Abstract
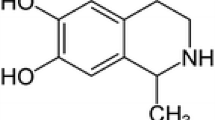
Quinolinic acid (QUIN) is an agonist of N-methyl-d-aspartate receptor (NMDAr) used to study the underlying mechanism of excitotoxicity in animal models. There is evidence indicating that impairment in autophagy at early times contributes to cellular damage in excitotoxicity; however, the status of autophagy in QUIN model on day 7 remains unexplored. In this study, the ultrastructural analysis of subcellular compartments and the status of autophagy, necroptosis, and apoptosis in the striatum of rats administered with QUIN (120 nmol and 240 nmol) was performed on day 7. QUIN induced circling behavior, neurodegeneration, and cellular damage; also, it promoted swollen mitochondrial crests, spherical-like morphology, and mitochondrial fragmentation; decreased ribosomal density in the rough endoplasmic reticulum; and altered the continuity of myelin sheaths in axons with separation of the compact lamellae. Furthermore, QUIN induced an increase and a decrease in ULK1 and p-70-S6K phosphorylation, respectively, suggesting autophagy activation; however, the increased microtubule-associated protein 1A/1B-light chain 3-II (LC3-II) and sequestosome-1/p62 (SQSTM1/p62), the coexistence of p62 and LC3 in the same structures, and the decrease in Beclin 1 and mature cathepsin D also indicates a blockage in autophagy flux. Additionally, QUIN administration increased tumor necrosis factor alpha (TNFα) and receptor-interacting protein kinase 3 (RIPK3) levels and its phosphorylation (p-RIPK3), as well as decreased B-cell lymphoma 2 (Bcl-2) and increased Bcl-2-associated X protein (Bax) levels and c-Jun N-terminal kinase (JNK) phosphorylation, suggesting an activation of necroptosis and apoptosis, respectively. These results suggest that QUIN activates the autophagy, but on day 7, it is blocked and organelle and cellular damage, neurodegeneration, and behavior alterations could be caused by necroptosis and apoptosis activation.











Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed though the current study are available as supplementary material.
References
Dong XX, Wang Y, Qin ZH (2009) Molecular mechanisms of excitotoxicity and their relevance to pathogenesis of neurodegenerative diseases. Acta Pharmacol Sin 30:379–387. https://doi.org/10.1038/aps.2009.24
Lai TW, Zhang S, Wang YT (2014) Excitotoxicity and stroke: identifying novel targets for neuroprotection. Prog Neurobiol 115:157–188. https://doi.org/10.1016/j.pneurobio.2013.11.006
Kulbe JR, Levy JMM, Coultrap SJ, Thorburn A, Bayer KU (2014) Excitotoxic glutamate insults block autophagy flux in hippocampal neurons. Brain Res 1542:12–19. https://doi.org/10.1016/j.brainres.2013.10.032
Pérez-Carrión MD, Pérez-Martínez FC, Merino S, Sánchez-Verdú P, Martínez-Hernández J, Luján R, Ceña V (2012) Dendrimer-mediated siRNA delivery knocks down Beclin 1 and potentiates NMDA-mediated toxicity in rat cortical neurons. J Neurochem 120:259–268. https://doi.org/10.1111/j.1471-4159.2011.07556.x
Yin WY, Ye Q, Huang HJ, Xia NG, Chen YY, Zhang Y, Qu QM (2016) Salidroside protects cortical neurons against glutamate-induced cytotoxicity by inhibiting autophagy. Mol Cell Biochem 419:53–64. https://doi.org/10.1007/s11010-016-2749-3
Lippai M, Lőw P (2014) The role of selective adaptor p62 and ubiquitin-like proteins in autophagy. Biomed Res Int 2014:832704. https://doi.org/10.1155/2014/832704
Zachari M, Ganley IG (2017) The mammalian ULK1 complex and autophagy initiation. Essays Biochem 61:585–596. https://doi.org/10.1042/EBC20170021
