Abstract
Background and aims
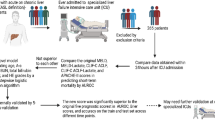
Acute-on-chronic liver failure (ACLF) is a progressive disease associated with rapid clinical worsening and high mortality. Early prediction of mortality and intervention can improve patient outcomes. We aimed to develop a dynamic prognostic model and compare it with the existing models.
Methods
A total of 1402 ACLF patients, enrolled in the APASL-ACLF Research Consortium (AARC) with 90-day follow-up, were analyzed. An ACLF score was developed in a derivation cohort (n = 480) and was validated (n = 922).
Results
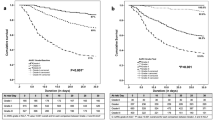
The overall survival of ACLF patients at 28 days was 51.7%, with a median of 26.3 days. Five baseline variables, total bilirubin, creatinine, serum lactate, INR and hepatic encephalopathy, were found to be independent predictors of mortality, with AUROC in derivation and validation cohorts being 0.80 and 0.78, respectively. AARC-ACLF score (range 5–15) was found to be superior to MELD and CLIF SOFA scores in predicting mortality with an AUROC of 0.80. The point scores were categorized into grades of liver failure (Gr I: 5–7; II: 8–10; and III: 11–15 points) with 28-day cumulative mortalities of 12.7, 44.5 and 85.9%, respectively. The mortality risk could be dynamically calculated as, with each unit increase in AARC-ACLF score above 10, the risk increased by 20%. A score of ≥11 at baseline or persisting in the first week was often seen among nonsurvivors (p = 0.001).
Conclusions
The AARC-ACLF score is easy to use, dynamic and reliable, and superior to the existing prediction models. It can reliably predict the need for interventions, such as liver transplant, within the first week.



Similar content being viewed by others
Abbreviations
- AARC:
-
APASL ACLF research consortium
- ACLF:
-
Acute-on-chronic liver failure
- HAV:
-
Hepatitis A virus
- HCC:
-
Hepato-cellular carcinoma
- HEV:
-
Hepatitis E virus
- HBV:
-
Hepatitis B virus
- SAH:
-
Severe alcoholic hepatitis
- TJLB:
-
Trans-jugular liver biopsy
References
Sarin SK, Choudhury A. Acute-on-chronic liver failure: terminology, mechanisms and management. Nat Rev Gastroenterol Hepatol 2016;13(3):131–149
Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, Durand F, For CANONIC Study Investigators of the EASL–CLIF Consortium, et al. Acute on chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 2013;144:1426–1437
Sarin SK, Kedarisetty CK, Abbas Z, Amarapurkar D, Bihari C, Chan AC, For APASL ACLF Working Party, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific Association for the study of the liver (APASL). Hepatol Int 2014;8:453–471
Jalan R, Saliba F, Pavesi M, Amoros A, Moreau R, Ginès P, Levesque E, Durand F, For CANONIC study investigators of the EASL-CLIF Consortium, et al. Development and validation of a prognostic score to predict mortality in patients with acute-on-chronic liver failure. J Hepatol 2014;61(5):1038–1047
Garg H, Kumar A, Garg V, Sharma P, Sharma BC, Sarin SK. Clinical profile and predictors of mortality in patients of acute-on-chronic liver failure. Dig Liver Dis 2012;44(2):166–171
Agrawal S, Duseja A, Gupta T, Dhiman RK, Chawla Y. Simple organ failure count versus CANONIC grading system for predicting mortality in acute-on-chronic liver failure. J Gastroenterol Hepatol 2015;30(3):575–581
Sarin SK, Choudhury A. Acute-on-chronic liver failure. CurrGastroenterol Rep 2016;18(12):61 (Review)
Wang ZX, Yan LN, Wang WT, Xu MQ, Yang JY. Impact of pretransplant MELD score on post transplant outcome in orthotropic liver transplantation for patients with acute-on-chronic hepatitis B liver failure. Transplant Proc 2007;39:15011504
Jalan R, Pavesi M, Saliba F, Amorós A, Fernandez J, Holland-Fischer P, For CANONIC Study Investigators; EASL-CLIF Consortium, et al. The CLIF Consortium Acute Decompensation score (CLIF-C ADs) for prognosis of hospitalised cirrhotic patients without acute-on-chronic liver failure. J Hepatol 2015;62(4):831–840
Yang WB, Chen EQ, Bi HX, Bai L, Chen XB, Feng P, Tang H. Different models in predicting the short-term prognosis of patients with hepatitis B virus-related acute-on-chronic liver failure. Ann Hepatol 2012;11(3):311–319
