Abstract
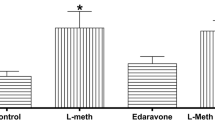
Elevated levels of homocysteine (Hcy) in the blood, called hyperhomocysteinemia (HHcy), is a prevalent risk factor for it has been shown that Hcy induces oxidative stress and increases microglial activation and neuroinflammation, as well as causes cognitive impairment, which have been linked to the neurodegenerative process. This study aimed to evaluate the effect of mild hyperhomocysteinemia with or without ibuprofen and rivastigmine treatments on the behavior and neurochemical parameters in male rats. The chronic mild HHcy model was chemically induced in Wistar rats by subcutaneous administration of Hcy (4055 mg/kg body weight) twice daily for 30 days. Ibuprofen (40 mg/kg) and rivastigmine (0.5 mg/kg) were administered intraperitoneally once daily. Motor damage (open field, balance beam, rotarod, and vertical pole test), cognitive deficits (Y-maze), neurochemical parameters (oxidative status/antioxidant enzymatic defenses, presynaptic protein synapsin 1, inflammatory profile parameters, calcium binding adapter molecule 1 (Iba1), iNOS gene expression), and cholinergic anti-inflammatory pathway were investigated. Results showed that mild HHcy caused cognitive deficits in working memory, and impaired motor coordination reduced the amount of synapsin 1 protein, altered the neuroinflammatory picture, and caused changes in the activity of catalase and acetylcholinesterase enzymes. Both rivastigmine and ibuprofen treatments were able to mitigate this damage caused by mild HHcy. Together, these neurochemical changes may be associated with the mechanisms by which Hcy has been linked to a risk factor for AD. Treatments with rivastigmine and ibuprofen can effectively reduce the damage caused by increased Hcy levels.











Similar content being viewed by others
Data Availability
Raw data are available from the authors upon request.
Abbreviations
- Hcy:
-
Homocysteine
- HHcy:
-
Hyperhomocysteinemia
- AD:
-
Alzheimer's disease
- ROS:
-
Reactive oxygen species
- DCFH:
-
Dihydrochlorofluorscein
- TBARS:
-
Reactive substances of thiobarbituric acid
- CAT:
-
Catalase
- SOD:
-
Superoxide dismutase
- Iba1:
-
Ionized calcium-binding adapter molecule 1
- iNOS:
-
Inducible nitric oxide synthase
- TNF-α:
-
Tumor necrosis factor-alpha
- IL-1β:
-
Interleukin 1 beta
- IL-6:
-
Interleukin 6
- IL-10:
-
Interleukin 10
- ACh:
-
Acetylcholine
- AChE:
-
Acetylcholinesterase
- ChAT:
-
Acetyltransferase
References
Škovierová H, Vidomanová E, Mahmood S et al (2016) The molecular and cellular effect of homocysteine metabolism imbalance on human health. Int J Mol Sci 17:1–18. https://doi.org/10.3390/ijms17101733
Shen W, Gao C, Cueto R et al (2020) Homocysteine-methionine cycle is a metabolic sensor system controlling methylation-regulated pathological signaling. Redox Biol 28:101322. https://doi.org/10.1016/j.redox.2019.101322
Bonetti F, Brombo G, Zuliani G (2016) The relationship between hyperhomocysteinemia and neurodegeneration. Neurodegener Dis Manag 6:133–145. https://doi.org/10.2217/nmt-2015-0008
Braun DJ, Dimayuga E, Morganti JM, Van Eldik LJ (2020) Microglial-associated responses to comorbid amyloid pathology and hyperhomocysteinemia in an aged knock-in mouse model of Alzheimer’s disease. J Neuroinflamm 17:1–17. https://doi.org/10.1186/s12974-020-01938-7
Smith AD, Refsum H (2016) Homocysteine, B vitamins, and cognitive impairment. Annu Rev Nutr 36:211–239. https://doi.org/10.1146/annurev-nutr-071715-050947
Kuo HK, Sorond FA, Chen JH et al (2005) The role of homocysteine in multisystem age-related problems: a systematic review. J Gerontol Ser A Biol Sci Med Sci 60:1190–1201. https://doi.org/10.1093/gerona/60.9.1190
Price BR, Wilcock DM, Weekman EM (2018) Hyperhomocysteinemia as a risk factor for vascular contributions to cognitive impairment and dementia. Front Aging Neurosci 10. https://doi.org/10.3389/fnagi.2018.00350
