Abstract
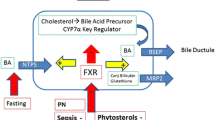
Premature infants and children with intestinal failure (IF) or short bowel syndrome are susceptible to intestinal failure-associated liver disease (IFALD, previously referred to as parenteral nutrition-associated liver disease, or PNALD). IFALD in children is characterized by progressive cholestasis and biliary fibrosis, and steatohepatitis in adults, and is seen in individuals dependent upon prolonged administration of PN. Many factors have been proposed as contributing to the pathogenesis of IFALD. In recent years, the focus has been on the potential synergistic roles of the intestinal microbiome, increased intestinal permeability, activation of hepatic innate immune pathways, and the use of intravenous soybean-oil-based intravenous lipid emulsions (SO-ILE). In vitro and in vivo studies have identified stigmasterol, a component of the plant sterols present in SO-ILE, as playing an important role. Although various strategies have been adopted to prevent or reverse IFALD, most suffer from a lack of strong evidence supported by well-designed, prospective clinical trials with clearly defined endpoints. Reduction in the amount of SO-ILEs or replacement with non-SO-ILEs has been shown to reverse IFALD although safety and long-term effectiveness have not been studied. Medical and surgical modalities to increase intestinal adaptation, advance enteral feedings, and prevent central line bloodstream infections are also important preventative strategies. There is a continued need to conduct high-quality, prospective trials with clearly define outcome measures to ascertain the potential benefits of these strategies.
Similar content being viewed by others
References
Duggan CP, Jaksic T. Pediatric intestinal failure. New Engl J Med 2017;377:666–675
Abi Nader E, Lambe C, Talbotec C, Pigneur B, Lacaille F, Garnier-Lengliné H, et al. Outcome of home parenteral nutrition in 251 children over 14-year period: report of a single center. Am J Clin Nutri 2016;103:1327–1336
Lee WS, Sokol RJ. Intestinal microbiota, lipids, and the pathogenesis of intestinal failure-associated liver disease. J Pediatr 2016;167:519–526
Javid PJ, Oron AP, Duggan C, Squires RH, Horslen SP. The extent of intestinal failure-associated liver disease in patients referred for intestinal rehabilitation is associated with increased mortality: an analysis of the pediatric intestinal failure consortium database. J Pediatr Surg 2017;1:1. https://doi.org/10.1016/j.pedsurg.2017.08.049
Lauriti G, Zani A, Aufieri R, Cananzi M, Chiesa PL, Eaton S, et al. Incidence, prevention, and treatment of parenteral nutrition-associated cholestasis and intestinal failure-associated liver disease in infants and children: a systematic review. JPEN J Parenter Enteral Nutr 2014;38:70–85
Pironi L, Joly F, Forbes A, Colomb V, Lyszkowska M, Baxter J, Gabe S, et al. Long-term follow-up of patients on home parenteral nutrition in Europe: implications for intestinal transplantation. Gut 2011;60:17–25
Lauriti G, Zani A, Aufieri R, Cananzi M, Chiesa PL, Eaton S, Pierro A. Incidence, prevention, and treatment of parenteral nutrition-associated cholestasis and intestinal failure-associated liver disease in infants and children: a systematic review. JPEN J Parenter Enteral Nutri 2014;38:70–85
Robinson DT, Ehrenkranz RA. Parenteral nutrition-associated cholestasis in small for gestational age infants. J Pediatr 2008;152:59–62
Norsa L, Nicastro E, Di Giorgio A, Lacaille F, D'Antiga L. Prevention and treatment of intestinal failure-associated liver disease in children. Nutrients 2018;10(6):1
