Abstract
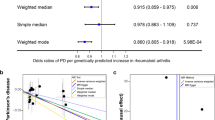
So far, the studies exploring plasma α-synuclein as a biomarker of Parkinson’s disease (PD) have provided contradictory results. Here, we first employed the Mendelian randomization (MR) approach to elucidate their potential causal relationship. Five genetic instrumental variables of plasma α-synuclein were acquired from two publicly available datasets. Three independent genome-wide association studies of PD were used as outcome cohorts (PD cohorts 1, 2, and 3). Two-sample MR analyses were conducted using inverse-variance weighted (IVW), MR-Egger, weighted median, simple mode, and leave-one-out methods. Though the IVW approach demonstrated positive plasma α-synuclein effect on the PD risk in three outcome cohorts (OR = 1.134, 1.164, and 1.189, respectively), the P values were all larger than 0.05. The conclusions were robust under complementary sensitivity analyses. Our results did not support the causal relationship between plasma α-synuclein and PD.



Similar content being viewed by others
Data Availability
The relevant GWAS summary statistics used in this work were publicly available, and the source was described appropriately in the main text.
References
de Lau LM et al (2004) Incidence of parkinsonism and Parkinson disease in a general population: the Rotterdam Study. Neurology 63(7):1240–1244
Surmeier DJ, Obeso JA, Halliday GM (2017) Selective neuronal vulnerability in Parkinson disease. Nat Rev Neurosci 18(2):101–113
Poewe W et al (2017) Parkinson disease. Nat Rev Dis Primers 3:17013
Tarsy D (2012) Treatment of Parkinson disease: a 64-year-old man with motor complications of advanced Parkinson disease. JAMA 307(21):2305–2314
GBD 2016 Parkinson’s Disease Collaborators (2018) Global, regional, and national burden of Parkinson’s disease, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 17(11):939–953
Obeso JA et al (2017) Past, present, and future of Parkinson’s disease: a special essay on the 200th Anniversary of the Shaking Palsy. Mov Disord 32(9):1264–1310
Armstrong MJ, Okun MS (2020) Diagnosis and treatment of Parkinson disease: a review. JAMA 323(6):548–560
Kowal SL et al (2013) The current and projected economic burden of Parkinson’s disease in the United States. Mov Disord 28(3):311–318
Ruppert MC et al (2021) The default mode network and cognition in Parkinson’s disease: a multimodal resting-state network approach. Hum Brain Mapp 42(8):2623–2641
Atik A, Stewart T, Zhang J (2016) Alpha-synuclein as a biomarker for Parkinson’s disease. Brain Pathol 26(3):410–418
Iwai A et al (1995) The precursor protein of non-A beta component of Alzheimer’s disease amyloid is a presynaptic protein of the central nervous system. Neuron 14(2):467–475
Spillantini MG et al (1997) Alpha-synuclein in Lewy bodies. Nature 388(6645):839–840
Fusco G, Chen SW (2017) Structural basis of membrane disruption and cellular toxicity by α-synuclein oligomers. Science 358(6369):1440–1443
Olanow CW, Brundin P (2013) Parkinson’s disease and alpha synuclein: is Parkinson’s disease a prion-like disorder? Mov Disord 28(1):31–40
Polymeropoulos MH et al (1997) Mutation in the alpha-synuclein gene identified in families with Parkinson’s disease. Science 276(5321):2045–2047
Ibáñez P et al (2004) Causal relation between alpha-synuclein gene duplication and familial Parkinson’s disease. Lancet 364(9440):1169–1171
Kalia LV (2019) Diagnostic biomarkers for Parkinson’s disease: focus on α-synuclein in cerebrospinal fluid. Parkinsonism Relat Disord 59:21–25
Parnetti L et al (2019) CSF and blood biomarkers for Parkinson’s disease. Lancet Neurol 18(6):573–586
Kang JH et al (2016) CSF biomarkers associated with disease heterogeneity in early Parkinson’s disease: the Parkinson’s Progression Markers Initiative study. Acta Neuropathol 131(6):935–949
Mollenhauer B et al (2017) Longitudinal CSF biomarkers in patients with early Parkinson disease and healthy controls. Neurology 89(19):1959–1969
Shahnawaz M et al (2017) Development of a biochemical diagnosis of Parkinson disease by detection of α-synuclein misfolded aggregates in cerebrospinal fluid. JAMA Neurol 74(2):163–172