Hooshmand B, Refsum H, Smith AD et al (2019) Association of methionine to homocysteine status with brain magnetic resonance imaging measures and risk of dementia. JAMA Psychiatry 76:1198–1205. https://doi.org/10.1001/jamapsychiatry.2019.1694
Morris MS (2003) Homocysteine and Alzheimer’s disease. Lancet Neurol 2:425–428. https://doi.org/10.1016/S1474-4422(03)00438-1
Beal MF, Swartz KJ, Finn SF et al (1991) Neurochemical characterization of excitotoxin lesions in the cerebral cortex. J Neurosci 11:147–158. https://doi.org/10.1523/jneurosci.11-01-00147.1991
Lipton SA, Kim WK, Choi YB et al (1997) Neurotoxicity associated with dual actions of homocysteine at the N-methyl-D-aspartate receptor. Proc Natl Acad Sci U S A 94:5923–5928. https://doi.org/10.1073/pnas.94.11.5923
Ma F, Wu T, Zhao J et al (2017) Plasma homocysteine and serum folate and vitamin B12 levels in mild cognitive impairment and alzheimer’s disease: a case-control study. Nutrients 9:1–11. https://doi.org/10.3390/nu9070725
Li JG, Chu J, Barrero C et al (2014) Homocysteine exacerbates β-amyloid pathology, tau pathology, and cognitive deficit in a mouse model of Alzheimer disease with plaques and tangles. Ann Neurol 75:851–863. https://doi.org/10.1002/ana.24145
Andra A, Tanigawa S, Bito T et al (2021) Effects of vitamin b12 deficiency on amyloid-β toxicity in caenorhabditis elegans. Antioxidants 10:1–11. https://doi.org/10.3390/antiox10060962
Wyse ATS, Sanches EF, Dos Santos TM et al (2020) Chronic mild hyperhomocysteinemia induces anxiety-like symptoms, aversive memory deficits and hippocampus atrophy in adult rats: New insights into physiopathological mechanisms. Brain Res 1728:146592. https://doi.org/10.1016/j.brainres.2019.146592
Chai GS, Jiang X, Ni ZF et al (2013) Betaine attenuates Alzheimer-like pathological changes and memory deficits induced by homocysteine. J Neurochem 124:388–396. https://doi.org/10.1111/jnc.12094
Raven F, Van der Zee EA, Meerlo P, Havekes R (2018) The role of sleep in regulating structural plasticity and synaptic strength: implications for memory and cognitive function. Sleep Med Rev 39:3–11. https://doi.org/10.1016/j.smrv.2017.05.002
Richter-Levin G, Segal M (1991) The effects of serotonin depletion and raphe grafts on hippocampal electrophysiology and behavior. J Neurosci 11:1585–1596. https://doi.org/10.1523/jneurosci.11-06-01585.1991
Fakhoury M (2017) Microglia and astrocytes in Alzheimer’s disease: implications for therapy. Curr Neuropharmacol 15:508–518. https://doi.org/10.2174/1570159x15666170720095240
Zhang Q, Lu Y, Bian H et al (2017) Activation of the α7 nicotinic receptor promotes lipopolysaccharide-induced conversion of M1 microglia to M2. Am J Transl Res 9:971–985
Scherer EBS, Loureiro SO, Vuaden FC et al (2014) Mild hyperhomocysteinemia increases brain acetylcholinesterase and proinflammatory cytokine levels in different tissues. Mol Neurobiol 50:589–596. https://doi.org/10.1007/s12035-014-8660-6
Shifrin H, Nadler-Milbauer M, Shoham S, Weinstock M (2013) Rivastigmine alleviates experimentally induced colitis in mice and rats by acting at central and peripheral sites to modulate immune responses. PLoS One 8. https://doi.org/10.1371/journal.pone.0057668
Nizri E, Irony-Tur-Sinai M, Faranesh N et al (2008) Suppression of neuroinflammation and immunomodulation by the acetylcholinesterase inhibitor rivastigmine. J Neuroimmunol 203:12–22. https://doi.org/10.1016/j.jneuroim.2008.06.018
Krukiewicz K, Kowalik A, Turczyn R, Biggs MJP (2020) In vitro attenuation of astrocyte activation and neuroinflammation through ibuprofen-doping of poly(3,4-ethylenedioxypyrrole) formulations. Bioelectrochemistry 134:107528. https://doi.org/10.1016/j.bioelechem.2020.107528
Liu L, Chen S, Xu X et al (2017) Astragalus polysaccharides combined with ibuprofen exhibit a therapeutic effect on septic rats via an anti-inflammatory cholinergic pathway. Exp Ther Med 14:3127–3130. https://doi.org/10.3892/etm.2017.4865
