Abstract
Background and aims
Non-alcoholic fatty liver disease (NAFLD) commonly affects subjects with obesity, yet non-obese NAFLD is increasingly being recognized. We aimed to investigate the clinicopathological and genetic characteristics of non-obese NAFLD patients.
Methods
The clinical, histological and genetic data of 84 NAFLD patients with biopsy for abnormal liver function test were reviewed. Both NAS-CRN and SAF scoring systems were applied for histopathological evaluation. PNPLA3 and TMS6F2 genotyping were also performed.
Results
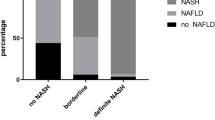
All of the 84 patients were histologically diagnosed with non-alcoholic steatohepatitis (NASH), with 36 of them (42.9%) being non-obese (BMI < 25 kg/m2). Compared with the obese group, non-obese group were predominantly females (88.9% vs 52.1%, p < 0.001), tended to have higher prevalence of diabetes (p = 0.068). More importantly non-obese patients had a significant higher prevalence of advanced fibrosis (F ≥ 3) (58.3% vs 29.2%, p = 0.013), and a trend of higher degree of ballooning (p = 0.061). In addition, values of liver stiffness measurement were also significantly higher in non-obese group (12.1 kPa vs 8.1 kPa, p = 0.032). There was also a trend of higher prevalence of TM6SF2 T allele in non-obese group (p = 0.085), while the prevalence of PNPLA3 risk allele did not differ between two groups. Multivariate analysis showed that higher fasting glucose (p = 0.038) and lower serum platelets (p = 0.040) were two independent predictors for advanced fibrosis in non-obese patients.
Conclusions
Non-obese NASH patients have a female predominance and more advanced fibrosis. Liver biopsy is crucial to evaluate the severity of disease in non-obese patients especially those with abnormal liver biochemistry.
Clinical trial number
NCT03386890.




Similar content being viewed by others
Abbreviations
- NAFLD:
-
Non-alcoholic fatty liver disease
- NASH:
-
Non-alcoholic steatohepatitis
- MetS:
-
Metabolic syndrome
- BMI:
-
Body mass index
- PNPLA3 :
-
Polymorphisms of patatin-like-phospholipase domain-containing protein 3
- TM6SF2 :
-
Transmembrane 6 superfamily antigen 2
- WC:
-
Waist circumference
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- ALP:
-
Alkaline phosphatase
- GGT:
-
γ-Glutamyltransferase
- CHE:
-
Cholinesterase
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- TG:
-
Triglycerides
- UA:
-
Uric acid
- PTA:
-
Prothrombin activity
- HOMA-IR:
-
Homeostatic model assessment insulin resistance
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- FPG:
-
Fasting plasma glucose
- LSM:
-
Liver stiffness measurements
- CAP:
-
Controlled attenuation parameter
- H&E:
-
Hematoxylin and eosin
- NASH CRN:
-
NASH Clinical Research Network
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- TE:
-
Transient elastography
References
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84.
Kim D, Kim WR. Nonobese fatty liver disease. Clin Gastroenterol Hepatol. 2017;15:474–85.
Assy N, Nasser G, Kamayse I, Nseir W, Beniashvili Z, Djibre A, et al. Soft drink consumption linked with fatty liver in the absence of traditional risk factors. Can J Gastroenterol. 2008;22:811–6.
Enjoji M, Yasutake K, Kohjima M, Nakamuta M. Nutrition and nonalcoholic Fatty liver disease: the significance of cholesterol. Int J Hepatol. 2012;2012:925807.
Wei JL, Leung JC, Loong TC, Wong GL, Yeung DK, Chan RS, et al. Prevalence and severity of nonalcoholic fatty liver disease in non-obese patients: a population study using proton-magnetic resonance spectroscopy. Am J Gastroenterol. 2015;110:1306–14 (quiz 1315).
Vos B, Moreno C, Nagy N, Fery F, Cnop M, Vereerstraeten P, et al. Lean non-alcoholic fatty liver disease (Lean-NAFLD): a major cause of cryptogenic liver disease. Acta Gastroenterol Belg. 2011;74:389–94.
Leung JC, Loong TC, Wei JL, Wong GL, Chan AW, Choi PC, et al. Histological severity and clinical outcomes of nonalcoholic fatty liver disease in nonobese patients. Hepatology. 2017;65:54–64.
Margariti A, Deutsch M, Manolakopoulos S, Tiniakos D, Papatheodoridis GV. The severity of histologic liver lesions is independent of body mass index in patients with nonalcoholic fatty liver disease. J Clin Gastroenterol. 2013;47:280–6.
Dela Cruz AC, Bugianesi E, George J, Day CP, Liaquat H, Charatcharoenwitthaya P, et al. Characteristics and long-term prognosis of lean patients with nonalcoholic fatty liver disease. Gastroenterology. 2014;146:S-909.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, Zenere MB, et al. Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care. 2000;23:57–63.
Heng D, Ma S, Lee JJ, Tai BC, Mak KH, Hughes K, et al. Modification of the NCEP ATP III definitions of the metabolic syndrome for use in Asians identifies individuals at risk of ischemic heart disease. Atherosclerosis. 2006;186:367–73.