Yeop I, Taylor CJ, Narula P, Johnson L, Bowen C, Gupte GL. Hepatocellular carcinoma in a child with intestinal failure-associated liver disease. J Pediatr Gastroenterol Nutr 2012;54:695–697
Spencer AU, Neaga A, West B, Safran J, Brown P, Btaiche I, Kuzma-O'Reilly B, Teitelbaum DH. Pediatric short bowel syndrome: redefining predictors of success. Ann Surg 2005;242:403–409
Christensen RD, Henry E, Weidmeier SE, Burnett J, Lambert DK. Identifying patients, on the first day of life, at high risk of developing parenteral nutrition-associated liver disease. J Perinatol 2007;27:284–290
Costa S, Maggio L, Sindico P, Cota F, De Carolis MP, Romagnoli C. Preterm small for gestational age infants are not at higher risk for parenteral nutrition-associated cholestasis. J Pediatr 2010;156:575–579
Duro D, Mitchell PD, Kalish LA, et al. Risk factors for parenteral nutrition-associated liver disease following surgical therapy for necrotizing enterocolitis. J Pediatr Gastroenterol Nutri 2011;52:595–600
Bishay M, Pichler J, Horn V, Macdonald S, Ellmer M, Eaton S, et al. Intestinal failure-associated liver disease in surgical infants requiring long-term parenteral nutrition. J Pediatr Surg 2012;47:359–362
Javid PJ, Malone FR, Dick AAS, Hsu E, Sunseri M, Healey P, Horslen S. A contemporary analysis of parenteral nutrition-associated liver disease in surgical infants. J Pediatr Surg 2011;46:1913–1917
Sanchez SE, Braun LP, Mercer LD, Sherill M, Stevens J, Javid PJ. The effect of lipid restriction on the prevention of parenteral nutrition- associated cholestasis in surgical infants. J Pediatr Surg 2013;48:573–578
Pichler J, Horn V, Macdonald S, Hill S. Intestinal failure-associated liver disease in hospitalized children. Arch Dis Child 2012;97:211–214
Cavicchi M, Beau P, Crenn P, Degott C, Messing B. Prevalence of liver disease and contributing factors in patients receiving home parenteral nutrition for permanent intestinal failure. Ann Intern Med 2000;132:525–532
Huard G, Fiel MI, Moon J, Iyer K, Schiano TD. Prevalence, evolution, and risk factors for advanced liver fibrosis in adults undergoing intestinal transplantation. JPEN J Parenter Enteral Nutr 2018. https://doi.org/10.1002/jpen.1148
Zambrano E, El-Hennawy M, Ehrenkranz RA, Zelterman D, Reyes-Mugica M. Total parenteral nutrition-induced liver pathology: an autopsy series of 24 newborn cases. Pediatr Develop Pathol 2004;7:425–432
Cohen C, Olsen MM. Pediatric total parenteral nutrition. Liver Histopathol Arch Pathol Lab Med 1981;105:152–156
Moss RL, Das JB, Raffensperger JG. Total parenteral nutrition-associated cholestasis: clinical and histopathologic correlation. J Pediatr Surg 1993;28:1270–1274
Mutanen A, Lohi J, Heikkila P, Koivusalo AI, Rintala RJ, Pakarinen MP. Persistent abnormal liver fibrosis after weaning off parenteral nutrition in pediatric intestinal failure. Hepatology 2013;58:729–738
Mutanen A, Lohi J, Sorsa T, Jalanko H, Pakarinen MP. Features of liver tissue remodeling in intestinal failure during and after weaning off parenteral nutrition. Surgery 2016;160:632–642
Fullerton BS, Sparks EA, Hall AM, Duggan C, Jaksic T, Modi BP. Enteral autonomy, cirrhosis, and long-term transplant-free survival in pediatric intestinal failure patients. J Pediatr Surg 2016;51:96–100
Wales PW, Aleen N, Worthington P, Compher C, Tietelbaum D. A.S.P.E.N. Clinical Guidelines: support of pediatric patients with intestinal failure at risk of parenteral nutrition-associated liver disease. J Parenter Enteral Nutr 2014;38:538–557
Muhammed R, Bremner R, Protheroe S, Johnson T, Holden C, Murphy MS. Resolution of parenteral nutrition-associated jaundice on changing from a soybean oil emulsion to a complex mixed-lipid emulsion. J Pediatr Gastroenterol Nutri 2012;54:797–802
