Abstract
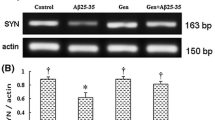
Neuronal death and synaptic loss are principal pathological features of Alzheimer’s disease (AD). Amyloid beta oligomers (AβOs) constitute the main neurotoxin underscoring AD pathology. AβOs interact with N-methyl-D-aspartate receptors (NMDARs), resulting in neurotoxic events, including activation of apoptosis and synaptic impairment. Carnosic acid (CA), extracted from Salvia rosmarinus, has been verified its neuroprotective effects in AD. However, the precise mechanisms by which CA induces synaptic protection remain unclear. In this study, we established an in vitro AD model using SH-SY5Y human neuroblastoma cells. We observed that CA improved neuronal survival by suppressing apoptosis. Moreover, CA restored synaptic impairments by increasing expression levels of brain-derived neurotrophic factor (BDNF), postsynaptic density protein-95 (PSD-95), and synaptophysin (Syn). Furthermore, we found these protective effects were dependent on inhibiting the phosphorylation of NMDAR subtype 2B (NMDAR2B), which further suppressed calcium overload and promoted activation of the extracellular signal-regulated kinase (ERK)–cAMP response element-binding protein (CREB) pathway. Administration of N-methyl-D-aspartic acid (NMDA), an agonist of NMDARs, abolished these effects of CA. Our findings demonstrate that CA exerts neuroprotective effects in an in vitro model of AD by regulating NMDAR2B and its downstream cascades, highlighting the therapeutic potential of CA as a NMDARs-targeted candidate in the treatment of AD.







Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during this study are available from the corresponding author upon reasonable request.
Abbreviations
- AD:
-
Alzheimer’s disease
- CA:
-
Carnosic acid
- Aβ:
-
Amyloid β
- AβOs:
-
Aβ oligomers
- NMDA:
-
N-Methyl-D-aspartic acid
- NMDARs:
-
N-Methyl-D-aspartate receptors
- NMDAR2B:
-
N-Methyl-D-aspartate receptor subtype 2B
- ERK:
-
Extracellular signal-regulated kinase
- CREB:
-
CAMP response element binding protein
- BDNF:
-
Brain-derived neurotrophic factor
- Bax:
-
B cell lymphoma 2 associated X
- Bcl-2:
-
B cell lymphoma 2
- MTT:
-
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide
- HBSS:
-
Hank’s Balanced Salt Solution
- SDS-PAGE:
-
Sodium dodecyl sulfate–polyacrylamide gel electrophoresis
References
GBD (2019) Dementia Forecasting Collaborators (2022) Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health 7:e105–e125. https://doi.org/10.1016/s2468-2667(21)00249-8
Cummings J, Lee G, Zhong K, Fonseca J, Taghva K (2021) Alzheimer’s disease drug development pipeline: 2021. Alzheimers Dement (N Y) 7:e12179. https://doi.org/10.1002/trc2.12179
Cummings JL, Morstorf T, Zhong K (2014) Alzheimer’s disease drug-development pipeline: few candidates, frequent failures. Alzheimers Res Ther 6:37. https://doi.org/10.1186/alzrt269
Scheltens P, De Strooper B, Kivipelto M, Holstege H, Chételat G, Teunissen CE, Cummings J, van der Flier WM (2021) Alzheimer’s disease. Lancet 397:1577–1590. https://doi.org/10.1016/s0140-6736(20)32205-4