Scherer EBS, da Cunha AA, Kolling J et al (2011) Development of an animal model for chronic mild hyperhomocysteinemia and its response to oxidative damage. Int J Dev Neurosci 29:693–699. https://doi.org/10.1016/j.ijdevneu.2011.06.004
Todorovic D, Stojanovic M, Medic A et al (2021) Four weeks of aerobic training affects cardiac tissue matrix metalloproteinase, lactate dehydrogenase and malate dehydrogenase enzymes activities, and hepatorenal biomarkers in experimental hyperhomocysteinemia in rats. Int J Mol Sci 22. https://doi.org/10.3390/ijms22136792
Matté C, Mussulini BHM, dos Santos TM et al (2010) Hyperhomocysteinemia reduces glutamate uptake in parietal cortex of rats. Int J Dev Neurosci 28:183–187. https://doi.org/10.1016/j.ijdevneu.2009.11.004
Streck EL, Matte C, Vieira PS et al (2002) Reduction of Na+, K+-ATPase activity in hippocampus of rats subjected to chemically induced hyperhomocysteinemia. Neurochem Res 27:1593–1598. https://doi.org/10.1023/A:1021670607647
Naeem S, Ikram R, Khan SS, Rao SS (2017) NSAIDs ameliorate cognitive and motor impairment in a model of parkinsonism induced by chlorpromazine. Pak J Pharm Sci 30:801–808
Comim CM, Pereira JG, Steckert A et al (2009) Rivastigmine reverses habituation memory impairment observed in sepsis survivor rats. Shock 32:270–271. https://doi.org/10.1097/SHK.0b013e31819963c4
Netto CA, Hodges H, Sinden JD et al (1993) Effects of fetal hippocampal field grafts on ischaemic-induced deficits in spatial navigation in the water maze. Neuroscience 54:69–92. https://doi.org/10.1016/0306-4522(93)90384-R
Rojas JJ, Deniz BF, Miguel PM et al (2013) Effects of daily environmental enrichment on behavior and dendritic spine density in hippocampus following neonatal hypoxia-ischemia in the rat. Exp Neurol 241:25–33. https://doi.org/10.1016/j.expneurol.2012.11.026
He YC, Wu GY, Li D et al (2012) Histamine promotes rat motor performances by activation of H 2 receptors in the cerebellar fastigial nucleus. Behav Brain Res 228:44–52. https://doi.org/10.1016/j.bbr.2011.11.029
Metz GAS, Dietz V, Schwab ME, Van De Meent H (1998) The effects of unilateral pyramidal tract section on hindlimb motor performance in the rat. - Behavioural brain research - 1998 - Metz et al.pdf. Behav Brain Res 96:37–46
Park G, Park YJ, Yang HO, Oh MS (2013) Ropinirole protects against 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine (MPTP)-induced neurotoxicity in mice via anti-apoptotic mechanism. Pharmacol Biochem Behav 104:163–168. https://doi.org/10.1016/j.pbb.2013.01.017
Song SH, Jee YS, Ko IG et al (2018) Treadmill exercise and wheel exercise improve motor function by suppressing apoptotic neuronal cell death in brain inflammation rats. J Exerc Rehabil 14:911–919. https://doi.org/10.12965/jer.1836508.254
Momeni S, Segerström L, Roman E (2015) Supplier-dependent differences in intermittent voluntary alcohol intake and response to naltrexone in Wistar rats. Front Neurosci 9:1–13. https://doi.org/10.3389/fnins.2015.00424
Szczygieł JA, Danielsen KI, Melin E et al (2020) Gene therapy vector encoding neuropeptide Y and its receptor Y2 for future treatment of epilepsy: preclinical data in rats. Front Mol Neurosci 13:1–13. https://doi.org/10.3389/fnmol.2020.603409
LeBel CP, Ischiropoulos H, Bondy SC (1992) Evaluation of the probe 2′,7′-dichlorofluorescin as an indicator of reactive oxygen species formation and oxidative stress. Chem Res Toxicol 5:227–231. https://doi.org/10.1021/tx00026a012
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358. https://doi.org/10.1016/0003-2697(79)90738-3
Aksenov MY, Markesbery WR (2001) Changes in thiol content and expression of glutathione redox system genes in the hippocampus and cerebellum in Alzheimer’s disease. Neurosci Lett 302:141–145. https://doi.org/10.1016/S0304-3940(01)01636-6
Marklund SL (1985) Product of extracellular-superoxide dismutase catalysis. FEBS Lett 184:237–239. https://doi.org/10.1016/0014-5793(85)80613-X
Aebi H (1984) [13] Catalase in vitro. Methods Enzymol 105:121–126. https://doi.org/10.1016/S0076-6879(84)05016-3