Kim J, Kundu M, Viollet B, Guan KL (2011) AMPK and mTOR regulates the autophagy through direct phosphorylation of Ulk1. Nat Cell Biol 13:132–141. https://doi.org/10.1038/ncb2152
Hurley JH, Young LN (2017) Mechanisms of autophagy initiation. Annu Rev Biochem 86:225–244. https://doi.org/10.1146/annurev-biochem-061516-044820
Braidy N, Brew BJ, Inestrosa NC, Chung R, Sachdev P, Guillemin GJ (2014) Changes in cathepsin D and Beclin-1 mRNA and protein expression by the excitotoxin quinolinic acid in human astrocytes and neurons. Metab Brain Dis 29:873–883. https://doi.org/10.1007/s11011-014-9557-9
Hernández DE, Salvadores NA, Moya-Alvarado G, Catalán RJ, Bronfman FC, Court FA (2018) Axonal degeneration induced by glutamate excitotoxicity is mediated by necroptosis. J Cell Sci 131:pii:jcs214684. https://doi.org/10.1242/jcs.214684
Li Y, Yang X, Ma C, Qiao J, Zhang C (2008) Necroptosis contributes to the NMDA-induced excitotoxicity in rat’s cultured cortical neurons. Neurosci Lett 447:120–123. https://doi.org/10.1016/j.neulet.2008.08.037
Yuan J, Amin P, Ofengeim D (2019) Necroptosis and RIPK1-mediated neuroinflammation in CNS diseases. Nat Rev Neurosci 20:19–22. https://doi.org/10.1038/s41583-018-0093-1
Frank D, Vaux DL, Murphy JM, Vince JE, Lindqvist LM (2019) Activated MLKL attenuates autophagy following its translocation to intracellular membranes. J Cell Sci 132:jcs220996. https://doi.org/10.1242/jcs.220996
Sas K, Szabó E, Vécsei L (2018) Mitochondria, oxidative stress and kynurenine system, with a focus on ageing and neuroprotection. Molecules 23:191. https://doi.org/10.3390/molecules23010191
Ferreira FS, Dos Santos TM, Ramires-Junior OV, Silveira JS, Schmitz F, Wyse ATS (2022) Quinolinic acid impairs redox homeostasis, bioenergetics, and cell signaling in rat striatum slices: prevention by coenzyme Q10. Neurotox Res 40:473–484. https://doi.org/10.1007/s12640-022-00484-9
Feng W, Wang Y, Liu ZQ, Zhang X, Han R, Miao YZ, Qin ZH (2017) Microglia activation contributes to quinolinic acid-induced neuronal excitotoxicity through TNF-α. Apoptosis 22:696–709. https://doi.org/10.1007/s10495-017-1363-5
Beal MF, Kowall NW, Swartz KJ, Ferrante RJ, Martin JB (1988) Systemic approaches to modifying quinolinic acid striatal lesions in rats. J Neurosci 8:3901–3908. https://doi.org/10.1523/JNEUROSCI.08-10-03901.1988
Ganzella M, Jardim FM, Boeck CR, Vendite D (2006) Time course of oxidative events in the hippocampus following intracerebroventricular infusion of quinolinic acid in mice. Neurosci Res 55:397–402. https://doi.org/10.1016/j.neures.2006.05.003
Wang Y, Dong XX, Cao Y, Liang ZQ, Han R, Wu JC, Gu ZL, Qin ZH (2009) p53 induction contributes to excitotoxic neuronal death in rat striatum through apoptotic and autophagic mechanisms. Eur J Neurosci 30:2258–2270. https://doi.org/10.1111/j.1460-9568.2009.07025.x
Hossain MI, Marcus JM, Lee JH, Garcia PL, Singh V, Shacka JJ, Zhang J, Gropen TI, Falany CN, Andrabi SA (2021) Restoration of CTSD (cathepsin D) and lysosomal function in stroke is neuroprotective. Autophagy 17:1330–1348. https://doi.org/10.1080/15548627.2020.1761219
Portera-Cailliau C, Price DL, Martin LJ (1997) Non-NMDA and NMDA receptor-mediated excitotoxic neuronal deaths in adult brain are morphologically distinct: further evidence for an apoptosis-necrosis continuum. J Comp Neurol 378:88–104. https://doi.org/10.1002/(SICI)1096-9861(19970203)378:1%3c88::AID-CNE5%3e3.0.CO;2-G
Feng Q, Ma Y, Mu S, Wu J, Chen S, Ouyang L, Lei W (2014) Specific reactions of different striatal neuron types in morphology induced by quinolinic acid in rats. PLoS One 9:e91512. https://doi.org/10.1371/journal.pone.0091512
