Abstract
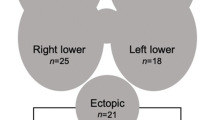
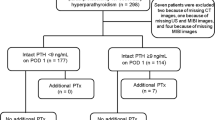
The aim of our study is to assess the feasibility, safety and adequacy of focused parathyroidectomy for single parathyroid adenoma accurately localized preoperatively by ultrasound neck and Tc99m sestamibi scan. The study was conducted in the department of Otorhinolaryngology of SMS Medical College and Hospital, Jaipur on 116 patients of primary hyperparathyroidism who underwent minimally invasive parathyroidectomy (MIP) for single gland adenoma localized by USG neck and tc99m sestamibi scans. S. Calcium and S. PTH followed up on day 1, 6th week and 6th month. Outcomes were determined on the basis of cure rate, duration of hospitalization, complication rates and disease persistence/recurrence rate. 82 (70.68%) females and 34 (29.31%) males belonging to the age group of 21–67 years (43.02 ± 14) formed the basis of our study. Skeletal (73.27%) and renal (62.93%) were the most common presentations. Accuracy of USG and sestamibi accurately was 93.10% and 96.55% respectively with combined accuracy of 100%. Preoperative serum calcium levels of 10.7–16.03 mg/dl (13.09 ± 2.11) and serum PTH 127–2196 pg/ml (846.57 ± 776.55) were observed. Cure rate of MIP was 99.13%. No permanent complications seen. MIP can be used as the surgical procedure of choice for PHPT caused by single gland adenoma aided by USG and sestamibi scan. The cure rates are equivalent to the bilateral neck exploration (> 95%) with minimal morbidity and complications. Hence, it is a more feasible, safe and effective treatment option.


Similar content being viewed by others
References
Pyram R, Mahajan G, Gliwa A (2011) Primary hyperparathyroidism: skeletal and non-skeletal effects, diagnosis and management. Maturitas 70(3):246–255. https://doi.org/10.1016/j.maturitas.2011.07.021
Cordellat IM (2012) Hyperparathyroidism: primary or secondary disease? Reumatol Clin 8(5):287–291. https://doi.org/10.1016/j.reuma.2011.06.001
Fraser WD (2009) Hyperparathyroidism. Lancet 374(9684):145–158. https://doi.org/10.1016/S0140-6736(09)60507-9
Liu JM, Cusano NE, Silva BC, Zhao L, He XY, Tao B, Sun LH, Zhao HY, Fan WW, Romano ME, Ning G, Bilezikian JP (2013) Primary Hyperparathyroidism: a tale of two cities revisited—New York and Shanghai. Bone Res 1(2):162–169. https://doi.org/10.4248/BR201302005
Reiher AE, Mazeh H, Schaefer S, Gould J, Chen H, Sippel RS (2012) Symptoms of gastroesophageal reflux disease improve after parathyroidectomy. Surgery 152(6):1232–1237. https://doi.org/10.1016/j.surg.2012.08.051
Pallan S, Rahman MO, Khan AA (2012) Diagnosis and management of primary hyperparathyroidism. BMJ 19(344):e1013. https://doi.org/10.1136/bmj.e1013
Rubin MR, Bilezikian JP, McMahon DJ, Jacobs T, Shane E, Siris E, Udesky J, Silverberg SJ (2008) The natural history of primary hyperparathyroidism with or without parathyroid surgery after 15 years. J Clin Endocrinol Metab 93(9):3462–3470. https://doi.org/10.1210/jc.2007-1215
Madkhali T, Alhefdhi A, Chen H, Elfenbein D (2016) Primary hyperparathyroidism. Ulus Cerrahi Derg 32(1):58–66. https://doi.org/10.5152/UCD.2015.3032
Calò PG, Pisano G, Loi G, Medas F, Barca L, Atzeni M, Nicolosi A (2013) Intraoperative parathyroid hormone assay during focused parathyroidectomy: the importance of 20 minutes measurement. BMC Surg 18(13):36. https://doi.org/10.1186/1471-2482-13-36
Silverberg SJ, Shane E, Jacobs TP, Siris E, Bilezikian JP (1999) A 10-year prospective study of primary hyperparathyroidism with or without parathyroid surgery. N Engl J Med 341(17):1249–1255. https://doi.org/10.1056/NEJM199910213411701 (Erratum in: N Engl J Med 2000 Jan13;342(2):144)
Pradeep PV, Jayashree B, Mishra A, Mishra SK (2011) Systematic review of primary hyperparathyroidism in India: the past, present, and the future trends. Int J Endocrinol 2011:921814. https://doi.org/10.1155/2011/921814
Mishra SK, Agarwal G, Kar DK, Gupta SK, Mithal A, Rastad J (2001) Unique clinical characteristics of primary hyperparathyroidism in India. Br J Surg 88(5):708–714. https://doi.org/10.1046/j.0007-1323.2001.01775.x
