Abstract
Purpose
Occult renal disease (ORD) is a clinical condition in which glomerular filtration rate (GFR) is less than 60 ml/min/1.73 m2, while serum creatinine is ≤ 1.3 mg/dl. The aim of the study was to compare the incidence of postoperative stage I acute kidney injury (AKI) according to Acute Kidney Injury Network (AKIN) classification in patients with ORD undergoing either off-pump or on-pump coronary artery bypass grafting.
Methods
A single center prospective randomized study was conducted from March 2011 through January 2014. A total of 120 coronary artery disease (CAD) patients with ORD undergoing coronary artery bypass grafting (CABG) were randomized to either off-pump (group1, n = 62) or on-pump (group2, n = 58) CABG in 1:1 ratio by computer-generated random number table. The GFR and serum creatinine levels were measured preoperatively and postoperatively on day 1 and day 5. The primary outcome (postoperative AKI (stage I)) and secondary outcomes (AKI (stage III) requiring renal replacement therapy (RRT) death, myocardial infarction (MI), cerebrovascular accident, atrial fibrillation (AF), and re-exploration for bleeding) at 30 days were analyzed between the groups.
Results
There is no significant difference in baseline characteristics of patients between off-pump and on-pump group. The incidence of postoperative AKI (stage I) was similar between on-pump (20.69%) and off-pump (16.13%) groups (p = 0.51). There was no significant difference in mortality (p = 0.33), postoperative MI (p = 0.34), cerebrovascular accident (p = 1.00), re-exploration (p = 0.96), and AF (p = 0.50). The number of patients of stage III AKI requiring RRT was higher in the off-pump group (3 patients, 4.8%) and none in the on-pump group (p = 0.08),
Conclusions
This study demonstrated that on-pump CABG is associated with significantly lower GFR and significantly higher serum creatinine on postoperative day 1 which return to baseline by postoperative day 5. In patients with ORD undergoing CABG, the incidence of postoperative AKI and major adverse cardiac and cerebrovascular events were similar between off-pump or on-pump CABG patients.

Similar content being viewed by others
References
Cooper WA, O’Brien SM, Thourani VH, et al. Impact of renal dysfunction on outcomes of coronary artery bypass surgery: results from the society of thoracic surgeons national adult cardiac database. Circulation. 2006;113:1063–70.
Chikwe J, Castillo JG, Rahmanian PB, Akujuo A, Adams DH, Filsoufi F. The impact of moderate-to-end-stage renal failure on outcomes after coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth. 2010;24:574–9.
Charytan DM, Yang SS, McGurk S, Rawn J. Long and short-term outcomes following coronary artery bypass grafting in patients with and without chronic kidney disease. Nephrol Dial Transplant. 2010;25:3654–63.
Zakeri R, Freemantle N, Barnett V, et al. Relation between mild renal dysfunction and outcomes after coronary artery bypass grafting. Circulation. 2005;112:I270–5.
Kellen M, Aronson S, Roizen MF, Barnard J, Thisted RA. Predictive and diagnostic tests of renal failure: a review. Anesth Analg. 1994;78:134–42.
Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function—measured and estimated glomerular filtration rate. New Engl J Med. 2006;354:2473–83.
Duncan L, Heathcote J, Djurdjev O, Levin A. Screening for renal disease using serum creatinine: who are we missing? Nephrol Dial Transplant. 2001;16:1042–6.
Rashid ST, Salman M, Agarwal S, Hamilton G. Occult renal impairment is common in patients with peripheral vascular disease and normal serum creatinine. Eur J Vasc Endovasc. 2006;32:294–9.
Sajja LR, Mannam G, Chakravarthi RM, et al. Coronary artery bypass grafting with or without cardio pulmonary bypass in patients with preoperative non-dialysis dependent renal insufficiency: a randomized study. J Thorac Cardiovasc Surg. 2007;133:378–88.
Miceli A, Bruno VD, Capoun R, Romeo F, Angelini GD, Caputo M. Occult renal dysfunction: a mortality and morbidity risk factor in coronary artery bypass grafting surgery. J Thorac Cardiovasc Surg. 2011;141:771–6.
Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31.
Chertow GM, Lazarus JM, Christiansen CL, et al. Preoperative renal risk stratification. Circulation. 1997;95:878–84.
Lassnigg A, Schmidlin D, Mouhieddine M, et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol. 2004;15:1597–605.
Provenchere S, Plantefeve G, Hufnagel G, et al. Renal dysfunction after cardiac surgery with normothermic cardiopulmonary bypass: incidence, risk factors, and effect on clinical outcome. Anesth Analg. 2003;96:1258–64.
Kim MY, Jang HR, Huh W, et al. Incidence, risk factors, and prediction of acute kidney injury after off-pump coronary artery bypass grafting. Ren Fail. 2011;33:316–22.
Marui A, Okabayashi H, Komiya T, et al. Impact of occult renal impairment on early and late outcomes following coronary artery bypass grafting. Interact Cardiovasc Thorac Surg. 2013;17:638–43.