Santana-Martínez RA, León-Contreras JC, Barrera-Oviedo D, Pedraza-Chaverri J, Hernández-Pando R, Maldonado PD (2018) Sustained activation of JNK induced by quinolinic acid alters the BDNF/TrkB axis in the rat striatum. Neuroscience 383:22–32. https://doi.org/10.1016/j.neuroscience.2018.04.034
Paxinos G, Watson C (1998) The rat brain in stereotaxic coordinates, 3rd edn. Academic Press Inc., San Diego
Lowry OH, Rosebrough NJ, Farr AL, Randall LJ (1951) Protein measurement with the Folin-phenol reagent. J Biol Chem 193:265–275. https://doi.org/10.1016/S0021-9258(19)52451-6
Nguyen HQ, Zada S, Lai TH, Pham TM, Hwang JS, Ahmed M, Kim DR (2019) Calpain-induced Beclin1 cleavage stimulates senescence-associated cell death in HT22 hippocampal cells under the oxidative stress conditions. Neurosci Lett 701:106–111. https://doi.org/10.1016/.neulet.2019.02.036
Mehta A, Prabhakar M, Kumar P, Deshmukh R, Sharma PL (2013) Excitotoxicity: bridge to various triggers in neurodegenerative disorders. Eur J Pharmacol 698:6–18. https://doi.org/10.1016/j.ejphar.2012.10.032
Schwarcz R, Guidetti P, Sathyasaikumar KV, Muchowski PJ (2010) Of mice, rats and men: revisiting the quinolinic acid hypothesis of Huntington’s disease. Prog Neurobiol 90:230–245. https://doi.org/10.1016/j.pneurobio.2009.04.005
da Silveira TL, Zamberland DC, Arantes LP, Machado ML, da Silva TC, Câmara DF, Santamaría A, Aschner M, Soares FAA (2018) Quinolinic acid and glutamatergic neurodegeneration in Caenorhabditis elegans. Neurotoxicology 67:94–101. https://doi.org/10.1016/j.neuro.2018.04.015
Ferreira FS, Schmitz F, Marques EP, Siebert C, Wyse ATS (2020) Intrastriatal quinolinic acid administration impairs redox homeostasis and induces inflammatory changes: prevention by kynurenic acid. Neurotox Res 38:50–58. https://doi.org/10.1007/s12640-020-00192-2
Santamaría A, Jiménez-Capdeville ME, Camacho A, Rodríguez-Martínez E, Flores A, Galván-Arzate S (2001) In vivo hydroxyl radical formation after quinolinic acid infusion into rat corpus striatum. NeuroReport 12:2693–2696. https://doi.org/10.1097/00001756-200108280-00020
Maldonado PD, Molina-Jijón E, Villeda-Hernández J, Galván-Arzate S, Santamaría A, Pedraza-Chaverrí J (2010) NAD(P)H oxidase contributes to neurotoxicity in an excitotoxic/prooxidant model of Huntington’s disease in rats: protective role of apocynin. J Neurosci Res 88:620–629. https://doi.org/10.1002/jnr.22240
Santamaría A, Rios C (1993) MK-801, an N-methyl-D-aspartate receptor antagonist, blocks quinolinic acid-induced lipid peroxidation in rat corpus striatum. Neurosci Lett 159:51–54. https://doi.org/10.1016/0304-3940(93)90796-n
Colín-González AL, Orozco-Ibarra M, Chánez-Cárdenas ME, Rangel-López E, Santamaría A, Pedraza-Chaverri J, Barrera-Oviedo D, Maldonado PD (2013) Heme oxigenase-1 (HO-1) upregulation delays morphological and oxidative stress damage induced in an excitotoxic/pro-oxidant model in the rat striatum. Neuroscience 231:91–101. https://doi.org/10.1016/j.neuroscience.2012.11.031
Cruz-Aguado R, Francis-Turner L, Díaz CM, Antúnez I (2000) Quinolinic acid lesion induces changes in rat striatal glutathione metabolism. Neurochem Int 37:53–60. https://doi.org/10.1016/s0197-0186(99)00165-5
Ferreiro E, Baldeiras I, Ferreira IL, Costa RO, Rego AC, Pereira CF, Oliveira CR (2012) Mitochondrial-and endoplasmic reticulum-associated oxidative stress in Alzheimer’s disease: from pathogenesis to biomarkers. Int J Cell Biol 2012:735206. https://doi.org/10.1155/2012/735206