Cordoba J, Ventura-Cots M, Simón-Talero M, Amorós À, Pavesi M, Vilstrup H, Angeli P, Domenicali M, Ginés P, Bernardi M, Arroyo V, CANONIC Study Investigators of EASL-CLIF Consortium. Characteristics, risk factors, and mortality of cirrhotic patients hospitalized for hepatic encephalopathy with and without acute-on-chronic liver failure (ACLF). J Hepatol. 2014;60(2):275–281
Levesque E, Winter A, Noorah Z, Daurès JP, Landais P, Feray C, Azoulay D. Impact of acute-on-chronic liver failure on 90-day mortality following a first liver transplantation. Liver Int 2017;. doi:10.1111/liv.13355
Jeppesen JB, Mortensen C, Bendtsen F, Møller S. Lactate metabolism in chronic liver disease. Scand J Clin Lab Invest 2013;73(4):293–299
Cardoso NM, Silva T, Basile-Filho A, Mente ED, Castro-e-Silva O. A new formula as a predictive score of post-liver transplantation outcome: postoperative MELD-lactate. Transplant Proc 2014;46(5):1407–1412
Huo TI, Lin HC, Wu JC, Lee FY, Hou MC, Lee PC, Chang FY, et al. Proposal of a modified Child-Turcotte-Pugh scoring system and comparison with the model for end-stage liver disease for outcome prediction in patients with cirrhosis. Liver Transplant 2006;12(1):65–71
Shi Y, Yang Y, Hu Y, Wu W, Yang Q, Zheng M, Zhang S, et al. Acute-on-chronic liver failure precipitated by hepatic injury is distinct from that precipitated by extrahepatic insults. Hepatology 2015;62(1):232–242
Moon DB, Lee SG, Kang WH, Song GW, Jung DH, Park GC, Cho HD, et al. Adult living donor liver transplantation for acute-on-chronic liver failure in high- model for end-stage liver disease score patients. Am J Transplant. 2017;17(7):1833–1842.
Gustot T, Fernandez J, Garcia E, Morando F, Caraceni P, Alessandria C, Laleman W, For CANONIC Study Investigators of the EASL-CLIF Consortium, et al. Clinical course of acute-on-chronic liver failure syndrome and effects on prognosis. Hepatology 2015;62(1):243–252
Zheng MH, Wu SJ, Shi KQ, Yan HD, Li H, Zhu GQ, Xie YY et al. Conditional survival estimate of acute-on-chronic hepatitis B liver failure: a dynamic prediction based on a multicenter cohort. Oncotarget 2015;6(27):23261–2371
Zabor EC, Gonen M, Chapman PB, Panageas KS. Dynamic prognostication using conditional survival estimates. Cancer 2013;119:3589–3592
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval of the institutional ethics committees was obtained.
Informed consent
Informed consent was taken from the patient or the next of kin.
Financial disclosures
None.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
The study was approved by institute ethical committee vide letter no F/25/5/64/AC2013/912 and the respective centers also had their own ethical board approval for the study to be carried out. The centers, investigators and the number of patients contibuted are listed as follows:
Center no. | Name | Country/center | Total patients |
|---|---|---|---|
1 | Dr. Shiv K Sarin | ILBS, India | 1286 |
5 | Dr. Mamun-Al Mahtab | Bangladesh | 145 |
6 | Dr. Yogesh Chawala | Chandigarh | 128 |
9 | Dr. Tan SS | Malaysia | 109 |
3 | Dr. Harshad Devarbhavi | Bangalore | 103 |
2 | Dr. Zhongping Duan | Beijing | 98 |
21 | Dr. Qin Ning, Jidong Jia, | China | 96 |
14 | Dr. Deepak Naryan | Bombay Hospital | 76 |
4 | Dr. Eapen | Vellore | 72 |
8 | Dr. Saeed Hamid | Karachi, Pakistan | 69 |
22 | Dr. Kim et.al. | Republic of Korea | 68 |
13 | Dr. Hasmik | Armenia | 50 |
10 | Dr. Guan Huei Lee | Singapore | 39 |
7 | Dr. Ajit sood | Ludhiana, India | 34 |
12 | Dr. Laurentius A. Lesmana | Indonesia | 28 |
17 | Dr. Zaigham Abbas | Pakistan | 25 |
23 | Dr. Gamal Shiha | Egypt | 25 |
11 | Dr. Diana Alcantara-Payawal | Philippines | 21 |
20 | Dr. A. Kadir Dokmeci | Turkey | 19 |
16 | Dr. Jose | Philippines | 12 |
24 | Dr. Man-Fung Yuen | Hong Kong | 12 |
15 | Dr. George K Lau | China | 10 |
18 | Dr. Fazal Karim | Bangladesh | 6 |
19 | Dr. P N Rao | Hyderabad, India | 4 |
Total | 2535 | ||
Complete data for analysis | 1402 | ||
Rights and permissions
About this article
Cite this article
Choudhury, A., Jindal, A., Maiwall, R. et al. Liver failure determines the outcome in patients of acute-on-chronic liver failure (ACLF): comparison of APASL ACLF research consortium (AARC) and CLIF-SOFA models. Hepatol Int 11, 461–471 (2017). https://doi.org/10.1007/s12072-017-9816-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-017-9816-z