Li K, Wei Q, Liu FF, Hu F, Xie AJ, Zhu LQ, Liu D (2018) Synaptic dysfunction in Alzheimer’s disease: Aβ, Tau, and epigenetic alterations. Mol Neurobiol 55:3021–3032. https://doi.org/10.1007/s12035-017-0533-3
Tu S, Okamoto S, Lipton SA, Xu H (2014) Oligomeric Aβ-induced synaptic dysfunction in Alzheimer’s disease. Mol Neurodegener 9:48. https://doi.org/10.1186/1750-1326-9-48
Zhang Y, Li P, Feng J, Wu M (2016) Dysfunction of NMDA receptors in Alzheimer’s disease. Neurol Sci 37:1039–1047. https://doi.org/10.1007/s10072-016-2546-5
Koh W, Park M, Chun YE, Lee J, Shim HS, Park MG, Kim S, Sa M, Joo J, Kang H, Oh SJ, Woo J, Chun H, Lee SE, Hong J, Feng J, Li Y, Ryu H, Cho J, Lee CJ (2022) Astrocytes render memory flexible by releasing D-serine and regulating NMDA receptor tone in the hippocampus. Biol Psychiatry 91:740–752. https://doi.org/10.1016/j.biopsych.2021.10.012
Griego E, Hernández-Frausto M, Márquez LA, Lara-Valderrabano L, López Rubalcava C, Galván EJ (2022) Activation of D1/D5 receptors ameliorates decreased intrinsic excitability of hippocampal neurons induced by neonatal blockade of N-methyl-d-aspartate receptors. Br J Pharmacol 179:1695–1715. https://doi.org/10.1111/bph.15735
Tu W, Xu X, Peng L, Zhong X, Zhang W, Soundarapandian MM, Balel C, Wang M, Jia N, Zhang W, Lew F, Chan SL, Chen Y, Lu Y (2010) DAPK1 interaction with NMDA receptor NR2B subunits mediates brain damage in stroke. Cell 140:222–234. https://doi.org/10.1016/j.cell.2009.12.055
Parsons MP, Raymond LA (2014) Extrasynaptic NMDA receptor involvement in central nervous system disorders. Neuron 82:279–293. https://doi.org/10.1016/j.neuron.2014.03.030
Liu Y, Wong TP, Aarts M, Rooyakkers A, Liu L, Lai TW, Wu DC, Lu J, Tymianski M, Craig AM, Wang YT (2007) NMDA receptor subunits have differential roles in mediating excitotoxic neuronal death both in vitro and in vivo. J Neurosci 27:2846–2857. https://doi.org/10.1523/jneurosci.0116-07.2007
Bao Y, Yang X, Fu Y, Li Z, Gong R, Lu W (2021) NMDAR-dependent somatic potentiation of synaptic inputs is correlated with β amyloid-mediated neuronal hyperactivity. Transl Neurodegener 10:34. https://doi.org/10.1186/s40035-021-00260-3
Ahmed H, Haider A, Ametamey SM (2020) N-Methyl-D-Aspartate (NMDA) receptor modulators: a patent review (2015-present). Expert Opin Ther Pat 30:743–767. https://doi.org/10.1080/13543776.2020.1811234
de Oliveira MR (2016) The dietary components carnosic acid and carnosol as neuroprotective agents: a mechanistic view. Mol Neurobiol 53:6155–6168. https://doi.org/10.1007/s12035-015-9519-1
Feng M, Cui D, Li Y, Shi J, Xiang L, Bian H, Ma Z, Xia W, Wei G (2020) Carnosic acid reverses the inhibition of ApoE4 on cell surface level of ApoER2 and reelin signaling pathway. J Alzheimers Dis 73:517–528. https://doi.org/10.3233/jad-190914
Rasoolijazi H, Azad N, Joghataei MT, Kerdari M, Nikbakht F, Soleimani M (2013) The protective role of carnosic acid against beta-amyloid toxicity in rats. ScientificWorldJournal 2013:917082. https://doi.org/10.1155/2013/917082
Satoh T, Trudler D, Oh CK and Lipton SA (2022) Potential therapeutic use of the rosemary diterpene carnosic acid for Alzheimer’s disease, Parkinson’s disease, and long-COVID through NRF2 activation to counteract the NLRP3 inflammasome. Antioxidants (Basel) 11. https://doi.org/10.3390/antiox11010124