Zündorf G, Reiser G (2011) Calcium dysregulation and homeostasis of neural calcium in the molecular mechanisms of neurodegenerative diseases provide multiple targets for neuroprotection. Antioxid Redox Signal 17:1275–1288. https://doi.org/10.1089/ars.2010.3359
Mishra J, Kumar A (2014) Improvement of mitochondrial function by paliperidone attenuates quinolinic acid-induced behavioural and neurochemical alterations in rats: implications in Huntington’s disease. Neurotox Res 26:363–381. https://doi.org/10.1007/s12640-014-9469-9
Luis-García ER, Limón-Pacheco JH, Serrano-García N, Hernández-Pérez AD, Pedraza-Chaverri J, Orozco-Ibarra M (2017) Sulforaphane prevents quinolinic acid-induced mitochondrial dysfunction in rat striatum. J Biochem Mol Toxicol 31:e21837. https://doi.org/10.1002/jbt.21837
Fernandes AM, Landeira-Fernandez AM, Souza-Santos P, Carvalho-Alves PC, Castilho RF (2008) Quinolinate-induced rat striatal excitotoxicity impairs endoplasmic reticulum Ca2+-ATPase function. Neurochem Res 33:1749–1758. https://doi.org/10.1007/s11064-008-9619-7
Beskid M, Zamecka E, Dybkowska-Klos H, Jachimowicz J, Kocjasz W (1995) Effect of quinolinic acid administration on rat liver: ultrastructural investigation. Exp Toxicol Pathol 47:375–379. https://doi.org/10.1016/s0940-2993(11)80352-0
Lim CK, Smythe GA, Stocker R, Brew BJ, Guillemin GJ (2007) Characterization of the kynurenine pathway in human oligodendrocytes. Int Congr Ser 1304:213–217. https://doi.org/10.1016/j.ics.2007.07.011
Cammer W (2001) Oligodendrocyte killing by quinolinic acid in vitro. Brain Res 896:157–160. https://doi.org/10.1016/s0006-8994(01)02017-0
Micu I, Jiang Q, Coderre E, Ridsdale A, Zhang L, Woulfe J, Yin X, Trapp BD, McRory JE, Rehak R, Zamponi GW, Wang W, Stys PK (2006) NMDA receptors mediate calcium accumulation in myelin during chemical ischaemia. Nature 439:988–992. https://doi.org/10.1038/nature04474
Chung Y, Lee J, Jung S, Lee Y, Cho JW, Oh YJ (2018) Dysregulated autophagy contributes to caspase-dependent neuronal apoptosis. Cell Detah Dis 9:1189. https://doi.org/10.1038/s41419-018-1229-y
Montiel T, Montes-Ortega LA, Flores-Yáñez S, Massieu L (2020) Treatment with the keto body D-beta-hydroxybutyrate attenuates autophagy activation by NMDA and reduces excitotoxic neuronal damage in the rat striatum in vivo. Curr Pharm Des 26:1377–1387. https://doi.org/10.2174/1381612826666200115103646
Peker N, Gozuacik D (2020) Autophagy as a cellular stress response mechanisms in the nervous system. J Mol Biol 432:2560–2588. https://doi.org/10.1016/j.jmb.2020.01.017
Bieri G, Lucin KM, O’Brien CE, Zhang H, Villeda SA, Wyss-Cora T (2018) Proteolytic cleavage of Beclin 1 exacerbates neurodegeneration. Mol Neurodegener 13:68. https://doi.org/10.1186/s13024-018-0302-4
Chen JH, Kuo HC, Lee KF, Tsai TH (2015) Global proteomic analysis of brain tissue in transient ischemia brain damage in rats. Int J Mol Sci 16:11873–11891. https://doi.org/10.3390/ijms160611873
Koike M, Nakanishi H, Saftig P, Ezaki J, Isahara K, Ohsawa Y, Schulz-Schaeffer W, Watanabe T, Waguri S, Kametaka S, Shibata M, Yamamoto K, Kominami E, Peters C, von Figura K, Uchiyama Y (2000) Cathepsin D deficiency induces lysosomal storage with ceroid lipofuscin in mouse CNS neurons. J Neurosci 20:6898–6906. https://doi.org/10.1523/JNEUROSCI.20-18-06898.2000
Koike M, Shibata M, Ohsawa Y, Nakanishi H, Koga T, Kametaka S, Waguri S, Momoi T, Kominami E, Peters C, von Figura K, Saftig P, Uchiyama Y (2003) Involvement of two different cell death pathways in retinal atrophy of cathepsin D-deficient mice. Mol Cell Neurosci 22:146–161. https://doi.org/10.1016/s1044-7431(03)00035-6