Cahova M, Bratova WP. Parenteral nutrition-associated liver disease: the role of the gut microbiota. Nutrients 2017;9:987. https://doi.org/10.3390/nu9090987
Hermans D, Talbotec C, Lacaille F, Goulet O, Ricour C, Colomb V. Early central catheter infections may contribute to hepatic fibrosis in children receiving long-term parenteral nutrition. J Pediatr Gastroenterol Nutri 2007;44:459–463
El Kasmi KC, Anderson AL, Devereaux MW, Fillon SA, Harris KT, Lowell MA, et al. Toll-like receptor 4-dependent Kupffer cell activation and liver injury in a novel mouse model of parenteral nutrition and intestinal injury. Hepatology 2012;55:1518–1528
El Kasmi KC, Anderson AL, Devereaux MW, Vue PM, Zhang W, Setchell KD, et al. Phytosterols promote liver injury and Kupffer cell activation in parenteral nutrition-associated liver disease. Sci Transl Med 2013;5(206):137
Kaufman SS, Loseke CA, Lupo JV, Young RJ, Murray ND, et al. Influence of bacterial overgrowth and intestinal inflammation on duration of parenteral nutrition in children with short bowel syndrome. J Pediatr 1997;131:356–361
Harris JK, El Kasmi KC, Anderson AL, Devereaux MW, Fillon SA, Robertson CE, Wagner BD, Stevens MJ, Pace NR, Sokol RJ. Specific microbiome changes in a mouse model of parenteral nutrition induced liver injury and intestinal inflammation. PLoS ONE 2014;9(10):e110396
Wang P, Wang Y, Lu L, Yan W, Tao Y, Zhou K, et al. Alterations in intestinal microbiota relate to intestinal failure-associated liver disease and central line infections. J Pediatr Surg 2017;52:1318–1326
Nandivada P, Cowan E, Carlson SJ, Chang M, Gura KM, Puder M. Mechanisms for the effects of fish oil lipid emulsions in the management of parenteral nutrition-associated liver disease. Prostaglandins Leukot Essent Fatty Acids 2013;89:153–158
Mutanen A, Lohi J, Heikkila P, Jalanko H, Pakarinen MP. Liver inflammation relates to decreased canalicular bile transporter expression in pediatric onset intestinal failure. Ann Surg 2018;268:332–329
El Kasmi KC, Vue PM, Anderson AL, Devereaux MW, Ghosh S, Balasubramaniyan N, et al. Macrophage-derived IL-1β/NFκB signalling mediates parenteral nutrition-associated cholestasis. Nat Commun 2018;9:1393
Norsa L, Nicastro E, Di Giorgio A, Lacaille F, D’Antiga L. Prevention and treatment of intestinal failure-associated liver disease in children. Nutrients 2018;10:664. https://doi.org/10.3390/nu10060664
Demehri FR, Stephens L, Herrman E, West B, Mehringer A, et al. Enteral autonomy in pediatric short bowel syndrome: predictive factors one year after diagnosis. J Pediatr Surg 2015;50:131–135
Mercer DF, Hobson BD, Gerhardt BK, Grant WJ, Vargas LM, Langnas AN, Quiros-Tejeira RE. Serial transverse enteroplasty allows children with short bowel to wean from parenteral nutrition. J Pediatr 2014;164:93–98
Kocoshis SA, Merritt RJ, Hill S, Protheroe S, Carter BA, Horslen S, Hu S, Kaufman SS, Mercer DF, Pakarinen MP, Venick RS, Wales PW, Grimm AA. Safety and efficacy of teduglutide in pediatric patients with intestinal failure due to short bowel syndrome: a 24-week, phase III study. JPEN J Parenter Enteral Nutr 2019;1:1. https://doi.org/10.1002/jpen.1690
Lim DW, Wales PW, Josephson JK, Nation PN, Wizzard PR, Sergi CM, Turner JM, et al. Glucagon-like peptide 2 improves cholestasis in parenteral nutrition-associated liver disease. JPEN J Parenter Enteral Nutr 2016;40:22–35
Slagle TA, Gross SJ. Effect of early low-volume enteral substrate on subsequent tolerance in very low birth weight infants. J Pediatr 1988;113:526–531
Oliveira C, Nasr A, Brindle M, Wales PW. Ethanol locks to prevent catheter-related bloodstream infections in parenteral nutrition: a meta-analysis. Pediatrics 2012;129:318–329