Liu Y, Zhang Y, Hu M, Li YH, Cao XH (2019) Carnosic acid alleviates brain injury through NF-κB-regulated inflammation and Caspase-3-associated apoptosis in high fat-induced mouse models. Mol Med Rep 20:495–504. https://doi.org/10.3892/mmr.2019.10299
Das S, Dewanjee S, Dua TK, Joardar S, Chakraborty P, Bhowmick S, Saha A, Bhattacharjee S and De Feo V (2019) Carnosic acid attenuates cadmium induced nephrotoxicity by inhibiting oxidative stress, promoting Nrf2/HO-1 signalling and impairing TGF-β1/Smad/collagen IV signalling. Molecules 24.https://doi.org/10.3390/molecules24224176
Kuo CF, Su JD, Chiu CH, Peng CC, Chang CH, Sung TY, Huang SH, Lee WC, Chyau CC (2011) Anti-inflammatory effects of supercritical carbon dioxide extract and its isolated carnosic acid from Rosmarinus officinalis leaves. J Agric Food Chem 59:3674–3685. https://doi.org/10.1021/jf104837w
Uddin N, Ali N, Uddin Z, Nazir N, Zahoor M, Rashid U, Ullah R, Alqahtani AS, Alqahtani AM, Nasr FA, Liu M, Nisar M (2020) Evaluation of cholinesterase inhibitory potential of different genotypes of Ziziphus nummularia, their HPLC-UV, and molecular docking analysis. Molecules 25(21):5011. https://doi.org/10.3390/molecules25215011 (2020 Oct 29)
Azri FA, Selamat J, Sukor R, Yusof NA, Raston NHA, Eissa S, Zourob M, Chinnappan R (2021) Determination of minimal sequence for zearalenone aptamer by computational docking and application on an indirect competitive electrochemical aptasensor. Anal Bioanal Chem 413(15):3861–3872. https://doi.org/10.1007/s00216-021-03336-1
Bordji K, Becerril-Ortega J, Buisson A (2011) Synapses, NMDA receptor activity and neuronal Aβ production in Alzheimer’s disease. Rev Neurosci 22:285–294. https://doi.org/10.1515/rns.2011.029
Jia G, Diao Z, Liu Y, Sun C, Wang C (2021) Neural stem cell-conditioned medium ameliorates Aβ25–35-induced damage in SH-SY5Y cells by protecting mitochondrial function. Bosn J Basic Med Sci 21:179–186. https://doi.org/10.17305/bjbms.2020.4570
Cascella R and Cecchi C (2021) Calcium dyshomeostasis in Alzheimer’s disease pathogenesis. Int J Mol Sci 22. https://doi.org/10.3390/ijms22094914
Xu HN, Li LX, Wang YX, Wang HG, An D, Heng B, Liu YQ (2019) Genistein inhibits Aβ(25–35) -induced SH-SY5Y cell damage by modulating the expression of apoptosis-related proteins and Ca(2+) influx through ionotropic glutamate receptors. Phytother Res 33:431–441. https://doi.org/10.1002/ptr.6239
Padmanabhan P, Kneynsberg A, Götz J (2021) Super-resolution microscopy: a closer look at synaptic dysfunction in Alzheimer disease. Nat Rev Neurosci 22:723–740. https://doi.org/10.1038/s41583-021-00531-y
Chen MK, Mecca AP, Naganawa M, Finnema SJ, Toyonaga T, Lin SF, Najafzadeh S, Ropchan J, Lu Y, McDonald JW, Michalak HR, Nabulsi NB, Arnsten AFT, Huang Y, Carson RE, van Dyck CH (2018) Assessing synaptic density in Alzheimer disease with synaptic vesicle glycoprotein 2A positron emission tomographic imaging. JAMA Neurol 75:1215–1224. https://doi.org/10.1001/jamaneurol.2018.1836
