Abstract
Background
Aortic stenosis (AS) is a well-known cause of mortality. We aimed to assess the prognostic value of high-sensitive troponin T (hs-TnT) in symptomatic patients with severe AS and preserved left ventricular ejection fraction (LVEF) after surgical aortic valve replacement (AVR).
Patients and methods
The study recruited patients with severe symptomatic AS fulfilling the inclusion criteria in the period between April 2020 and February 2022. Comprehensive echocardiography was done. The following parameters were assessed: AS severity, LV mass index (LVMI), left atrium volume index (LAVI), and LVEF. E/e′ and LVEF were calculated using the biplane method of Simpsons. Global longitudinal strain (GLS) was assessed by speckle tracking echocardiography. Peripheral blood samples were collected for hs-TnT measurement. All patients underwent surgical AVR. The patients were followed for the following 6 months for major adverse cardiovascular events (MACE). MACE was defined as cardiac death, re-admission for congestive heart failure (CHF) and fatal arrhythmia.
Results
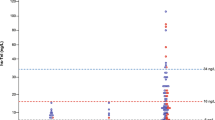
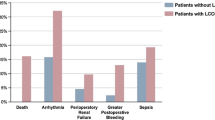
One hundred and eight patients (mean age = 58.7 ± 7.68 years) with severe AS were recruited. Seventeen patients presented with MACE including 8 cardiac deaths. We divided the patients into two groups based on the normal hs-TnT values. The Kaplan–Meier curve revealed a statistically significant difference in MACE rate among troponin groups (log-rank test = 5.06, p = 0.025). There was significant difference between both groups regarding GLS with smaller GLS in negative hs-TnT group. In multivariate analysis, GLS and hs-TnT were significantly associated with MACE (p = 0.022 and < 0.01 respectively). The cutoff value of hs-TnT of 238.25 had a sensitivity of 70% and a specificity of 81% for predicting future MACE. There was a significant correlation between GLS and troponin (p < 0.001).
Conclusions
hs-TnT is associated with bad short-term prognosis after AVR. hs-TnT and GLS could be significant predictors for future MACE in patients with severe symptomatic AS and preserved LVEF who underwent AVR. Elevated hs-TnT and impaired GLS could set an indication of early intervention in asymptomatic severe AS.


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the author (Dr. Mohammad Fikry) upon reasonable request.
Abbreviations
- AS:
-
Aortic stenosis
- hs-TnT:
-
High-sensitive troponin T
- LVEF:
-
Left ventricular ejection fraction
- LV:
-
Left ventricle
- MACE:
-
Major adverse cardiovascular event
- AVR:
-
Aortic valve replacement
- CHF:
-
Congestive heart failure
- AVA:
-
Aortic valve area
- BSA:
-
Body surface area
- LVOT:
-
Left ventricle outflow tract
- LVMI:
-
LV mass index
- LAVI:
-
Left atrial volume index
- DFS:
-
Disease-free survival
- MRI:
-
Magnetic resonance imaging
- LGE:
-
Late gadolinium enhancement
- TAVR:
-
Transcatheter aortic valve replacement
References
Carabello BA, Paulus WJ. Aortic stenosis. Lancet. 2009;373:956–66.
Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease: developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Rev Esp Cardiol (Engl Ed). 2021;75:524.
Varadarajan P, Kapoor N, Bansal RC, Pai RG. Survival in elderly patients with severe aortic stenosis is dramatically improved by aortic valve replacement: results from a cohort of 277 patients aged ≥80 years. Eur J Cardiothorac Surg. 2006;30:722–7.
Villablanca PA, Mathew V, Thourani VH, Rodes-Cabau J, Bangalore S, Makkiya M, et al. A meta-analysis and meta-regression of long-term outcomes of transcatheter versus surgical aortic valve replacement for severe aortic stenosis. Int J Cardiol. 2016;225:234–43.
Rajappan K, Rimoldi OE, Dutka DP, Ariff B, Pennell DJ, Sheridan DJ, et al. Mechanisms of coronary microcirculatory dysfunction in patients with aortic stenosis and angiographically normal coronary arteries. Circulation. 2002;105:470–6.
Park KC, Gaze DC, Collinson PO, Marber MS. Cardiac troponins: from myocardial infarction to chronic disease. Cardiovasc Res. 2017;113:1708–18.
Omland T, De Lemos JA, Sabatine MS, Christophi CA, Rice MM, Jablonski KA, et al. Prevention of Events with Angiotensin Converting Enzyme Inhibition (PEACE) trial investigators. A sensitive cardiac troponin T assay in stable coronary artery disease. N Engl J Med. 2009;361:2538–47.
