Abstract
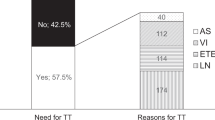
Papillary thyroid carcinoma (PTC) contributes to 88% of thyroid malignancies and its extent of surgical management has been a topic of debate in the past 2 decades. American thyroid association (ATA) recommendations have been periodically updated for its robust and evidence-based management. We present our experience in implementing 2015 ATA guidelines, assessment of surgical outcomes of hemithyroidectomy in PTC ≤ 4 cm and contemplating on the potential clinical implications of 2015 ATA guidelines. A prospective study in a cohort of Bethesda class V and VI PTC with nodule ≤ 4 cm who underwent Hemithyroidectomy between 2012 and 2020. Data on thyroid nodule evaluation, management, histopathology and follow up were used for risk stratification. Of 37 patients, 27 (72.9%) were low risk and 10 (37%) were intermediate risk ATA group. 4 (40%) intermediate risk patients had structural incomplete response and underwent completion thyroidectomy. 1 (2.7%) out of 4 completion surgery patients required adjuvant radio-ablation iodine (RAI) and 3 patients were under surveillance. Overall, 2 (5.4%) of 37 patients, 1 each from low and intermediate groups were given remnant RAI in view of aggressive histology, old age and unwillingness for a completion surgery. During follow up of 4.94 ± 2.4 years, 35 (94.5%) showed excellent response and 2 (5.4%) showed biochemical incomplete response. The difference in RFS between two groups was statistically significant with p < 0.001. Thyroid preserving surgery combined with real time risk stratification seems appropriate for low and intermediate risk PTC ≤ 4 cm.




Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Sherman SI (2003) Thyroid carcinoma. Lancet. 361(9356):501–511
Vaisman F, Momesso D, Bulzico DA, Pessoa CH, da Cruz MDG, Dias F et al (2013) Thyroid lobectomy is associated with excellent clinical outcomes in properly selected differentiated thyroid cancer patients with primary tumors greater than 1 cm. J Thyroid Res 2013:398194
Kuba S, Yamanouchi K, Hayashida N, Maeda S, Adachi T, Sakimura C et al (2017) Total thyroidectomy versus thyroid lobectomy for papillary thyroid cancer: comparative analysis after propensity score matching: a multicenter study. Int J Surg 38:143–148
Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedus L et al (2010) American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and european thyroid Association Medical guidelines for clinical practice for the diagnosis and management of thyroid nodules: executive summary of recommendations. Endocr Pract 16(3):468–475
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ et al (2009) Revised american thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19(11):1167–1214
Mendelsohn AH, Elashoff DA, Abemayor E, St John MA (2010) Surgery for papillary thyroid carcinoma: is lobectomy enough? Arch Otolaryngol Head Neck Surg 136:1055–106111
Adam MA, Pura J, Gu L, Dinan MA, Tyler DS, Reed SD et al (2014) Extent of surgery for papillary thyroid cancer is not associated with survival: an analysis of 61,775 patients. Ann Surg 260(4):601–605
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE et al (2016) 2015 American thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the american thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1):1–33
Cibas ES, Ali SZ (2009) The Bethesda system for reporting thyroid cytopathology. Thyroid 19(11):1159–1165
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ et al (2006) Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 16(2):109–142
Rahbari R, Zhang L, Kebebew E (2010) Thyroid cancer gender disparity. Future Oncol 6(11):1771–1779
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM (2014) Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 74(11):2913–2921
Cetta F, Montalto G, Gori M, Curia MC, Cama A, Olschwang S (2000) Germline mutations of the APC gene in patients with familial adenomatous polyposis-associated thyroid carcinoma: results from a European cooperative study. J Clin Endocrinol Metab 85(1):286–292
Mankarios D, Baade P, Youl P, Mortimer RH, Onitilo AA, Russell A et al (2014) Validation of the QTNM staging system for cancer-specific survival in patients with differentiated thyroid cancer. Endocrine 46(2):300–308