Li S, Selkoe DJ (2020) A mechanistic hypothesis for the impairment of synaptic plasticity by soluble Aβ oligomers from Alzheimer’s brain. J Neurochem 154:583–597. https://doi.org/10.1111/jnc.15007
Haass C, Selkoe DJ (2007) Soluble protein oligomers in neurodegeneration: lessons from the Alzheimer’s amyloid beta-peptide. Nat Rev Mol Cell Biol 8:101–112. https://doi.org/10.1038/nrm2101
Sha S, Xing XN, Wang T, Li Y, Zhang RW, Shen XL, Cao YP, Qu L (2022) DNA vaccines targeting amyloid-β oligomer ameliorate cognitive deficits of aged APP/PS1/tau triple-transgenic mouse models of Alzheimer’s disease. Neural Regen Res 17:2305–2310. https://doi.org/10.4103/1673-5374.337054
Kan Z, Wang Y, Chen Q, Tang X, Thompson HJ, Huang J, Zhang J, Gao F, Shen Y, Wan X (2021) Green tea suppresses amyloid β levels and alleviates cognitive impairment by inhibiting APP cleavage and preventing neurotoxicity in 5XFAD mice. Mol Nutr Food Res 65:e2100626. https://doi.org/10.1002/mnfr.202100626
Meng C, He Z, Xing D (2013) Low-level laser therapy rescues dendrite atrophy via upregulating BDNF expression: implications for Alzheimer’s disease. J Neurosci 33:13505–13517. https://doi.org/10.1523/jneurosci.0918-13.2013
Amidfar M, de Oliveira J, Kucharska E, Budni J, Kim YK (2020) The role of CREB and BDNF in neurobiology and treatment of Alzheimer’s disease. Life Sci 257:118020. https://doi.org/10.1016/j.lfs.2020.118020
Sivanesan S, Tan A, Rajadas J (2013) Pathogenesis of Abeta oligomers in synaptic failure. Curr Alzheimer Res 10:316–323. https://doi.org/10.2174/1567205011310030011
Dore K, Carrico Z, Alfonso S, Marino M, Koymans K, Kessels HW, Malinow R (2021) PSD-95 protects synapses from β-amyloid. Cell Rep 35:109194. https://doi.org/10.1016/j.celrep.2021.109194
Vaka SRK, Murthy SN, Repka MA, Nagy T (2011) Upregulation of endogenous neurotrophin levels in the brain by intranasal administration of carnosic acid. J Pharm Sci 100:3139–3145. https://doi.org/10.1002/jps.22528
Hardingham GE, Bading H (2010) Synaptic versus extrasynaptic NMDA receptor signalling: implications for neurodegenerative disorders. Nat Rev Neurosci 11:682–696. https://doi.org/10.1038/nrn2911
Paoletti P, Bellone C, Zhou Q (2013) NMDA receptor subunit diversity: impact on receptor properties, synaptic plasticity and disease. Nat Rev Neurosci 14:383–400. https://doi.org/10.1038/nrn3504
Ortiz-Sanz C, Balantzategi U, Quintela-López T, Ruiz A, Luchena C, Zuazo-Ibarra J, Capetillo-Zarate E, Matute C, Zugaza JL, Alberdi E (2022) Amyloid β / PKC-dependent alterations in NMDA receptor composition are detected in early stages of Alzheimer´s disease. Cell Death Dis 13:253. https://doi.org/10.1038/s41419-022-04687-y
Fani G, Mannini B, Vecchi G, Cascella R, Cecchi C, Dobson CM, Vendruscolo M, Chiti F (2021) Aβ oligomers dysregulate calcium homeostasis by mechanosensitive activation of AMPA and NMDA receptors. ACS Chem Neurosci 12:766–781. https://doi.org/10.1021/acschemneuro.0c00811
Lian WW, Zhou W, Zhang BY, Jia H, Xu LJ, Liu AL, Du GH (2021) DL0410 ameliorates cognitive disorder in SAMP8 mice by promoting mitochondrial dynamics and the NMDAR-CREB-BDNF pathway. Acta Pharmacol Sin 42:1055–1068. https://doi.org/10.1038/s41401-020-00506-2
