Abstract
Aims
The aim of this study is to evaluate the effect of Positive End Expiratory Pressure (PEEP) on surgical field bleeding and its respiratory and hemodynamic consequences in rhinoplasty surgeries.
Materials and methods
This single-blind clinical trial performed in Amir Al-Momenin university Hospital in 2018. Seventy cases of rhinoplasty surgery patients Enrolled and were randomized into two groups; intervention (PEEP = 5) and comparison group (PEEP = 0). Surgical field bleeding and arterial oxygen saturation pulmonary dynamics and hemodynamic parameters were evaluated during operation and in post anesthesia care unit. Data were analyzed by SPSS software using descriptive and analytical statistics.
Results
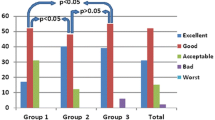
PEEP applying had no negative effect on surgical bleeding as well as surgeon satisfaction, heart rate and blood pressure were similar in two groups. Pulmonary dynamics and oxygenation were stable and within normal values in all cases. The mean peak airway pressure was 17.87 ± 2.24 in the PEEP group and 16.08 ± 3.37 in the ZEEP group (P = 0.029).
Conclusion
applying low level PEEP during anesthesia improved recovery oxygen saturation but had no negative effects on the patient`s hemodynamics, and did not aggravate bleeding and visual clarity.
Similar content being viewed by others
References
Ebrahimi A, Kalantar Motamedi MH, Shams A, Nejadsarvari N (2016) Health and social problems of rhinoplasty in Iran. World J Plast Surg 5(1):75–76
Rastmanesh R, Gluck ME, Shadman Z (2009) Comparison of body dissatisfaction and cosmetic rhinoplasty with levels of veil practicing in islamic women. Int J Eat Disord 42(4):339–345
Ozkose M, Baykan H, Coşkuner İ (2016) The effect of patient positioning on amount of intraoperative bleeding in rhinoplasty: a randomized controlled trial. Aesthetic Plast Surg 40(4):453–457
Flint PW, Haughey BH, Robbins KT, Thomas JR, Niparko JK, Lund VJ et al (2014) Cummings otolaryngology-head and neck surgery e-book. Elsevier Health Sciences
Nikoyan L, Matthews S (2012) Epistaxis and hemostatic devices. Oral and Maxillofacial Surgery Clinics 24(2):219–228
Sieskiewicz A, Olszewska E, Rogowski M, Grycz E (2006) Preoperative corticosteroid oral therapy and intraoperative bleeding during functional endoscopic sinus surgery in patients with severe nasal polyposis: a preliminary investigation. Annals of Otology, Rhinology & Laryngology. ;115(7):490-4
Tirelli G, Bigarini S, Russolo M, Lucangelo U, Gullo A (2004) Total intravenous anaesthesia in endoscopic sinus-nasal surgery. Acta Otorhinolaryngol Ital 24:137–144
Futier E, Constantin J-M, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A et al (2013) A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 369(5):428–437
Karsten J, Heinze H, Meier T (2014) Impact of PEEP during laparoscopic surgery on early postoperative ventilation distribution visualized by electrical impedance tomography. Minerva Anestesiol 80(2):158
Bajwa SJS, Kaur J, Kulshrestha A, Haldar R, Sethi R, Singh A (2016) Nitroglycerine, esmolol and dexmedetomidine for induced hypotension during functional endoscopic sinus surgery: a comparative evaluation. J Anaesthesiol Clin Pharmacol 32(2):192
Webster AC, Morley-Forster PK, Janzen V, Watson J, Dain SL, Taves D et al (1999) Anesthesia for intranasal surgery: a comparison between tracheal intubation and the flexible reinforced laryngeal mask airway. Anesth Analgesia 88(2):421–425
Hall RI, Smith MS, Rocker G (1997) The systemic inflammatory response to cardiopulmonary bypass: pathophysiological, therapeutic, and pharmacological considerations. Anesth Analgesia 85(4):766–782
Dorinsky PM, Whitcomb ME (1983) The effect of PEEP on cardiac output. Chest 84(2):210–216
Tusman G, Böhm S, de Anda GV, Do Campo J, Lachmann B (1999) Alveolar recruitment strategy’improves arterial oxygenation during general anaesthesia. Br J Anaesth 82(1):8–13
Auler J Jr, Carmona M, Barbas C, Saldiva P, Malbouisson L (2000) The effects of positive end-expiratory pressure on respiratory system mechanics and hemodynamics in postoperative cardiac surgery patients. Braz J Med Biol Res 33(1):31–42
Niazi M, POURMIRZA KR (2003) The effect of positive end expiratory pressure on incidence rate of atelectasis after coronary artery bypass graft.
Golparvar M, Abbasi S, Jazi SK (2013) The Effects of different levels of positive end-expiratory pressure on hemodynamic and respiratory indexes in patients with healthy and damaged lungs.Journal of Isfahan Medical School. ; 31(239)
DeMaria S, Govindaraj S, Huang A, Hyman J, McCormick P, Lin HM et al (2015) The influence of positive end-expiratory pressure on surgical field conditions during functional endoscopic sinus surgery. Anesth Analgesia 120(2):305–310
Güldner A, Kiss T, Neto AS, Hemmes SN, Canet J, Spieth PM et al (2015) Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complicationsa comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. J Am Soc Anesthesiologists 123(3):692–713
Neuschwander A, Futier E, Jaber S, Pereira B, Eurin M, Marret E et al (2016) The effects of intraoperative lung protective ventilation with positive end-expiratory pressure on blood loss during hepatic resection surgery: a secondary analysis of data from a published randomised control trial (IMPROVE). Eur J Anaesthesiol (EJA) 33(4):292–298
Ingaramo OA, Ngo T, Khemani RG, Newth CJ (2014) Impact of positive end-expiratory pressure on cardiac index measured by ultrasound cardiac output monitor. Pediatr Crit Care Medicine| Soc Crit Care Med 15(1):15–20
Sarge T, Loring SH, Yitsak-Sade M, Malhotra A, Novack V, Talmor D (2014) Raising positive end-expiratory pressures in ARDS to achieve a positive transpulmonary pressure does not cause hemodynamic compromise. Intensive Care Med 40(1):126–128
D’Antini D, Huhle R, Herrmann J, Sulemanji DS, Oto J, Raimondo P et al (2018) Respiratory system mechanics during low versus high positive end-expiratory pressure in open abdominal surgery: a substudy of PROVHILO randomized controlled trial. Anesth Analg 126(1):143
Kwak HJ, Park SK, Lee KC, Lee DC, Kim JY (2013) High positive end-expiratory pressure preserves cerebral oxygen saturation during laparoscopic cholecystectomy under propofol anesthesia. Surg Endosc 27(2):415–420
Neto AS, Rabello Filho R, Cherpanath T, Determann R, Dongelmans DA, Paulus F et al (2016) Associations between positive end-expiratory pressure and outcome of patients without ARDS at onset of ventilation: a systematic review and meta-analysis of randomized controlled trials. Ann Intensiv Care 6(1):109
Acknowledgements
We are especially grateful to all the experts who were an integral partner in the preparation of facilities.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Habibi, A.F., Ashraf, A., Ghanavi, Z. et al. Positive End-Expiratory Pressure in Rhinoplasty Surgery; Risks and Benefits. Indian J Otolaryngol Head Neck Surg 75, 2823–2828 (2023). https://doi.org/10.1007/s12070-023-03854-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-03854-7