Deng X, Xiao L, Lang W, Gao F, Ruvolo P, May WS Jr (2001) Novel role for JNK as a stress-activated Bcl2 kinase. J Biol Chem 276:23681–23688. https://doi.org/10.1074/jbc.M1002792000
Lin SS, Bassik MC, Suh H, Nishino M, Arroyo JD, Hahn WC, Korsmeyer SJ, Roberts TM (2006) PP2A regulates Bcl-2 phosphorylation and proteasome-mediated degradation at the endoplasmic reticulum. J Biol Chem 281:23003–23012. https://doi.org/10.1074/jbc.M602648200
Zhang YX, Kong CZ, Wang LH, Li JY, Liu XK, Xu B, Xu CL, Sun YH (2010) Ursolic acid overcomes Bcl-2 mediated resistance to apoptosis in prostate cancer cell involving activation of JNK-induced Bcl-2 phosphorylation and degradation. J Cell Biochem 109:764–773. https://doi.org/10.1002/jcb.22455
Naito MG, Xu D, Amin P, Lee J, Wang H, Li W, Kelliher M, Pasparakis M, Yuan J (2020) Sequential activation of necroptosis and apoptosis cooperates to mediate vascular and neural pathology in stroke. Proc Natl Acad Sci U S A 117:4959–4970. https://doi.org/10.1073/pnas.1916427117
Deng XX, Li SS, Sun FY (2019) Necrostatin-1 prevents necroptosis in brain after ischemic stroke via inhibition of RIPK1-mediated RIPK3/MLKL signaling. Aging Dis 10:807–817. https://doi.org/10.14336/AD.2018.0728
Yuan S, Yu Z, Zhang Z, Zhang J, Zhang P, Li X, Li H, Shen H, Chen G (2019) RIP3 participates in early brain injury after experimental subarachnoid hemorrhage in rats by inducing necroptosis. Neurobiol Dis 129:144–158. https://doi.org/10.1016/j.nbd.2019.05.004
Chen T, Pan H, Li J, Xu H, Jin H, Qian C, Yan F, Chen J, Wang C, Chen J, Wang L, Chen G (2018) Inhibition of RIPK3 attenuates early brain injury following subarachnoid hemorrhage: possibly through alleviation necroptosis. Biomed Pharmacother 107:563–570. https://doi.org/10.1016/j.biopha.2018.08.056
Funding
This work was supported by CONACYT (Grant No. A1-S-21433 to PDM).
Author information
Authors and Affiliations
Contributions
Conceptualization: Perla D. Maldonado and Carlos Alfredo Silva-Islas; methods: Carlos Alfredo Silva-Islas, Ricardo Alberto Santana-Martínez, and Juan Carlos León-Contreras; formal analysis and investigation: Carlos Alfredo Silva-Islas; writing or preparation of the original draft: Carlos Alfredo Silva-Islas and Ricardo Alberto Santana-Martínez; writing which included review and editing: Carlos Alfredo Silva-Islas, Diana Barrera-Oviedo, Jose Pedraza-Chaverri, Rogelio Hernández-Pando, and Perla D. Maldonado; funding acquisition: Perla D. Maldonado; resources: Perla D Maldonado; supervision: Jose Pedraza-Chaverri, Rogelio Hernández-Pando, and Perla D. Maldonado. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
This research only involves animals. All procedures with animals were carried out strictly according to the National Institutes of Health Guide for the Care and Use of Laboratory Animals and to the Norma Oficial Mexicana NOM-062-ZOO-1999. The experimental procedures were approved by the Institutional and Local Committee for the Care and Use of Laboratory Animals on the Ethical Use of Animals from Instituto Nacional de Neurología y Neurocirugía Manuel Velasco Suárez, INNN project 44/15. During the experiments, all efforts were made to minimize animal suffering. Informed consent is not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Silva-Islas, C.A., Santana-Martínez, R.A., León-Contreras, J.C. et al. Quinolinic Acid Induces Alterations in Neuronal Subcellular Compartments, Blocks Autophagy Flux and Activates Necroptosis and Apoptosis in Rat Striatum. Mol Neurobiol 59, 6632–6651 (2022). https://doi.org/10.1007/s12035-022-02986-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-022-02986-1