Abstract
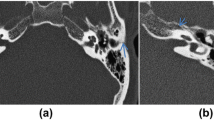
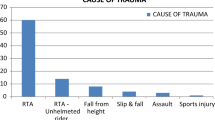
To address the management of complications after temporal bone fractures and the outcomes. A prospective clinical study of 100 patients from the Department of Trauma (Surgery + E.N.T.), P.D.U. Medical College, Rajkot between the time period of 2017–2019. Among 100 patients, 79 were males and 21 were females. The most affected age group was 16–45 years (72). The longitudinal fracture (90) is the most common type of fracture, in which non-petrous type is the most prevalent (88) as low impact injuries are more common. The most common presentations of temporal bone fracture are ear bleed (59) and decreased hearing (59), mostly over the side of trauma. The most common clinical finding is hearing impairment (59), followed by haemotympanum (20) and facial palsy (15), more common over the side of trauma. Facial palsy had been easily managed conservatively by steroids and physiotherapy in most of the cases. 12 out of 15 patients had good recovery i.e. upto grade I and II by conservative management, 3 had undergone facial nerve decompression, following which 1 had recovered completely, i.e. grade 1; 1 upto grade II while 1 did not show any improvement. Other complications included giddiness (18), trigeminal neuralgia (1) and abducens nerve palsy (1). The temporal bone is more prone to injury and complications following trauma like hearing impairment, cerebrospinal fluid leak and facial palsy resolve either spontaneously or with conservative management. Surgeries must be undertaken only if adequate conservative treatment fails and after proper investigations.


Similar content being viewed by others
References
Ulrich K (1926) Verletzungen des Gehörorgans bei Schädel-Basisfrakturen:(eine histologische und klinische Studie). Mercators
Zayas JO, Feliciano YZ, Hadley CR, Gomez AA, Vidal JA (2011) Temporal bone trauma and the role of multidetector CT in the emergency department. RadioGraphics 31(6):1741–1755
Ghorayeb BY, Yeakley JW (1992) Temporal bone fractures: longitudinal or oblique? The case for oblique temporal bone fractures. The Laryngoscope 102(2):129–134
Kelly KE, Tami TA (1994) Temporal bone and skull base trauma. In: Jackler RK, Brackmann DE (eds) Neurotology. Mosby, St Louis, pp 1127–1147
Brodie HA, Thompson TC (1997) Management of complications from 820 temporal bone fractures. Am J Otol 18(2):188–197
Little SC, Kesser BW (2006) Radiographic classification of temporal bone fractures: clinical predictability using a new system. Arch Otolaryngol Neck Surg 132(12):1300
Gleeson M, Clarke R (2008) Scott-Brown’s otorhinolaryngology, head and neck surgery, vol 3, 7th edn. CRC Press, Boca Raton, p 3070 (Chapter 241c)
Shah SB, Jackler RK (1998) Facial nerve surgery in the 19th and early 20th centuries: the evolution from crossover anastomosis to direct nerve repair. Am J Otol 19(2):236–245
Viswanatha B, Vijayashree MS, Priyadarshini V, Rasika R (2014) Clinical study of intratemporal facial nerve palsy—the causes and outcome. J Neurol Epidemiol 2:17–24
Zlab MK, Moore GF, Daly DT, Yonkers AJ (1992) Cerebrospinal fluid rhinorrhea: a review of the literature. Ear Nose Throat J 71(7):314–317
Maradi N, Somanath BM (2017) Hearing loss following temporal bone fractures—a study on classification of fractures and the prognosis. Int J Otorhinolaryngol Head Neck Surg 3(2):390
Amin Z, Sayuti R, Kahairi A, Islah W, Ahmad R (2008) Head injury with temporal bone fracture: one year review of case incidence, causes, clinical features and outcome. Med J Malays 63(5):373–376
Basavaraju U et al (2017) Temporal bone fractures and its classification: retrospective study of incidence, causes, clinical features, complications and outcome. Int J Anat Radiol Surg 6(4):RO57–RO61
Diaz R, Cervenka B, Brodie H (2016) Treatment of temporal bone fractures. J Neurol Surg Part B Skull Base 77(05):419–429
Heid L, Claussen C-F, Kersebaum M, Nagy E, Bencze G, Bencsik B (2004) Vertigo, dizziness, and tinnitus after otobasal fractures. Int Tinnitus J 10(1):94–100
Turel KE et al (2005) Post traumatic facial paralysis treatment options and strategies. IJNT 2(1):33–34
Gregory J Basura KV (2014) Bilateral temporal bone fracture resulting in expedited simultaneous bilateral cochlear implantation. J Trauma Treat 03(04). https://omicsgroup.org/journals/bilateral-temporal-bone-fracture-resulting-in-expedited-simultaneous-bilateral-cochlear-implantation-2167–1222.1000208.php?aid=33414. Cited 29 Sept 2019
Kim SY, Kim YJ, Kim YH, Park M-H (2016) Audiologic patterns of otic capsule preserving temporal bone fracture: effects of the affected subsites. Clin Exp Otorhinolaryngol 9(3):206–211
Choi MS, Shin S-O, Yeon JY, Choi YS, Kim J, Park SK (2013) Clinical characteristics of labyrinthine concussion. Korean J Audiol 17(1):13–17
Wiet RJ, Valvassori GE, Kotsanis CA, Parahy C (1985) Temporal bone fractures. State of the art review. Am J Otol 6(3):207–215
Ghorayeb BY, Rafie JJ (1989) Fracture of the temporal bone. Evaluation of 123 cases. J Radiol 70(12):703–710
Patel A, Groppo E (2010) Management of temporal bone trauma. Craniomaxillofac Trauma Reconstr 3(02):105–113
Turner JWA (1944) Facial palsy in closed head injuries the prognosis. The Lancet 243(6302):756–757
Lambert PR, Brackmann DE (1984) Facial paralysis in longitudinal temporal bone fractures: a review of 26 cases. The Laryngoscope 94(8):1022–1026
Funding
The authors have not received any funding for the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in our study involving human participant were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants for participation and publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Venugopalan, S., Mehta, M.R., Khavdu, P.J. et al. Temporal Bone Trauma Management: A Study of 100 Cases. Indian J Otolaryngol Head Neck Surg 74 (Suppl 1), 299–306 (2022). https://doi.org/10.1007/s12070-020-02068-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-020-02068-5