Abd Elhadi S et al (2019) α-Synuclein in blood cells differentiates Parkinson’s disease from healthy controls. Ann Clin Transl Neurol 6(12):2426–2436
Miller DW et al (2004) Alpha-synuclein in blood and brain from familial Parkinson disease with SNCA locus triplication. Neurology 62(10):1835–1838
Lee PH et al (2006) The plasma alpha-synuclein levels in patients with Parkinson’s disease and multiple system atrophy. J Neural Transm (Vienna) 113(10):1435–1439
Duran R et al (2010) Plasma alpha-synuclein in patients with Parkinson’s disease with and without treatment. Mov Disord 25(4):489–493
Li QX et al (2007) Plasma alpha-synuclein is decreased in subjects with Parkinson’s disease. Exp Neurol 204(2):583–588
Park MJ et al (2011) Elevated levels of α-synuclein oligomer in the cerebrospinal fluid of drug-naïve patients with Parkinson’s disease. J Clin Neurol 7(4):215–222
Goldman JG et al (2018) Cerebrospinal fluid, plasma, and saliva in the BioFIND study: relationships among biomarkers and Parkinson’s disease Features. Mov Disord 33(2):282–288
Mollenhauer B et al (2011) α-Synuclein and tau concentrations in cerebrospinal fluid of patients presenting with parkinsonism: a cohort study. Lancet Neurol 10(3):230–240
Davey Smith G, Hemani G (2014) Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet 23(R1):R89-98
Yarmolinsky J et al (2018) Causal inference in cancer epidemiology: what is the role of Mendelian randomization? Cancer Epidemiol Biomarkers Prev 27(9):995–1010
Sekula P et al (2016) Mendelian randomization as an approach to assess causality using observational data. J Am Soc Nephrol 27(11):3253–3265
Ferkingstad E et al (2021) Large-scale integration of the plasma proteome with genetics and disease. Nat Genet 53(12):1712–1721
Sun BB et al (2018) Genomic atlas of the human plasma proteome. Nature 558(7708):73–79
Hemani G et al (2018) The MR-Base platform supports systematic causal inference across the human phenome. Elife 7:e34408
Fuchs J et al (2007) Phenotypic variation in a large Swedish pedigree due to SNCA duplication and triplication. Neurology 68(12):916–922
Burgess S, Butterworth A, Thompson SG (2013) Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol 37(7):658–665
Nalls MA et al (2019) Identification of novel risk loci, causal insights, and heritable risk for Parkinson’s disease: a meta-analysis of genome-wide association studies. Lancet Neurol 18(12):1091–1102
Simón-Sánchez J et al (2009) Genome-wide association study reveals genetic risk underlying Parkinson’s disease. Nat Genet 41(12):1308–1312
Elsworth B et al (2020) The MRC IEU OpenGWAS data infrastructure. bioRxiv
Burgess S et al (2020) Guidelines for performing Mendelian randomization investigations. Wellcome Open Res 4:186–186
Vázquez-Vélez GE, Zoghbi HY (2021) Parkinson’s disease genetics and pathophysiology. Annu Rev Neurosci 44:87–108
Diaz-Ortiz ME, Seo Y (2022) GPNMB confers risk for Parkinson’s disease through interaction with α-synuclein. Science 377(6608):eabk0637
Choi BK et al (2013) Large α-synuclein oligomers inhibit neuronal SNARE-mediated vesicle docking. Proc Natl Acad Sci U S A 110(10):4087–4092
Colla E et al (2012) Accumulation of toxic α-synuclein oligomer within endoplasmic reticulum occurs in α-synucleinopathy in vivo. J Neurosci 32(10):3301–3305
Zarranz JJ et al (2004) The new mutation, E46K, of alpha-synuclein causes Parkinson and Lewy body dementia. Ann Neurol 55(2):164–173
Krüger R et al (1998) Ala30Pro mutation in the gene encoding alpha-synuclein in Parkinson’s disease. Nat Genet 18(2):106–108
Appel-Cresswell S et al (2013) Alpha-synuclein p.H50Q, a novel pathogenic mutation for Parkinson’s disease. Mov Disord 28(6):811–3
Lesage S et al (2013) G51D α-synuclein mutation causes a novel parkinsonian-pyramidal syndrome. Ann Neurol 73(4):459–471
Pasanen P et al (2014) Novel α-synuclein mutation A53E associated with atypical multiple system atrophy and Parkinson’s disease-type pathology. Neurobiol Aging 35(9):2180.e1–5
Chartier-Harlin MC et al (2004) Alpha-synuclein locus duplication as a cause of familial Parkinson’s disease. Lancet 364(9440):1167–1169