Khan AA, Hanley DA, Rizzoli R, Bollerslev J, Young JE, Rejnmark L, Thakker R, D’Amour P, Paul T, Van Uum S, Shrayyef MZ, Goltzman D, Kaiser S, Cusano NE, Bouillon R, Mosekilde L, Kung AW, Rao SD, Bhadada SK, Clarke BL, Liu J, Duh Q, Lewiecki EM, Bandeira F, Eastell R, Marcocci C, Silverberg SJ, Udelsman R, Davison KS, Potts JT Jr, Brandi ML, Bilezikian JP (2017) Primary hyperparathyroidism: review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporos Int 28(1):1–19. https://doi.org/10.1007/s00198-016-3716-2
Grant CS, Thompson G, Farley D, van Heerden J (2005) Primary hyperparathyroidism surgical management since the introduction of minimally invasive parathyroidectomy: Mayo Clinic experience. Arch Surg 140(5):472–478. https://doi.org/10.1001/archsurg (discussion 478–9)
Udelsman R (2002) Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg 235(5):665–670. https://doi.org/10.1097/00000658-200205000-00008 (discussion 670–2)
Pradeep PV, Mishra A, Agarwal G, Agarwal A, Verma AK, Mishra SK (2008) Long-term outcome after parathyroidectomy in patients with advanced primary hyperparathyroidism and associated vitamin D deficiency. World J Surg 32(5):829–835. https://doi.org/10.1007/s00268-007-9384-9
Usta A, Alhan E, Cinel A, Türkyılmaz S, Erem C (2015) A 20-year study on 190 patients with primary hyperparathyroidism in a developing country: Turkey experience. Int Surg 100(4):648–655. https://doi.org/10.9738/INTSURG-D-14-00094.1
Yadav SK, Mishra SK, Mishra A, Mayilvagnan S, Chand G, Agarwal G, Agarwal A, Verma AK (2019) Surgical management of primary hyperparathyroidism in the era of focused parathyroidectomy: a study in tertiary referral Centre of North India. Indian J Endocrinol Metab 23(4):468–472. https://doi.org/10.4103/ijem.IJEM_255_19
Bhansali A, Masoodi SR, Reddy KS, Behera A, das Radotra B, Mittal BR, Katariya RN, Dash RJ (2005) Primary hyperparathyroidism in north India: a description of 52 cases. Ann Saudi Med 25(1):29–35. https://doi.org/10.5144/0256-4947.2005.29
Jinih M, O’Connell E, O’Leary DP, Liew A, Redmond HP (2017) Focused versus bilateral parathyroid exploration for primary hyperparathyroidism: a systematic review and meta-analysis. Ann Surg Oncol 24(7):1924–1934. https://doi.org/10.1245/s10434-016-5694-1
Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA (2012) A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol 19(2):577–583. https://doi.org/10.1245/s10434-011-1870-5
Haber RS, Kim CK, Inabnet WB (2002) Ultrasonography for preoperative localization of enlarged parathyroid glands in primary hyperparathyroidism: comparison with (99m)technetium sestamibi scintigraphy. Clin Endocrinol (Oxf) 57(2):241–249. https://doi.org/10.1046/j.1365-2265.2002.01583.x
Johnson NA, Tublin ME, Ogilvie JB (2007) Parathyroid imaging: technique and role in the preoperative evaluation of primary hyperparathyroidism. AJR Am J Roentgenol 188(6):1706–1715. https://doi.org/10.2214/AJR.06.0938
Norman J, Chheda H, Farrell C (1998) Minimally invasive parathyroidectomy for primary hyperparathyroidism: decreasing operative time and potential complications while improving cosmetic results. Am Surg 64(5):391–395 (discussion 395–6)
Goldstein RE, Blevins L, Delbeke D, Martin WH (2000) Effect of minimally invasive radioguided parathyroidectomy on efficacy, length of stay, and costs in the management of primary hyperparathyroidism. Ann Surg 231(5):732–742. https://doi.org/10.1097/00000658-200005000-00014
Quinn AJ, Ryan ÉJ, Garry S, James DL, Boland MR, Young O, Kerin MJ, Lowery AJ (2021) Use of Intraoperative parathyroid hormone in minimally invasive parathyroidectomy for primary hyperparathyroidism: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg 147(2):135–143. https://doi.org/10.1001/jamaoto.2020.4021
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All the authors declare that they have no conflict of Interest.
Ethical Approval
All procedures performed in study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent
Informed consent was obtained from all the participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rawat, A., Grover, M., Kataria, T. et al. Minimally Invasive Parathyroidectomy as the Surgical Management of Single Parathyroid Adenomas: A Tertiary Care Experience. Indian J Otolaryngol Head Neck Surg 75, 271–277 (2023). https://doi.org/10.1007/s12070-022-03236-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03236-5