Zhu L, Yang L, Zhao X, Liu D, Guo X, Liu P, Chi T, Ji X, Zou L (2018) Xanthoceraside modulates NR2B-containing NMDA receptors at synapses and rescues learning-memory deficits in APP/PS1 transgenic mice. Psychopharmacology 235:337–349. https://doi.org/10.1007/s00213-017-4775-6
Wang XY, Zhou HR, Wang S, Liu CY, Qin GC, Fu QQ, Zhou JY, Chen LX (2018) NR2B-Tyr phosphorylation regulates synaptic plasticity in central sensitization in a chronic migraine rat model. J Headache Pain 19:102. https://doi.org/10.1186/s10194-018-0935-2
Li Y, Sun W, Han S, Li J, Ding S, Wang W, Yin Y (2017) IGF-1-involved negative feedback of NR2B NMDA subunits protects cultured hippocampal neurons against NMDA-induced excitotoxicity. Mol Neurobiol 54:684–696. https://doi.org/10.1007/s12035-015-9647-7
Qiu F, Zhou Y, Deng Y, Yi J, Gong M, Liu N, Wei C, Xiang S (2020) Knockdown of TNFAIP1 prevents di-(2-ethylhexyl) phthalate-induced neurotoxicity by activating CREB pathway. Chemosphere 241:125114. https://doi.org/10.1016/j.chemosphere.2019.125114
Liu S, Liu C, Xiong L, Xie J, Huang C, Pi R, Huang Z, Li L (2021) Icaritin alleviates glutamate-induced neuronal damage by inactivating GluN2B-containing NMDARs through the ERK/DAPK1 pathway. Front Neurosci 15:525615. https://doi.org/10.3389/fnins.2021.525615
Pang J, Hou J, Zhou Z, Ren M, Mo Y, Yang G, Qu Z, Hu Y (2020) Safflower yellow improves synaptic plasticity in APP/PS1 mice by regulating microglia activation phenotypes and BDNF/TrkB/ERK signaling pathway. Neuromolecular Med 22:341–358. https://doi.org/10.1007/s12017-020-08591-6
Zhong X, Li G, Qiu F, Huang Z (2018) Paeoniflorin ameliorates chronic stress-induced depression-like behaviors and neuronal damages in rats via activation of the ERK-CREB pathway. Front Psychiatry 9:772. https://doi.org/10.3389/fpsyt.2018.00772
Kushwah N, Jain V, Kadam M, Kumar R, Dheer A, Prasad D, Kumar B, Khan N (2021) Ginkgo biloba L. prevents hypobaric hypoxia-induced spatial memory deficit through small conductance calcium-activated potassium channel inhibition: the role of ERK/CaMKII/CREB signaling. Front Pharmacol 12:669701. https://doi.org/10.3389/fphar.2021.669701
Liu W, Jiang X, Zu Y, Yang Y, Liu Y, Sun X, Xu Z, Ding H, Zhao Q (2020) A comprehensive description of GluN2B-selective N-methyl-D-aspartate (NMDA) receptor antagonists. Eur J Med Chem 200:112447. https://doi.org/10.1016/j.ejmech.2020.112447
Loftis JM, Janowsky A (2003) The N-methyl-D-aspartate receptor subunit NR2B: localization, functional properties, regulation, and clinical implications. Pharmacol Ther 97(1):55–85. https://doi.org/10.1016/s0163-7258(02)00302-9
Geoffroy C, Paoletti P, Mony L (2022) Positive allosteric modulation of NMDA receptors: mechanisms, physiological impact and therapeutic potential. J Physiol 600:233–259. https://doi.org/10.1113/jp280875
Song Y, Zhao X, Wang D, Zheng Y, Dai C, Guo M, Qin L, Wen X, Zhou X, Liu Z (2019) Inhibition of LPS-induced brain injury by NR2B antagonists through reducing assembly of NR2B-CaMKII-PSD95 signal module. Immunopharmacol Immunotoxicol 41:86–94. https://doi.org/10.1080/08923973.2018.1549566
