hepatol. 2021. https://doi.org/10.1016/j.cgh.2021.02.027
Eslam M, Sarin SK, Wong VW, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020;14(6):889–919
Fouad Y, Waked I, Bollipo S, et al. What’s in a name? Renaming “NAFLD” to “MAFLD.” Liver Int. 2020;40(6):1254–1261
The Lancet Gastroenterology H. Redefining non-alcoholic fatty liver disease: what’s in a name? Lancet Gastroenterol Hepatol. 2020;5(5):419
Younossi ZM, Rinella ME, Sanyal AJ, et al. From NAFLD to MAFLD: implications of a premature change in terminology. Hepatology. 2021;73(3):1194–1198
Lin S, Huang J, Wang M, et al. Comparison of MAFLD and NAFLD diagnostic criteria in real world. Liver int. 2020;40(9):2082–2089
Younes R, Bugianesi E. NASH in lean individuals. Semin Liver Dis. 2019;39(1):86–95
Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84
Meffert PJ, Baumeister SE, Lerch MM, et al. Development, external validation, and comparative assessment of a new diagnostic score for hepatic steatosis. Am J Gastroenterol. 2014;109(9):1404–1414
Cumberledge J, Angulo P. Noninvasive prediction of hepatic steatosis. Am J Gastroenterol. 2014;109(9):1415–1416
Acknowledgements
The authors thank all the staff and participants of this study for their important contributions. The data, methods used in the analysis, and materials used to conduct the research will be available to any researcher for purposes of reproducing the results or replicating the procedure from the corresponding author on reasonable request.
Funding
This work was supported by the Capital Health Development Fund (201614035) and CAMS Major Collaborative Innovation Project (2016-I2M-1-011) awarded to JJL, the Fundamental Research Funds for the Central Universities (2019-XHQN09) and the Youth Research Fund of Peking Union Medical College (2019-F11) awarded to HHL. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
HHL participated in research design and data interpretation, obtained funding, and drafted the manuscript; YXC and JLJ participated in data analysis and work revisions; YLG, CGZ, NQW, YG, RXX, and QD conducted the research, collected data and revised the manuscript. MHZ contributed to the research design and manuscript revisions. JJL designed and supervised this study, obtained funding, and made critical revisions of the manuscript. All authors approve the version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors Hui-Hui Liu, Ye-Xuan Cao, Jing-Lu Jin, Yuan-Lin Guo, Cheng-Gang Zhu, Na-Qiong Wu, Ying Gao, Rui-Xia Xu, Qian Dong, Ming-Hua Zheng and Jian-Jun Li declare that they have no conflict of interest.
Ethics approval
All procedures performed in this study involving human participants were approved by the hospital’s ethical review board (FuWai Hospital & National Center for Cardiovascular Diseases, Beijing, China) and complied with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all individual participants included in the study.
Consent to publication
All authors give final approval of the version to be published, and agree to be accountable for all aspects of the work.
Code availability
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, HH., Cao, YX., Jin, JL. et al. Metabolic-associated fatty liver disease and major adverse cardiac events in patients with chronic coronary syndrome: a matched case–control study. Hepatol Int 15, 1337–1346 (2021). https://doi.org/10.1007/s12072-021-10252-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-021-10252-0