Abstract
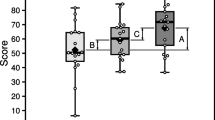
Nijmegen Cochlear Implant Questionnaire is an HRQoL tool that was developed by Dutch researchers to assess the QoL in adult CI users in the English language. It is used to measure the impact of the use of CI on the daily life situations of its users, on the perception of speech sounds, and on the cost–benefit assessment CI in adult CI users. There is no specific instrument available to assess the QoL in adult CI users in India, hence there was a need to take up this study. The primary aim of the study was to adapt and translate NCIQ into Hindi with a secondary aim to describe the effect of CI on quality of life in adult CI users. For translation, permission was taken from the authors of the original tool. The Forward-backward translation method was utilized for translation. The final version of the NCIQ-H was administered to the study participants (25 no.) 25, aged 18–60 years; High School as the minimum level of education; post-lingual hearing impairment, and CI use ≥ 12 months. The Cronbach’s α coefficient was calculated for all domains and subdomains in the NCIQ-H showed the overall reliability of the questionnaire (0.82), showing good internal consistency. The CI users reported high scores across all the domains indicating improved quality of life. No significant correlation was found between the CI usage time and NCIQ scores on Spearman’s correlation test. Also, there was no significant difference in NCIQ-H scores between genders on the Kruskal–Wallis test. The NCIQ (H) can be used to assess QoL in adults with cochlear implants. The scores suggest improvement in physical, social and psychological domains of life. No correlation was observed between the NCIQ-H scores and duration of CI usage as well as with gender differences.

Similar content being viewed by others

References
GBD Disease Injury Incidence Prevalence Collaborators (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the global burden of disease study 2015. The Lancet 388:1545–602
World Health Organization. Deafness and hearing loss [Online]. Available https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss(2020) Accessed: 06-Sep-2020
WHO. World Report on hearing. https://apps.who.int/iris/bitstream/handle/10665/339913/9789240020481-eng.pdf?sequence=1. Accessed date 26 Mar 2021
Davis A, McMahon CM, Pichora-Fuller KM, Russ S, Lin F, Olusanya BO, Chadha S, Tremblay K (2016) Aging and hearing health: the life-course approach. Gerontologist 56(Suppl 2):S256–S267
Genther DJ, Frick KD, Chen D, Betz J, Lin FR (2013) Association of hearing loss with hospitalization and burden of disease in older adults. JAMA 309:2322–2324
Contrera KJ, Betz J, Genther DJ, Lin FR (2015) Association of hearing impairment and mortality in the national health and nutrition examination survey. JAMA Otolaryngol Head Neck Surg 141:944–946
Fisher D, Li CM, Chiu MS et al (2014) Impairments in hearing and vision impact on mortality in older people: the AGES- Reykjavik study. Age Ageing 43:69–76
Lin FR, Ferrucci L (2012) Hearing loss and falls among older adults in the United States. Arch Intern Med 172:369–371
Viljanen A, Kaprio J, Pyykko I et al (2009) Hearing as a predictor of falls and postural balance in older female twins. J Gerontol A Biol Sci Med Sci 64:312–317
Lin FR, Metter EJ, O’Brien RJ, Resnick SM, Zonderman AB, Ferrucci L (2011) Hearing loss and incident dementia. Arch Neurol 68:214–220
Lin FR, Yaffe K, Xia J et al (2013) Hearing loss and cognitive decline in older adults. JAMA Intern Med 173:293–299
Gallacher J, Ilubaera V, Ben-Shlomo Y et al (2012) Auditory threshold, phonologic demand, and incident dementia. Neurology 79:1583–1590
Li CM, Zhang X, Hoffman HJ, Cotch MF, Themann CL, Wilson MR (2014) Hearing impairment associated with depression in US adults, national health and nutrition examination survey 2005–2010. JAMA Otolaryngol Head Neck Surg 140:293–302
Mener DJ, Betz J, Genther DJ, Chen D, Lin FR (2013) Hearing loss and depression in older adults. J Am Geriatr Soc 61:1627–1629
Holden LK, Finley CC, Firszt JB, Holden TA, Brenner C, Potts LG et al (2013) Factors affecting open-set word recognition in adults with cochlear implants. Ear Hear 34(3):342–60
Blamey P, Artieres F, Başkent D, Bergeron F, Beynon A, Burke E et al (2013) Factors affecting the auditory performance of postlinguistically deaf adults using cochlear implants: an update with 2251 patients. Audiol Neurotol 18(1):36–47
Green KM, Bhatt Y, Mawman DJ, O’Driscoll MP, Saeed SR, Ramsden RT et al (2007) Predictors of audiological outcome following cochlear implantation in adults. Cochlear Implants Int 8(1):1–11
Rubinstein JT (2012) Cochlear implants: the hazards of unexpected success. Can Med Assoc J 184(12):1343–4. https://doi.org/10.1503/cmaj.111743
Black J, Hickson l, Black B (2012) Defining and evaluating success in pediatric cochlear implantation—an exploratory study. Int J Audiol 76(9):131726
WHO (1998) The World Health Organization quality of life assessment (WHOQOL): development and general psychometric properties. Soc Sci Med 46(12):1569–85