Vistrup-Parry M, Chen X, Johansen TL, Bach S, Buch-Larsen SC, Bartling CRO, Ma C, Clemmensen LS, Nielsen ML, Zhang M, Strømgaard K (2021) Site-specific phosphorylation of PSD-95 dynamically regulates the postsynaptic density as observed by phase separation. iScience 24(11):103268. https://doi.org/10.1016/j.isci.2021.103268
Caffino L, Piva A, Mottarlini F, Di Chio M, Giannotti G, Chiamulera C, Fumagalli F (2018) Ketamine self-administration elevates αCaMKII autophosphorylation in mood and reward-related brain regions in rats. Mol Neurobiol 55(7):5453–5461. https://doi.org/10.1007/s12035-017-0772-3
Zhang L, Yang J, Cao Y (2013) What is the new target inhibiting the progression of Alzheimer’s disease. Neural Regen Res 25 8(21):1938–47. https://doi.org/10.3969/j.issn.1673-5374.2013.21.002
Lu W, Fang W, Li J, Zhang B, Yang Q, Yan X, Peng L, Ai H, Wang JJ, Liu X, Luo J, Yang W (2015) Phosphorylation of tyrosine 1070 at the GluN2B subunit is regulated by synaptic activity and critical for surface expression of N-methyl-D-aspartate (NMDA) receptors. J Biol Chem 290(38):22945–22954. https://doi.org/10.1074/jbc.M115.663450
McQueen J, Ryan TJ, McKay S, Marwick K, Baxter P, Carpanini SM, Wishart TM, Gillingwater TH, Manson JC, Wyllie DJA, Grant SGN, McColl BW, Komiyama NH, Hardingham GE (2017) Pro-death NMDA receptor signaling is promoted by the GluN2B C-terminus independently of Dapk1. Elife 6:e17161. https://doi.org/10.7554/eLife.17161
Acknowledgements
We wish to thank Dr. Di-yang Lyv, Dr. Heng Zhang, Dr. Min Gong, Dr. Xue-chu Wang, Dr. Tan Zhao, and Dr. Yue Zhang for their generous assistant with performing experiments and suggestions on revising the manuscript. We wish to thank Bing-qiu Li, Wen-wen Li, Ya-na Pang, and Mei-na Quan for their guidance.
Funding
This study was supported by the Key Project of the National Natural Science Foundation of China (U20A20354); Beijing Brain Initiative from Beijing Municipal Science & Technology Commission (Z201100005520016, Z201100005520017); the National Major R&D projects of China-Scientific Technological Innovation 2030 (2021ZD0201802); the National Key Scientific Instrument and Equipment Development Project (31627803); and the Key Project of the National Natural Science Foundation of China (81530036).
Author information
Authors and Affiliations
Contributions
Jian-ping Jia contributed to the research concept and the study design. Wen-ying Liu designed the study, performed experiments, analyzed data, drew figures, and wrote the manuscript. Yan Li, Yan Li, and Ling-zhi Xu helped with language editing of the manuscript. Jian-ping Jia revised the manuscript critically and obtained funding. All authors contributed to the article and approved the submitted manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, Wy., Li, Y., Li, Y. et al. Carnosic Acid Attenuates AβOs-Induced Apoptosis and Synaptic Impairment via Regulating NMDAR2B and Its Downstream Cascades in SH-SY5Y Cells. Mol Neurobiol 60, 133–144 (2023). https://doi.org/10.1007/s12035-022-03032-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-022-03032-w