Abstract
Introduction
Thymic epithelial tumors represent the most common cause of anterior mediastinal masses in adults. Among these tumors, thymomas constitute the majority, whereas thymic carcinomas are less prevalent and associated with a poorer prognosis. This study seeks to investigate the clinical and prognostic factors of these rare entities, thymoma, and thymic carcinomas.
Materials and methods
We conducted a retrospective analysis on a cohort of 60 patients diagnosed with thymoma and thymic carcinoma, who were under follow-up at our clinic between January 1998 and February 2023. The clinical characteristics and prognostic factors of these patients were analyzed separately.
Results
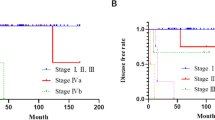
Thymomas accounted for 75% of the cases. The median age at diagnosis was 46 years in both patient groups. Masaoka stage 4 was observed in 28.9% of thymoma patients and 66.7% of thymic carcinoma patients. The median overall survival (mOS) for thymoma patients was 261.4 months, while it was 9.23 months for patients with thymic carcinoma. Curative surgery emerged as a prognostic factor significantly influencing overall survival in both thymoma and thymic carcinoma patients.
Conclusion
Our study highlights the significance of Eastern Cooperative Oncology Group (ECOG) performance status and curative surgery as prognostic factors affecting overall survival in thymoma patients. In thymic carcinoma, only curative surgery was found as a prognostic factor. These findings may enhance patient care and guide personalized treatment strategies. Further investigations and prospective studies are warranted to corroborate and expand upon these results.

Similar content being viewed by others
References
Girard N, Ruffini E, Marx A, Faivre-Finn C, Peters S. Thymic epithelial tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26:v40-55.
Engels EA. Epidemiology of thymoma and associated malignancies. J Thorac Oncol. 2010;5:S260–5.
Loehrer PJ Sr, Wang W, Johnson DH, Aisner SC, Ettinger DS. Octreotide alone or with prednisone in patients with advanced thymoma and thymic carcinoma: an Eastern Cooperative Oncology Group Phase II Trial. J Clin Oncol. 2004;22:293–9.
Marx A, Ströbel P, Badve SS, Chalabreysse L, Chan JK, Chen G, et al. ITMIG consensus statement on the use of the WHO histological classification of thymoma and thymic carcinoma: refined definitions, histological criteria, and reporting. J Thorac Oncol. 2014;9:596–611.
Eng TY, Fuller CD, Jagirdar J, Bains Y, Thomas CR Jr. Thymic carcinoma: state of the art review. Int J Radiat Oncol Biol Phys. 2004;59:654–64.
Kojima Y, Ito H, Hasegawa S, Sasaki T, Inui K. Resected invasive thymoma with multiple endocrine neoplasia type 1. Jpn J Thorac Cardiovasc Surg. 2006;54:171–3
Detterbeck FC, Stratton K, Giroux D, Asamura H, Crowley J, Falkson C, et al. The IASLC/ITMIG Thymic Epithelial Tumors Staging Project: proposal for an evidence-based stage classification system for the forthcoming (8th) edition of the TNM classification of malignant tumors. J Thorac Oncol. 2014;9:S65-72.
Schwartz LH, Litière S, de Vries E, Ford R, Gwyther S, Mandrekar S, et al. RECIST 1.1-update and clarification: from the RECIST committee. Eur J Cancer. 2016;62:132–7
Carter BW, Benveniste MF, Madan R, Godoy MC, de Groot PM, Truong MT, et al. ITMIG classification of mediastinal compartments and multidisciplinary approach to mediastinal masses. Radiographics. 2017;37:413–36.
Falkson CB, Bezjak A, Darling G, Gregg R, Malthaner R, Maziak DE, et al. The management of thymoma: a systematic review and practice guideline. J Thorac Oncol. 2009;4:911–9.