Rollins MD, Ward RM, Jackson WD, et al. Effect of decreased parenteral soybean lipid emulsion on hepatic function in infants at risk for parenteral nutrition-associated liver disease: a pilot study. J Pediatr Surg 2013;48:1348–1356
Diamond IR, de Silva NT, Tomlinson GA, Pencharz PB, Feldman BM, Moore AM, Ling SC, Wales PW. The role of parenteral lipids in the development of advanced intestinal failure-associated liver disease in infants: a multiple-variable analysis. JPEN J Parenter Enteral Nutr 2011;35:596–602
Nehra D, Fallon EM, Carlson SJ, Potemkin A, Hevelone ND, Mitchell PD, et al. Provision of a soy-based intravenous lipid emulsion at 1 g/kg/d does not prevent cholestasis in neonates. JPEN J Parenter Enteral Nutr 2013;37:498–505
Levit OL, Calkins KL, Gibson LC, Kelley-Quon L, Robinson DT, Elashoff DA, et al. Low-dose intravenous soybean oil emulsion for prevention of cholestasis in preterm neonates. JPEN J Parenter Enteral Nutr 2016;40:374–382
Josephson J, Turner JM, Field CJ, Wizzard PR, Nation PN, Sergi C, et al. Parenteral soy oil and fish oil emulsions: impact of dose restriction on bile flow and brain size of parenteral nutrition-fed neonatal piglets. JPEN J Parenter Enteral Nutr 2015;39:677–687
Schneider J, Fischer Fumeaux CJ, Duerden EG, Guo T, Foong J, Graz MB, et al. Nutrient intake in the first two weeks of life and brain growth in preterm neonates. Pediatrics 2018;1:1. https://doi.org/10.1542/peds.2017-2169(Epub ahead of print)
de Meijer VE, Gura KM, Le HD, Meisel JA, Puder M. Fish-oil based lipid emulsions prevent and reverse parenteral nutrition-associated liver dis- ease: the Boston experience. JPEN J Parenter Enteral Nutr 2009;33:541–547
Zhang T, Wang N, Yan W, Lu L, Tao Y, Li F, Wang Y, Cai W. Effect of a fish oil-based lipid emulsion on intestinal failure-associated liver disease in children. Eur J Clin Nutr 2018;72:1364–1372
Nehra D, Fallon EM, Potemkin AK, Voss SD, Mitchell PD, Valim C, et al. A comparison of 2 intravenous lipid emulsions: interim analysis of a randomized controlled trial. JPEN J Parenter Enteral Nutr 2014;38:693–701
Park HW, Lee NM, Kim JH, Kim KS, Kim SN. Parenteral fish oil-containing lipid emulsions may reverse parenteral nutrition-associated cholestasis in neonates: a systematic review and analysis. J Nutr 2015;145:277–283
Khan FA, Fisher JG, Sparks EA, Potemkin A, Duggan C, Raphael BP, et al. Preservation of biochemical liver function with low-dose soy-based lipids in children with intestinal failure-associated liver disease. JPEN J Parenter Enteral Nutr 2015;60:375–377
Raphael BP, Mitchell PD, Gura KM, Potemkin AK, Squires RH, Puder M, Duggan CP. Growth in infants and children with intestinal failure associated-liver disease treated with intravenous fish oil. J Pediatr Gastroenterol Nutr 2019;1:1. https://doi.org/10.1097/MPG.0000000000002551(Epub ahead of print)
Ong ML, Venick RS, Shew SB, Dunn JCY, Reyen L, Grogan T, Calkins KL. Intravenous fish oil and serum fatty acid profiles in pediatric patients with intestinal failure-associated liver disease. JPEN J Parenter Enteral Nutr 2019;43:717–725
Repa A, Binder C, Thanhaeuser M, Kreissl A, Pablik E, Huber-Dangl M, Berger A, Haiden N. A mixed lipid emulsion for prevention of parenteral nutrition associated cholestasis in extremely low birth weight infants: a randomized clinical trial. J Pediatr 2018;194:87–93
Lee S, Park HJ, Yoon J, Hong SH, Oh CY, Lee SK, et al. Reversal of intestinal-failure associated liver disease by switching from a combination lipid emulsion containing fish oil to fish oil monotherapy. JPEN J Parenter Enteral Nutr 2016;40:437–440