DeFilippi CR, de Lemos JA, Christenson RH, Gottdiener JS, Kop WJ, Zhan M, et al. Association of serial measures of cardiac troponin T using a sensitive assay with incident heart failure and cardiovascular mortality in older adults. JAMA. 2010;304:2494–502.
Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J Am Soc Echocardiogr. 2009;22:1–23.
Taylor R. Evolution of the continuity equation in the Doppler echocardiographic assessment of the severity of valvular aortic stenosis. J Am Soc Echocardiogr. 1990;3:326–30.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015;16:233–71.
Park JH, Marwick TH. Use and limitations of E/e′ to assess left ventricular filling pressure by echocardiography. J Cardiovasc Ultrasound. 2011;19:169–73.
Dokainish H, Zoghbi WA, Lakkis NM, Al-Bakshy F, Dhir M, Quinones MA, et al. Optimal noninvasive assessment of left ventricular filling pressures: a comparison of tissue Doppler echocardiography and B-type natriuretic peptide in patients with pulmonary artery catheters. Circulation. 2004;109:2432–243914.
Witkowski TG, Thomas JD, Debonnaire PJ, Delgado V, Hoke U, Ewe SH, et al. Global longitudinal strain predicts left ventricular dysfunction after mitral valve repair. Eur Heart J Cardiovasc Imaging. 2013;14:69–76.
Fabiani I, Pugliese NR, Santini V, Conte L, Di Bello V. Speckle-tracking imaging, principles and clinical applications: a review for clinical cardiologists. In: Echocardiography in Heart Failure and Cardiac Electrophysiology. Intech 2016;85–114.
Teske AJ, De Boeck BW, Melman PG, Sieswerda GT, Doevendans PA, Cramer MJ. Echocardiographic quantification of myocardial function using tissue deformation imaging, a guide to image acquisition and analysis using tissue Doppler and speckle tracking. Cardiovasc Ultrasound. 2007;5:1–9.
Yang H, Wright L, Negishi T, Negishi K, Liu J, Marwick TH. Research to practice: assessment of left ventricular global longitudinal strain for surveillance of cancer chemotherapeutic-related cardiac dysfunction. JACC Cardiovasc Imaging. 2018;11:1196–201.
Giannitsis E, Kurz K, Hallermayer K, Jarausch J, Jaffe AS, Katus HA. Analytical validation of a high-sensitivity cardiac troponin T assay. Clin Chem. 2010;56:254–61.
Statistics IS. IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.
Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, et al. A prospective survey of patients with valvular heart disease in Europe: the Euro Heart Survey on Valvular Heart Disease. Eur Heart J. 2003;24:1231–43.
Pellikka PA, Sarano ME, Nishimura RA, Malouf JF, Bailey KR, Scott CG, et al. Outcome of 622 adults with asymptomatic, hemodynamically significant aortic stenosis during prolonged follow-up. Circulation. 2005;111:3290–5.
Gaudino M, Alessandrini F, Glieca F, Luciani N, Cellini C, Pragliola C, et al. Survival after aortic valve replacement for aortic stenosis: does left ventricular mass regression have a clinical correlate? Eur Heart J. 2005;26:51–7.
Hein S, Arnon E, Kostin S, Schönburg M, Elsässer A, Polyakova V, et al. Progression from compensated hypertrophy to failure in the pressure-overloaded human heart: structural deterioration and compensatory mechanisms. Circulation. 2003;107:984–91.
Kupari M, Eriksson S, Turto H, Lommi J, Pettersson K. Leakage of cardiac troponin I in aortic valve stenosis. J Intern Med. 2005;258:231–7.
Saito T, Hojo Y, Hirose M, Ikemoto T, Katsuki T, Kario K. High-sensitivity troponin T is a prognostic marker for patients with aortic stenosis after valve replacement surgery. J Cardiol. 2013;61:342–7.
Schwartzkopff B, Mundhenke M, Strauer BE. Remodelling of intramyocardial arterioles and extracellular matrix in patients with arterial hypertension and impaired coronary reserve. Eur Heart J. 1995;16:82–6.
Chin CW, Shah AS, McAllister DA, Joanna Cowell S, Alam S, Langrish JP, et al. High-sensitivity troponin I concentrations are a marker of an advanced hypertrophic response and adverse outcomes in patients with aortic stenosis. Eur Heart J. 2014;35:2312–21.