Yan M, Wu J, Xue M, Mo J, Zheng L, Zhang J, et al. The studies of prognostic factors and the genetic polymorphism of methylenetetrahydrofolate reductase C667T in thymic epithelial tumors. Front Oncol. 2022;12: 847957.
Mastromarino MG, Bacchin D, Aprile V, Ceccarelli I, Korasidis S, Lenzini A, et al. Unradical surgery for locally-advanced thymoma: is it time to evolve perspectives? Lung cancer. 2023;180: 107214.
Zhang Y, Yu L, Jing Y, Ke J. The relationship between myasthenia gravis and the different pathological type of thymoma patients’ operation and prognosis. Zhonghua wai ke za zhi. 2015;53:612–6.
Martín C, Enrico D, Mas L, Patane AK, Arrieta O, Soria T, et al. Characteristics and outcomes of thymomas in Latin America: results from over 10 years of experience (CLICaP-LATimus). Thorac cancer. 2021;12:1328–35.
Margaritora S, Cesario A, Cusumano G, Meacci E, D'Angelillo R, Bonassi S, et al. Thirty-five-year follow-up analysis of clinical and pathologic outcomes of thymoma surgery. Ann Thorac Surg. 2010;89:245–52.
Kamata S, Ishida I, Suzuki Y, Oura H. Single-center evaluation of prognostic factors for thymoma treated by surgery: a retrospective study. J Cardiothorac Surg. 2021;16:8.
Jiang YG, Ma MY, Wu JJ, Ma R, Bai XH, Zhao R, et al. Prognostic factors in patients with thymoma who underwent surgery. World J Surg Oncol. 2023;21:203.
Xu C, Zhang Y, Wang W, Wang Q, Li Z, Song Z, et al. Chinese expert consensus on the diagnosis and treatment of thymic epithelial tumors. Thorac Cancer. 2023;14:1102–17.
Berruti A, Borasio P, Gerbino A, Gorzegno G, Moschini T, Tampellini M, et al. Primary chemotherapy with adriamycin, cisplatin, vincristine and cyclophosphamide in locally advanced thymomas: a single institution experience. Br J Cancer. 1999;81:841–5.
Schmitt J, Loehrer PJ Sr. The role of chemotherapy in advanced thymoma. J Thorac Oncol. 2010;5:S357–60.
Hsu HC, Huang EY, Wang CJ, Sun LM, Chen HC. Postoperative radiotherapy in thymic carcinoma: treatment results and prognostic factors. Int J Radiat Oncol Biol Phys. 2002;52:801–5.
Ahmad U, Yao X, Detterbeck F, Huang J, Antonicelli A, Filosso PL, et al. Thymic carcinoma outcomes and prognosis: results of an international analysis. J Thorac Cardiovasc Surg. 2015;149:95–100, 1.e1–2.
Ma WL, Lin CC, Hsu FM, Lee JM, Chen JS, Huang YL, et al. Clinical outcomes for patients with thymoma and thymic carcinoma after undergoing different front-line chemotherapy regimens. Cancer Med. 2022;11:3445–56.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional ethics committee approved this study. All procedures followed were by the ethical standards of the responsible committee and the latest Declaration of Helsinki. Informed consent was not obtained from the patients due to the retrospective study design. Ankara City Hospital Clinical Research Ethics Committee approved that informed consent is not required (Date:10.05.2023 / No: E1-23–3546).
Conflict of interest
In our study, we did not receive any financial support or sponsorship. The authors declare that there is no conflict of interest among them. All the research and analysis were conducted independently without any external influence or funding. The study was solely driven by the scientific curiosity and dedication of the authors to contribute to the field of thymic epithelial tumors. The absence of any financial or personal conflicts of interest ensures the objectivity and integrity of our research findings.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bayram, D., Sekmek, S., Kayaalp, M. et al. Clinical features and prognostic factors in thymoma and thymic carcinoma. Indian J Thorac Cardiovasc Surg (2024). https://doi.org/10.1007/s12055-024-01741-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12055-024-01741-6