Bin-Nun A, Kassirer Y, Mimouni FB, Shchors I, Hammerman C. Head circumference growth is enhanced by SMOFlipid in preterm neonates. Am J Perinatol 2019. https://doi.org/10.1055/s-0039-1692390(Epub ahead of print)
Soden JS, Lovell MA, Brown K, Patrick DA, Sokol RJ. Failure of resolution of portal fibrosis during omega-3 fatty acid lipid emulsion therapy in two patients with irreversible intestinal failure. J Pediatr 2010;156:327–331
Kappor V, Malviya MN, Soll R. Lipid emulsions for parenterally fed preterm infants. Cochrane Database Syst Rev 2019;6:CD013163. https://doi.org/10.1002/14651858.CD013163.pub2
Seida JC, Mager DR, Hartling L, Vandermeer B, Turner JM. Parenteral u-3 fatty acid lipid emulsions for children with intestinal failure and other conditions: systematic review. JPEN J Parenter Enteral Nutri 2013;37:44–55
Lacaille F, Gupte G, Colomb V, D’Antiga L, Hartman C, Hojsak I, et al. Intestinal failure-associated liver disease: a position paper of the ESPGHAN working group of intestinal failure and intestinal transplantation. J Pediatr Gastroenterol Nutr 2015;60:272–283
Li J, Gong YM, Wu J, Wu WJ, Cai W. Anti-tumor necrosis factor-α monoclonal antibody alleviates parenteral nutrition-associated liver disease in mice. JPEN J Parenter Enteral Nutri 2012;36:219–225
Neuschwander-Tetri BA, Loomba R, Sanyal AJ, Lavine JE, Van Natta ML, et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randominsed, placebo-controlled trial. Lancet 2015;385(9972):956–956
El Kasmi KC, Ghosh S, Anderson AL, Devereaux MW, Balasubramaniyan N, Johnson L, Haines JR, Suchy FJ, D’Alessandro A, Sokol RJ. FXR agonist GW4064 prevents parenteral nutrition-associated cholestasis (PNAC) in mice. Hepatology 2017;66(Suppl 1):58A–9A
Ganousse-Mazeron S, Lacaille F, Colombo-Jung V, Talbotec C, Ruemmele F, Sauvat F, et al. Assessment and outcome of children with intestinal failure referred for intestinal transplantation. Clin Nutri 2015;34:428–435
Fiel MI, Sauter B, Wu HS, Rodriguez-Laiz G, Gondolesi G, Iyer K, Schiano TD. Regression of hepatic fibrosis after intestinal transplantation in total parenteral nutrition liver disease. Clin Gastroenterol Hepatol 2008;6:926–933
Hawksworth JS, Desai CS, Khan KM, Kaufman SS, Yazigi N, Girlanda R, et al. Visceral transplantation in patients with intestine-failure associated liver disease: evolving indications, graft selection, and outcome. Am J Transplant 2018;18:1312–1320
Acknowledgements
Ronald J. Sokol receives funding from the National Institutes of Health (UL1TR002535, T32 DK067009, and U01DK062453). Dr. Sokol would also like to thank the members of his laboratory team (Karim El Kasmi, Michael Devereaux, Aimee Anderson, Swati Ghosh, and Padade Vue) and other collaborators for work discussed in this review.
Funding
Ronald J. Sokol received funding from the National Institutes of Health (UL1TR002535, U01DK062453, T32 DK067009). None of the authors received any honorarium, grant, or other form of payment in the process of the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared. Way S Lee wrote the first draft of the manuscript. All the authors have seen and approved the submission of this version of the manuscript and take full responsibility for the manuscript. No honorarium or other form of payment was given to anyone to produce the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, W.S., Chew, K.S., Ng, R.T. et al. Intestinal failure-associated liver disease (IFALD): insights into pathogenesis and advances in management. Hepatol Int 14, 305–316 (2020). https://doi.org/10.1007/s12072-020-10048-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-020-10048-8