Abstract
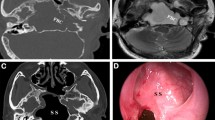
The aim of this study is to present the clinical symptoms, complications and treatments of the petrous apex cholesteatoma and is to describe the current role of oto-endoscopy. This was a retrospective non-randomized study of 14 petrous apex cholesteatoma surgeries performed between 1994 and 2012. Petrosectomy was performed according to the location of the cholesteatoma, hearing level of the patients and facial nerve function. Oto-endoscopy was used in the petrous apex and the cerebellopontine angle for residual cholesteatoma. 14 patients, seven were men and seven women were included in this study between 1994–2012. The most common symptom was hearing loss (85.7 %) and tinnitus (50 %) at the presentation. During the surgeries, it was observed that cholesteatoma involved most frequently facial nerve, dura and labyrinthines. Labyrinthectomy, middle cranial fossa approach and petromastoidectomy was performed to these patients. Four of six patients operated without the endoscope assistance between 1994–2006 had recurrences after the operation. These patients were re-operated and in the follow up, there was no recurrence. In the endoscopy assisted surgery, there was no recurrence observed (significance level p = 0.014). The most common complication after the surgery was hearing loss (42.8 %) but it was not significant after surgery (p > 0.05). The petrous apex and mastoid cavity was obliterated with fat tissue in eight patients while six patients were exteriorized to follow the recurrence and it was insignificant in recurrences (p > 0.05) Conclusion: Endoscope-assisted surgery allows to remove residual the cholesteatoma around the carotid artery, dura and facial nerve in the petrous apex resulting in less invasive surgery and less recurrence in blind spots.



Similar content being viewed by others
References
Dutt SN, Mirza S, Chavda SV, Irving RM (2002) Radiologic differentiation of intracranial epidermoids from arachnoid cysts. Otol Neurotol 23(1):84–92
Nelson M, Roger G, Koltai PJ et al (2002) Congenital cholesteatoma: classification, management, and outcome. Arch Otolaryngol Head Neck Surg 128:810–814
Semaan MT, Megerian CA (2006) The pathophysiology of cholesteatoma. Otolaryngol Clin N Am 39(6):1143–1159
Giannuzzi AL, Merkus P, Taibah A, Falcioni M (2011) Congenital mastoid cholesteatoma: case series definition, surgical key points, and literature review. Ann Otol Rhinol Laryngol 120(11):700–706
Sanna M, Zini C, Gamoletti R, Frau N, Taibah Ak, Pasanisi E (1993) Petrous bone cholesteatoma. Skull Base Surg 3(4):201–213
Fisch U (1984) Infratemporal fossa approach for lesions in the temporal bone and base of the skull. Adv Otorhinolaryngol 34:254–266
Sanna MM, Pandya Y, Mancini F, Sequino G, Piccirillo E (2011) Petrous bone cholesteatoma: classification, management and review of the literature. Audiol Neurotol 16(2):124–136
Profant M, Steno J (2000) Petrous apex cholesteatoma. Acta Otolaryngol 120(2):164–167
Schuknecht HF, Gao YZ (1984) Cochlear pathology following experimental ablation ofthe vestibular labyrinth. Ann Otol Rhinol Laryngol Suppl 112:52–58
Dhepnorrarat RC, Wood B, Rajan GP (2009) Postoperative non-echo-planar diffusion-weighted magnetic resonance imaging changes after cholesteatoma surgery: implications for cholesteatoma screening. Otol Neurotol 30(1):54–58
Yanagihara N, Nakamura K, Hatakayama T (1992) Surgical management of petrous apex cholesteatoma: a therapeutic scheme. Skull base Surg 2:22–27
Yanagihara N, Matsumoto Y (1981) Cholesteatoma in the petrous apex. Laryngoscope 91:272–278
Aubry K, Kania R, Sauvaget E, Huy PT, Herman P (2010) Endoscopic transsphenoidal approach to petrous apex cholesteatoma. Skull Base 20(4):305–308
Zanation AM, Snyderman CH, Carrau RL, Gardner PA, Prevedello DM, Kassam AB (2009) Endoscopic endonasal surgery for petrous apex lesions. Laryngoscope 119:19–25
Pyle GM, Wiet RJ (1991) Petrous apex cholesteatoma: exteriorization vs. subtotal petrosectomy with obliteration. Skull Base Surg 1(2):97–105
Coker NJ, Jenkins HA, Fisch U (1986) Obliteration of the middle ear and mastoid cleft in subtotal petrosectomy: indications, technique and results. Ann Otol Rhinol Laryngol 95:5–11
Conflict of interest
All authors had no conflict of interest on this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kumral, T.L., Uyar, Y., Yıldırım, G. et al. Does Endoscopic Surgery Reduce Recurrence of the Petrous Apex Cholesteatoma?. Indian J Otolaryngol Head Neck Surg 65, 327–332 (2013). https://doi.org/10.1007/s12070-013-0637-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-013-0637-7