Abstract
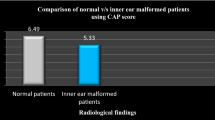
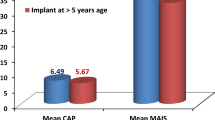
Cochlear implantation (CI) is used for rehabilitation of children with bilateral severe to profound permanent childhood hearing loss (PCHL). Recently, treatment of such children has been influenced by diagnostic technological advances. Children with perinatal risk factors associated with PCHL can undergo CI. The primary aim of this study was to determine the effects of ‘perinatal risk factor associated with PCHL’ on post-CI auditory outcomes. In this prospective study at a tertiary care centre we evaluated 50 cochlear implanted children from October 2011 to March 2013. The case group consisted of 6 (12%) children who had presence of ‘perinatal risk factor associated with PCHL’ and control group consisted of 44 (88%) children without any ‘perinatal risk factor associated with PCHL’. All patients received auditory and speech rehabilitation and we evaluated their auditory perception outcomes by categories of auditory performance (CAP) and meaningful auditory integration scale (MAIS) scores at 1 year post-CI. There were significantly decreased mean MAIS scores (decrease of 8.6%) and mean CAP scores (decrease of 6.7%) in CI recipient children with ‘perinatal risk factor associated with PCHL’ as compared to those who were without any ‘perinatal risk factor associated with PCHL’ at 1 year after CI. However, in children with ‘perinatal risk factor associated with PCHL’, mean CAP & MAIS scores (auditory perception outcomes) were still more than 80% of maximum achievable CAP & MAIS scores. In this study, CI recipient children who were without any ‘perinatal risk factor associated with PCHL’ had significantly better mean MAIS & CAP scores (auditory perception outcomes) 1 year post-CI. However, even in children who had ‘perinatal risk factor associated with PCHL’, there was substantial improvement in auditory perception outcomes at 1 year post-CI and CI was still helpful in these children. Hence, knowledge of ‘perinatal risk factor associated with PCHL’ can provide reasonable help in predicting the auditory perception outcome and optimal counselling of families of CI candidates.

Similar content being viewed by others
References
American Academy of Pediatrics (2007) Joint committee on infant hearing. Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics 120(4):898–921
Hood LJ (2015) Auditory Neuropathy/Dys-Synchrony Disorder: Diagnosis and Management. Otolaryngol Clin N Am 48(6):1027–1040
Saluja S, Agarwal A, Kler N et al (2010) Auditory neuropathy spectrum disorder in late preterm and term infants with severe jaundice. Int J Pediatr Otorhinolaryngol 74(11):1292–1297
Speleman K, Kneepkens K, Vandendriessche K et al (2012) Prevalence of risk factors for sensorineural hearing loss in NICU newborns. B-ENT 8(1):1–6
Oh W, Tyson JE, Fanaroff AA et al (2003) Association between peak serum bilirubin and neurodevelopmental outcomes in extremely low birth weight infants. Pediatrics 112:773–779
Robertson CMT, Howarth TM, Bork DLR, Dinu IA (2009) Permanent bilateral sensory and neural hearing loss of children after neonatal intensive care because of extreme prematurity: a thirty-year study. Pediatrics 123(5):e797–807
Pruszewicz A, Pospiech I (2001) Low birth weight as a risk factor of hearing loss. Scand Audiol Suppl 52:194–196
Roth DA, Hildesheimer M, Maayan-Metzger A et al (2006) Low prevalence of hearing impairment among very low birthweight infants as detected by universal neonatal hearing screening. Arch Dis Child Fetal Neonatal Ed 91(4):F257–F262
Valkama AM, Laitakari KT, Tolonen EU et al (2000) Prediction of permanent hearing loss in high risk preterm infants at term age. Eur J Pediatr 159:459–464
Mulrennan SA, Helm J, Thomas RB et al (2009) Aminoglycoside ototoxicity susceptibility in cystic fibrosis. Thorax 64:271–272
Rybak LP, Mukherjea D, Jajoo S et al (2009) Cisplatin ototoxicity and protection: clinical and experimental studies. Tohoku J Exp Med 219(3):177–186
Miyamoto RT, Osberger MJ, Todd SL, Robbins AM, Stroer BS, Zimmerman-Phillips SZ et al (1994) Variables affecting implant performance in children. Laryngoscope 104:1120–1124
Dowell RC, Cowan RSC (1997) Evaluation of benefit: infants and children. In: Clark GM (ed) CI for infants and children—advances. Singular Publishing Group, San Diego, pp 205–222
Osberger M (1998) Speech recognition performance of older children with cochlear implants. Am J Otol 19:152–157
Tye-Murray N, Spencer L, Woodworth GG (1995) Acquisition of speech by children who have prolonged cochlear implant experience. J Speech Hear Res 38:327–337
Archbold S, Lutman ME, Marshal DH (1995) Category of auditory performance. Ann Otol Rhinol Laryngol 166(Suppl. 1):312–314
Zimmerman-Phillips S, Robbins AM, Osberger MJ (2001) Infant-toddler meaningful auditory integration score. Sylmar, Calif. Advanced Bionics Corp
Fisher RA (1950) Nig J Paediatr. London: Oliver and Boyd. Statistical methods for research workers. p. 80
Esterberg R, Coffin AB, Ou H et al (2013) Fish in a dish: drug discovery for hearing habilitation. Drug Discov Today Dis Models 10(1):e23–e29
Kang DH, Lee MJ, Lee K-Y, Lee SH, Jang JH (2016) Prediction of Cochlear Implant Outcomes in Patients With Prelingual Deafness. Clin Exp Otorhinolaryngol 9(3):220–225
Birman CS, Elliott EJ, Gibson WP (2012) Pediatric cochlear implants: additional disabilities prevalence, risk factors, and effect on language outcomes. Otol Neurotol 33(8):1347–1352
Funding
None.
Author information
Authors and Affiliations
Contributions
VG: Concept and design of study, acquisition of data/analysis and interpretation of data; SS: Manuscript review and final approval of the version to be published; SS: Manuscript review.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gaurav, V., Sharma, S. & Singh, S. Effects of ‘Perinatal Risk Factors Associated with Hearing Loss’ on Auditory Outcomes in Cochlear Implant Recipient Children. Indian J Otolaryngol Head Neck Surg 74 (Suppl 1), 255–262 (2022). https://doi.org/10.1007/s12070-020-02050-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-020-02050-1