Najafi M, Goodarznejad H, Karimi A, et al. Is preoperative serum creatinine a reliable indicator of outcome in patients undergoing coronary artery bypass surgery? J Thorac Cardiovasc Surg. 2009;137:304–8.
Sajja LR, Mannam G, Chakravarthi RM, Guttikonda J, Sompalli S, Bloomstone J. Impact of preoperative renal dysfunction on outcomes of off-pump coronary artery bypass grafting. Ann Thorac Surg. 2011;92:2161–7.
Pramodh K, Vani MK. Renal function following CABG: on-pump vs off-pump. Indian J Thorac Cardiovasc Surg. 2003;19:169–73.
Sajja LR, Mannam GC, Chakravarthi RM. In search of strategies for optimizing outcomes in patients with compromised renal function undergoing coronary artery bypass grafting. Cardiology. 2008;111:21–2.
Acknowledgments
We thank Mr.A.Nadamuni Naidu, M.Sc (Stat), Head, Department of Statistics (Retired), National Institute of Nutrition, ICMR, Hyderabad, India, and Sajja Heart Foundation, Hyderabad, India, for statistical advice; and Prashanthi Beri M.Sc (Clinical Research), Clinical Research Associate, Sajja Heart Foundation, Hyderabad, India, for the help in preparing the manuscript and analysis for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study complies with the principles of the Declaration of Helsinki and was approved by the institutional ethics committee, and informed consent was obtained from all the patients.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Discussant:
Dr Yugal K Mishra
Head of Cardiac Sciences and Chief Cardiovascular Surgeon, Manipal Hospital, Sector 6, Dwarka, New Delhi.
Question 1. What is the probable mechanism you think, by which on-pump CABG caused increase in serum creatinine and decrease in GFR on first post operative day?
Response: On-pump CABG is associated with hemodynamic disturbances at the level of arterial blood supply to the kidneys due to inflammatory, immunological, neurohumoral and mechanical factors. The hemodilution associated with cardiopulmonary bypass and non-pulsatile flow may be responsible for rise in serum creatinine.
Question 2: What is that factor which contributed to the upward trend of renal replacement therapy in post op AKI in off-pump CABG, which is not seen in on-pump group?
Response: The upward trend of renal replacement therapy in patients of off-pump CABG appears to be unrelated to the technique of off-pump or on-pump CABG. Out of 3 patients who required RRT, one patient had complete heart block with hypotension, second patient had cardiac tamponade and third patient had sepsis.
Question 3. Have you deduced any risk factors for developing AKI in patients with borderline GFR which can help in taking the precautionary measures to prevent it?
Response: Most of these patients with GFR <60 mL/min/1.73m2 had preoperative nephrology consultation where Angiotensin-converting enzyme (ACE) inhibitors and Angiotensin II receptor blockers (ARBs) were withheld , albumin was transfused in patients with hypoalbuminemia and surgery was delayed for 24 to 72 hours after coronary angiography . The duration of CPB time did not differ significantly between the patients who developed AKI and who did not. However, the mean pump time was lower and is less than 90min.
Question 4. From your table we can see the on-pump group required no renal replacement therapy in spite of higher number of AKI. What is the reason? Did they improve?
Response: In the on-pump group less severe AKI (stage 1) occurred. All of them improved postoperatively and creatinine returned to baseline at the time of discharge.
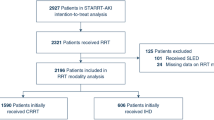
Question 5. From your consort diagram we can see there is no attrition in number of patients after allocation to the groups. That’s a very efficient conduct of a RCT. We have observed that there is high rate of attrition in randomized trials in cardiac surgery due to multiple factors. Please elaborate on the methods you used to prevent the attrition?
Response: There was no attrition in this study due to small number of patients (120) , shorter duration of study (less than 6 weeks) and enrollment of local patients who were willing to come back for the follow up.
Question 6. Considering the renal insult in occult group by coronary bypass surgery, can we generalize the concept to other organs like hepatic failure in borderline groups? Or there is renal specific mechanism involved in these patients?
Response: Ischemic hepatitis is defined as rapid and transient increase in serum transaminase levels more than 8 times of normal. There is no definition available for occult ischemic liver disease. In contrast to kidney, liver has dual blood supply from portal vein (75%) and hepatic artery (25%) and liver is less susceptible to ischemic injury. However, a mild increase in transaminase levels, less than 8 times of normal, can still be commonly found in studies in both off-pump and on-pump techniques.
Question 7. Is there any co-relation between diabetes mellitus, hypertension, LV dysfunction and prior PCI with intra-venous contrast and occurrence of AKI?
Response: The AKI is independent of diabetes mellitus, hypertension, prior PCI and LV dysfunction (mild to moderate).
Rights and permissions
About this article
Cite this article
Sajja, L.R., Singh, S., Mannam, G. et al. Impact of occult renal disease on the outcomes of off-pump and on-pump coronary artery bypass grafting. Indian J Thorac Cardiovasc Surg 35, 150–157 (2019). https://doi.org/10.1007/s12055-018-0767-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-018-0767-3