Luk KC et al (2012) Pathological α-synuclein transmission initiates Parkinson-like neurodegeneration in nontransgenic mice. Science 338(6109):949–953
Stefanis L (2012) α-Synuclein in Parkinson’s disease. Cold Spring Harb Perspect Med 2(2):a009399
Olanow CW, Prusiner SB (2009) Is Parkinson’s disease a prion disorder? Proc Natl Acad Sci U S A 106(31):12571–12572
Guo JL, Lee VM (2014) Cell-to-cell transmission of pathogenic proteins in neurodegenerative diseases. Nat Med 20(2):130–138
Angot E, Brundin P (2009) Dissecting the potential molecular mechanisms underlying alpha-synuclein cell-to-cell transfer in Parkinson’s disease. Parkinsonism Relat Disord 15(Suppl 3):S143–S147
Borchelt DR et al (1994) Rapid anterograde axonal transport of the cellular prion glycoprotein in the peripheral and central nervous systems. J Biol Chem 269(20):14711–14714
El-Agnaf OM et al (2006) Detection of oligomeric forms of alpha-synuclein protein in human plasma as a potential biomarker for Parkinson’s disease. Faseb J 20(3):419–425
Hong Z et al (2010) DJ-1 and alpha-synuclein in human cerebrospinal fluid as biomarkers of Parkinson’s disease. Brain 133(Pt 3):713–726
Tokuda T et al (2010) Detection of elevated levels of α-synuclein oligomers in CSF from patients with Parkinson disease. Neurology 75(20):1766–1772
Hansson O et al (2014) Levels of cerebrospinal fluid α-synuclein oligomers are increased in Parkinson’s disease with dementia and dementia with Lewy bodies compared to Alzheimer’s disease. Alzheimers Res Ther 6(3):25
Maass F et al (2019) Cerebrospinal fluid biomarker for Parkinson’s disease: an overview. Mol Cell Neurosci 97:60–66
Wang Y et al (2012) Phosphorylated α-synuclein in Parkinson’s disease. Sci Transl Med 4(121):121ra20
Kang JH et al (2013) Association of cerebrospinal fluid β-amyloid 1–42, T-tau, P-tau181, and α-synuclein levels with clinical features of drug-naive patients with early Parkinson disease. JAMA Neurol 70(10):1277–1287
Tokuda T et al (2006) Decreased alpha-synuclein in cerebrospinal fluid of aged individuals and subjects with Parkinson’s disease. Biochem Biophys Res Commun 349(1):162–166
Lin CH et al (2017) Plasma α-synuclein predicts cognitive decline in Parkinson’s disease. J Neurol Neurosurg Psychiatry 88(10):818–824
Ibanez L et al (2017) Parkinson disease polygenic risk score is associated with Parkinson disease status and age at onset but not with alpha-synuclein cerebrospinal fluid levels. BMC Neurol 17(1):198
Ibanez L et al (2020) Functional genomic analyses uncover APOE-mediated regulation of brain and cerebrospinal fluid beta-amyloid levels in Parkinson disease. Acta Neuropathol Commun 8(1):196
Escott-Price V et al (2015) Polygenic risk of Parkinson disease is correlated with disease age at onset. Ann Neurol 77(4):582–591
Acknowledgements
We sincerely thank the researchers who performed the relevant GWAS and made the summary statistics publicly available. Their contributions were cited appropriately in the main text.
Author information
Authors and Affiliations
Contributions
Junhong Jiang: conceptualization, methodology, and writing; Qi Zhang and Zenan Lin: methodology, investigation, analysis of data, and writing; Yan He: analysis of data; Di Hu: supervision, conceptualization, and writing. The authors approved the final version of the submitted manuscript.
Corresponding authors
Ethics declarations
Ethics Approval
All relevant ethics approvals are from original genome-wide association studies.
Consent to Participate
This study only used publicly available summary statistics from published genome-wide association studies. No individual-level data were involved, and no additional informed consent is needed in this study.
Consent for Publication
No individual-level data were involved, and no consent for publication is needed for this study.
Conflict of Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Q., Lin, Z., He, Y. et al. Mendelian Randomization Analysis Reveals No Causal Relationship Between Plasma α-Synuclein and Parkinson’s Disease. Mol Neurobiol 60, 2268–2276 (2023). https://doi.org/10.1007/s12035-023-03206-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-023-03206-0