Surks MI, Ortiz E, Daniels GH, Sawin CT, Col NF, Cobin RH et al (2004) Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA 291(2):228–238
Ahn D, Lee GJ, Sohn JH, Jeon JH (2020) Oncological impact of hypothyroidism and levothyroxine supplementation following hemithyroidectomy in patients with papillary thyroid carcinoma. Head Neck 42(5):1004–1013
Brassard M, Borget I, Edet-Sanson A, Giraudet AL, Mundler O, Toubeau M et al (2011) Long-term follow-up of patients with papillary and follicular thyroid cancer: a prospective study on 715 patients. J Clin Endocrinol Metab 96(5):1352–1359
Momesso DP, Vaisman F, Yang SP, Bulzico DA, Corbo R, Vaisman M et al (2016) Dynamic risk stratification in patients with differentiated thyroid cancer treated without radioactive iodine. J Clin Endocrinol Metab 101(7):2692–2700
Trimboli P, La Torre D, Ceriani L, Condorelli E, Laurenti O, Romanelli F et al (2013) High sensitive thyroglobulin assay on thyroxine therapy: can it avoid stimulation test in low and high risk differentiated thyroid carcinoma patients? Horm Metab Res 45(9):664–668
Horvath E, Majlis S, Rossi R, Franco C, Niedmann JP, Castro A et al (2009) An ultrasonogram reporting system for thyroid nodules stratifying cancer risk for clinical management. J Clin Endocrinol Metab 94(5):1748–1751
Redman R, Yoder BJ, Massoll NA (2006) Perceptions of diagnostic terminology and cytopathologic reporting of fine-needle aspiration biopsies of thyroid nodules: a survey of clinicians and pathologists. Thyroid 16(10):1003–1008
Bernstein JM, Shah M, McMillan C, Freeman JL (2016) Institution-specific risk of papillary thyroid carcinoma in atypia/follicular lesion of undetermined significance. Head Neck 38(Suppl1):E1210–E1215
Nikiforov YE, Steward DL, Robinson-Smith TM, Haugen BR, Klopper JP, Zhu Z et al (2009) Molecular testing for mutations in improving the fine-needle aspiration diagnosis of thyroid nodules. J Clin Endocrinol Metab 94(6):2092–2098
Collet JF, Lacave R, Hugonin S, Poulot V, Tassart M, Fajac A (2016) BRAF V600E detection in cytological thyroid samples: a key component of the decision tree for surgical treatment of papillary thyroid carcinoma. Head Neck 38(7):1017–1021
Lesnik D, Cunnane ME, Zurakowski D, Acar GO, Ecevit C, Mace A et al (2014) Papillary thyroid carcinoma nodal surgery directed by a preoperative radiographic map utilizing CT scan and ultrasound in all primary and preoperative patients. Head Neck 36(2):191–202
Haugen BR (2015) American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: What is new and What has changed? Cancer. 123(3):372 –3 81
Abdul-Sater L, Henry M, Majdan A, Mijovic T, Franklin JH, Brandt MG et al (2011) What are thyroidectomy patients really concerned about? Otolaryngol Head Neck Surg 144:685–6905
Soylu L, Ozbas S, Uslu HY, Kocak S (2007) The evaluation of the causes of subjective voice disturbances after thyroid surgery. Am J Surg 194(3):317–322
De Carlucci D Jr, Tavares MR, Obara MT, Martins LA, Hojaij FC, Cernea CR (2008) Thyroid function after unilateral total lobectomy: risk factors for postoperative hypothyroidism. Arch Otolaryngol Head Neck Surg. 134(10):1076–1079
Gupta K, Panda NK, Jain P, Bakshi J, Verma R (2015) Hypothyroidism after hemithyroidectomy for colloid goiter: is it a reality. Thyroid Res Pract 12:107–109
Zhang C, Li Y, Li J, Chen X (2020) Total thyroidectomy versus lobectomy for papillary thyroid cancer: a systematic review and meta-analysis. Medicine 99(6):e19073
Acknowledgements
None.
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethics Approval
Institutional ethics committee approval was taken prior to beginning of the study with approval number “NK/7071/Study/130”.
Consent to Participate
A verbal consent of the patient and/or their guardian was taken at every step of investigation and treatment.
Consent for Publication
A verbal Consent was taken for use of patient’s treatment related data for academic use and publication on the condition of anonymity.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rathod, R., Panda, N.K., Bakshi, J. et al. Hemithyroidectomy in Papillary Thyroid Cancers: A Prospective, Single Institutional Surgical Audit and Contemplating on the Clinical Implications of 2015 American Thyroid Association Guidelines. Indian J Otolaryngol Head Neck Surg 75, 508–516 (2023). https://doi.org/10.1007/s12070-022-03312-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03312-w