Sasso M, Beaugrand M, de Ledinghen V, Douvin C, Marcellin P, Poupon R, et al. Controlled attenuation parameter (CAP): a novel VCTE guided ultrasonic attenuation measurement for the evaluation of hepatic steatosis: preliminary study and validation in a cohort of patients with chronic liver disease from various causes. Ultrasound Med Biol. 2010;36:1825–35.
Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21.
Bedossa P, Poitou C, Veyrie N, Bouillot JL, Basdevant A, Paradis V, et al. Histopathological algorithm and scoring system for evaluation of liver lesions in morbidly obese patients. Hepatology. 2012;56:1751–9.
Akyuz U, Yesil A, Yilmaz Y. Characterization of lean patients with nonalcoholic fatty liver disease: potential role of high hemoglobin levels. Scand J Gastroenterol. 2015;50:341–6.
Honda Y, Yoneda M, Kessoku T, Ogawa Y, Tomeno W, Imajo K, et al. Characteristics of non-obese non-alcoholic fatty liver disease: effect of genetic and environmental factors. Hepatol Res. 2016;46:1011–8.
Kumar R, Rastogi A, Sharma MK, Bhatia V, Garg H, Bihari C, et al. Clinicopathological characteristics and metabolic profiles of non-alcoholic fatty liver disease in Indian patients with normal body mass index: do they differ from obese or overweight non-alcoholic fatty liver disease? Indian J Endocrinol Metab. 2013;17:665–71.
Hagstrom H, Nasr P, Ekstedt M, Hammar U, Stal P, Hultcrantz R, et al. Risk for development of severe liver disease in lean patients with nonalcoholic fatty liver disease: a long-term follow-up study. Hepatol Commun. 2018;2:48–57.
Nishioji K, Sumida Y, Kamaguchi M, Mochizuki N, Kobayashi M, Nishimura T, et al. Prevalence of and risk factors for non-alcoholic fatty liver disease in a non-obese Japanese population, 2011–2012. J Gastroenterol. 2015;50:95–108.
Das K, Das K, Mukherjee PS, Ghosh A, Ghosh S, Mridha AR, et al. Nonobese population in a developing country has a high prevalence of nonalcoholic fatty liver and significant liver disease. Hepatology. 2010;51:1593–602.
Cho HC. Prevalence and factors associated with nonalcoholic fatty liver disease in a nonobese Korean population. Gut Liver. 2016;10:117–25.
Sinn DH, Gwak GY, Park HN, Kim JE, Min YW, Kim KM, et al. Ultrasonographically detected non-alcoholic fatty liver disease is an independent predictor for identifying patients with insulin resistance in non-obese, non-diabetic middle-aged Asian adults. Am J Gastroenterol. 2012;107:561–7.
Kim D, Chung GE, Kwak MS, Seo HB, Kang JH, Kim W, et al. Body fat distribution and risk of incident and regressed nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2016;14(132–138):e134.
Yang JD, Abdelmalek MF, Pang H, Guy CD, Smith AD, Diehl AM, et al. Gender and menopause impact severity of fibrosis among patients with nonalcoholic steatohepatitis. Hepatology. 2014;59:1406–14.
Liu YL, Reeves HL, Burt AD, Tiniakos D, McPherson S, Leathart JB, et al. TM6SF2 rs58542926 influences hepatic fibrosis progression in patients with non-alcoholic fatty liver disease. Nat Commun. 2014;5:4309.
Acknowledgements
This study was funded by Beijing Municipal Administration of Hospitals Clinical Medicine Development of special funding support (XMLX201606), The Digestive Medical Coordinated Development Center of Beijing Municipal Administration of Hospitals (XXZ03) and Research Foundation of Beijing Friendship Hospital, Capital Medical University (yyqdkt2017-8).
Author information
Authors and Affiliations
Contributions
Study design: JJ, RS, ASHG, HY. Data collection: QW, MW, XO, YW, WD, XW. Liver biopsy assessment: XZ, RS, ASHG. Statistical analysis: QW, YS, YK, SW. Manuscript writing: QW. Genotype analysis: PW, QW, MW. Critical revision of the manuscript: HY, JJ, RS, ASHG.
Corresponding authors
Ethics declarations
Conflict of interest
Qianyi Wang, Hong You, Xiaojuan Ou, Xinyan Zhao, Yameng Sun, Min Wang, Ping Wang, Yu Wang, Weijia Duan, Xiaoming Wang, Shanshan Wu, Yuanyuan Kong, Romil Saxena, Annette S. H. Gouw, Jidong Jia declare that they have no conflicts of interest.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by the institutional Ethics Committee (Ethical approval no. 2015-P2-070-01). All patients signed informed consent for liver biopsy and blood sample storage.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Romil Saxena, Annette S. H. Gouw and Jidong Jia share co-corresponding authorship.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, Q., You, H., Ou, X. et al. Non-obese histologically confirmed NASH patients with abnormal liver biochemistry have more advanced fibrosis. Hepatol Int 13, 766–776 (2019). https://doi.org/10.1007/s12072-019-09982-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-019-09982-z