Hinderink JB, Krabbe PFM, Broek PVD (2000) Development and application of a health-related quality-of-life instrument for adults with cochlear implants: the Nijmegen cochlear implant questionnaire. Otolaryngol Head Neck Surg 123(6):756–65. https://doi.org/10.1067/mhn.2000.108203
Lassaletta L, Castro A, Bastarrica M, Sarria MJ, Gavila J (2006) Quality of life in postlingually deaf patients following cochlear implantation. Eur Arch Otorhinolaryngol 263(3):267–70. https://doi.org/10.1007/s00405-005-0987-1
Damen GWJA, Pennings RJE, Snik AFM, Mylanus EAM (2006) Quality of life and cochlear implantation in Usher syndrome type I. Laryngoscope. 116(5):723–8. https://doi.org/10.1097/01.mlg.0000205128.86063.17
Klop WMC, Boermans PPBM, Ferrier MB, Hout WBVD, Stiggelbout AM, Frijns JHM (2008) Clinical relevance of quality of life outcome in cochlear implantation in postlingually deafened adults. Otol Neurotol 29(5):615–21. https://doi.org/10.1097/MAO.0b013e318172cfac
Vermeire K, Brokx JPL, Wuyts FL, Cochet E, Hofkens A, Van de Heyning PH (2005) Quality-of-life benefit from cochlear implantation in the elderly. Otol Neurotol 26(2):188–95. https://doi.org/10.1097/00129492-200503000-00010
Sparreboom M, Snik FM, Mylanus EAM (2012) Sequential bilateral cochlear implantation in children. Arch Otolaryngol Head Neck Surg 138(2):134–41. https://doi.org/10.1001/archoto.2011.229
Krabbe PFM, Hinderink JB, Broek P (2000) The effect of cochlear implant use in postlingually deaf adults. Int J Technol Assess Health Care 16(3):864–73. https://doi.org/10.1017/S0266462300102132
Ottaviani F, Iacona E, Sykopetrites V, Schindler A, Mozzanica F (2016) Crosscultural adaptation and validation of the Nijmegen Cochlear Implant Questionnaire into Italian. Eur Arch Otorhinolaryngol 273(8):2001–7. https://doi.org/10.1007/s00405-015-3765-8
Sanchez-Cuadrado I, Gavilan J, Perez-Mora R, Muñoz E, Lassaletta L (2015) Reliability and validity of the Nijmegen Cochlear implant questionnaire in Spanish. Eur Arch Otorhinolaryngol 272(7):1621–5. https://doi.org/10.1007/s00405-014-2983-9
Dong RJ, Liu B, Peng XX, Chen XQ, Gong SS (2010) Analysis of reliability and validity of the Chinese version of Nijmegen cochlear implant questionnaire. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 45(10):818–23
Kosugi EM, Chen VG, Fonseca VMG, Cursino MMP, Neto JAM, Gregório LC (2011) Tradução, adaptação cultural e validação do questionário sinonasal outcome test (SNOT)—22 para a Língua portuguesa (BR). Rev Bras Otorrinolaringol 77(5):663–669
Sanchez-Cuadrado I, Gavilan J, Perez-Mora R, Muñoz E, Lassaletta L (2015) Reliability and validity of the Nijmegen Cochlear implant questionnaire in Spanish. Eur Arch Otorhinolaryngol 272(7):1621–5. https://doi.org/10.1007/s00405-014-2983-9
Olze H, Szczepek AJ, Haupt H, Förster U, Zirke N, Gräbel S et al (2011) Cochlear implantation has a positive influence on quality of life, tinnitus, and psychological comorbidity. Laryngoscope 121(10):2220–7. https://doi.org/10.1002/lary.22145
Rumeau C, Frère J, Montaut-Verient B, Lion A, Gauchard G, Parietti-Winkler C (2015) Quality of life and audiologic performance through the ability to phone of cochlear implant users. Eur Arch Otorhinolaryngol 272(12):3685–92. https://doi.org/10.1007/s00405-014-3448-x
Damen GW, Beynon AJ, Krabbe PF, Mulder JJ, Mylanus EA (2007) Cochlear implantation and quality of life in postlingually deaf adults: long-term followup. Otolaryngol Head Neck Surg 136(4):597–604. https://doi.org/10.1016/j.otohns.2006.11.044
Klop WM, Briaire JJ, Stiggelbout AM, Frijns JH (2007) Cochlear implant outcomes and quality of life in adults with prelingual deafness. Laryngoscope 117(11):1982–7. https://doi.org/10.1097/MLG.0b013e31812f56a6
Louza J, Hempel JM, Krause E, Berghaus A, Müller J, Braun T, Braun T (2017) Patient benefit from Cochlear implantation in single-sided deafness: a 1-year follow-up. Eur Arch Otorhinolaryngol 274(6):2405–9. https://doi.org/10.1007/s00405-017-4511-1
Damen GWJA, Pennings RJE, Snik AFM, Mylanus EAM (2006) Quality of life and cochlear implantation in Usher syndrome type I. Laryngoscope 116(5):723–8. https://doi.org/10.1097/01.mlg.0000205128.86063.17
Krabbe PFM, Hinderink JB, Broek P (2000) The effect of cochlear implant use in postlingually deaf adults. Int J Technol Assess Health Care 16(3):864–73. https://doi.org/10.1017/S0266462300102132
Hirschfelder A, Grabel S, Olze H (2008) The impact of cochlear implantation on quality of life: the role of audiologic performance and variables. Otolaryngol Head Neck Surg 138(3):357–62. https://doi.org/10.1016/j.otohns.2007.10.019
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human or Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (PGIMER Ethical Committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alam, N., Munjal, S.K., Panda, N.K. et al. Translation and Adaptation of the Nijmegen Cochlear Implant Questionnaire in Hindi: A Health-Related Quality of Life Questionnaire for Adults with Cochlear Implants. Indian J Otolaryngol Head Neck Surg 75 (Suppl 1), 121–126 (2023). https://doi.org/10.1007/s12070-022-03306-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03306-8