Hadziselimovic E, Greve AM, Sajadieh A, Olsen MH, Kesaniemi YA, Nienaber CA, et al. High-sensitive troponin T in asymptomatic aortic stenosis. Eur Heart J. 2020;41:ehaa946–16.
El Tahlawi M, Morsy M, Elawady M, Abdelaziz M, Eldamanhory A. Is there any relationship between biomarkers and echocardiographic markers in patients with pulmonary stenosis underwent balloon valvuloplasty? Echocardiography. 2021;38:924–31.
Jin H, Lyon AR, Akar FG. Arrhythmia mechanisms in the failing heart. Pacing Clin Electrophysiol. 2008;31:1048–56.
Krayenbuehl HP, Hess OM, Monrad ES, Schneider J, Mall G, Turina M. Left ventricular myocardial structure in aortic valve disease before, intermediate, and late after aortic valve replacement. Circulation. 1989;79:744–55.
Dweck MR, Joshi S, Murigu T, Alpendurada F, Jabbour A, Melina G, et al. Mid wall fibrosis is an independent predictor of mortality in patients with aortic stenosis. J Am Coll Cardiol. 2011;58:1271–9.
Dahl JS, Videbæk L, Poulsen MK, Pellikka PA, Veien K, Andersen LI, et al. Noninvasive assessment of filling pressure and left atrial pressure overload in severe aortic valve stenosis: relation to ventricular remodeling and clinical outcome after aortic valve replacement. J Thorac Cardiovasc Surg. 2011;142:e77–83.
Dahl JS, Videbæk L, Poulsen MK, Rudbæk TR, Pellikka PA, Møller JE. Global strain in severe aortic valve stenosis: relation to left ventricular remodeling and outcome after aortic valve replacement. Circ Cardiovasc Imaging. 2012;5:613–20.
Chang SA, Park PW, Sung K, Lee SC, Park SW, Lee YT, et al. Noninvasive estimate of left ventricular filling pressure correlated with early and midterm postoperative cardiovascular events after isolated aortic valve replacement in patients with severe aortic stenosis. J Thorac Cardiovasc Surg. 2010;140:1361–6.
Sakrana AA, Nasr MM, Ashamallah GA, Abuelatta RA, Naeim HA, Tahlawi ME. Paravalvular leak after transcatheter aortic valve implantation: is it anatomically predictable or procedurally determined? MDCT study Clin Radiol. 2016;71:1095–103.
Seoudy H, Lambers M, Winkler V, Dudlik L, Freitag-Wolf S, Frank J, et al. Elevated high-sensitivity troponin T levels at 1-year follow-up are associated with increased long-term mortality after TAVR. Clin Res Cardiol. 2021;110:421–8.
Takagi H, Hari Y, Nakashima K, Kuno T, Ando T. Meta-analysis of impact of troponins on mortality after transcatheter aortic valve implantation. J Cardiovasc Surg. 2020;61:98–106.
Jawitz OK, Gulack BC, Grau-Sepulveda MV, Matsouaka RA, Mack MJ, Smith PK. Contemporary outcomes of isolated aortic valve replacement in North America. J Am Coll Cardiol. 2020;76:1075–85.
Kapadia SR, Tuzcu EM, Makkar RR, Svensson LG, Agarwal S, Kodali S, et al. Long-term outcomes of inoperable patients with aortic stenosis randomized to transcatheter aortic valve replacement or standard therapy. Circulation. 2014;130:1483–92.
Funding
None.
Author information
Authors and Affiliations
Contributions
AS analyzed and interpreted the patient data. GI was responsible for conceptualization and validation. MF was responsible for formal analysis, conducting research, collection of data, and investigation process. MHE was responsible for revision, validation, and data curation. ME was responsible for conceptualization of concept and writing the draft. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics Committee approval
Ethical approval was granted from the ethical committee of the Faculty of Medicine, Zagazig University vide reference No. 6334 dated 23-08-2020.
Consent to participate
Informed consent was obtained from each participant.
Human and Animal Rights Statement
The study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. Confidentiality of participants’ personal information was maintained throughout the research process, and all data were anonymized to protect their identities. This research did not involve the use of animals. Therefore, no animals were harmed or subjected to experimentation for the purpose of this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Salama, A., Ibrahim, G., Fikry, M. et al. Prognostic value of high-sensitive troponin T in patients with severe aortic stenosis undergoing valve replacement surgery. Indian J Thorac Cardiovasc Surg 40, 142–150 (2024). https://doi.org/10.1007/s12055-023-01594-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-023-01594-5