Ferreira FS, Biasibetti-Brendler H, Pierozan P et al (2018) Kynurenic acid restores Nrf2 levels and prevents quinolinic acid-induced toxicity in rat striatal slices. Mol Neurobiol 55:8538–8549. https://doi.org/10.1007/s12035-018-1003-2
Heneka MT, Carson MJ, El KJ et al (2015) Neuroinflammation in Alzheimer’s disease. Lancet Neurol 14:388–405. https://doi.org/10.1016/S1474-4422(15)70016-5
Nyul-Toth A, DelFavero J, Mukli P et al (2021) Early manifestation of gait alterations in the Tg2576 mouse model of Alzheimer’s disease. GeroScience. https://doi.org/10.1007/s11357-021-00401-6
Blaise SA, Nédélec E, Schroeder H et al (2007) Gestational vitamin B deficiency leads to homocysteine-associated brain apoptosis and alters neurobehavioral development in rats. Am J Pathol 170:667–679. https://doi.org/10.2353/ajpath.2007.060339
Obeid R, Herrmann W (2006) Mechanisms of homocysteine neurotoxicity in neurodegenerative diseases with special reference to dementia. FEBS Lett 580:2994–3005. https://doi.org/10.1016/j.febslet.2006.04.088
Kumar M, Sandhir R (2019) Hydrogen sulfide suppresses homocysteine-induced glial activation and inflammatory response. Nitric Oxide Biol Chem 90:15–28. https://doi.org/10.1016/j.niox.2019.05.008
Rocha-Dias PF, Simao-Silva DP, da Silva SSL et al (2020) Influence of a genetic variant of CHAT gene over the profile of plasma soluble ChAT in Alzheimer disease. Genet Mol Biol 43:1–6. https://doi.org/10.1590/1678-4685-GMB-2019-0404
Bello-Medina PC, Hernández-Quiroz F, Pérez-Morales M et al (2021) Spatial memory and gut microbiota alterations are already present in early adulthood in a pre-clinical transgenic model of Alzheimer’s disease. Front Neurosci 15:1–18. https://doi.org/10.3389/fnins.2021.595583
Tosto G, Monsell SE, Hawes SE, Mayeux R (2015) Pattern of extrapyramidal signs in Alzheimer’s disease. J Neurol 262:2548–2556. https://doi.org/10.1007/s00415-015-7886-1
Pieruccini-Faria F, Black SE, Masellis M et al (2021) Gait variability across neurodegenerative and cognitive disorders: results from the Canadian Consortium of Neurodegeneration in Aging (CCNA) and the Gait and Brain Study. Alzheimers Dement:1–12. https://doi.org/10.1002/alz.12298
Belghali M, Chastan N, Cignetti F et al (2017) Loss of gait control assessed by cognitive-motor dual-tasks: pros and cons in detecting people at risk of developing Alzheimer’s and Parkinson’s diseases. GeroScience 39:305–329. https://doi.org/10.1007/s11357-017-9977-7
Rucco R, Agosti V, Jacini F et al (2017) Spatio-temporal and kinematic gait analysis in patients with Frontotemporal dementia and Alzheimer’s disease through 3D motion capture. Gait Posture 52:312–317. https://doi.org/10.1016/j.gaitpost.2016.12.021
Jadavji NM, Mosnier H, Kelly E et al (2019) One-carbon metabolism supplementation improves outcome after stroke in aged male MTHFR-deficient mice. Neurobiol Dis 132:1–8. https://doi.org/10.1016/j.nbd.2019.104613
Annerbo S, Wahlund LO, Lökk J (2006) The significance of thyroid-stimulating hormone and homocysteine in the development of Alzheimer’s disease in mild cognitive impairment: a 6-year follow-up study. Am J Alzheimers Dis Other Dement 21:182–188. https://doi.org/10.1177/1533317506289282
Blasko I, Jellinger K, Kemmler G et al (2008) Conversion from cognitive health to mild cognitive impairment and Alzheimer’s disease: prediction by plasma amyloid beta 42, medial temporal lobe atrophy and homocysteine. Neurobiol Aging 29:1–11. https://doi.org/10.1016/j.neurobiolaging.2006.09.002
Gabryelewicz T, Styczynska M, Luczywek E et al (2007) The rate of conversion of mild cognitive impairment to dementia: predictive role of depression. Int J Geriatr Psychiatry 22:563–567. https://doi.org/10.1002/gps.1716
Mattsson N, Ewers M, Rich K et al (2009) CSF biomarkers and incipient Alzheimer disease. JAMA 302:385–393
Slutsky I, Abumaria N, Wu LJ et al (2010) Enhancement of learning and memory by elevating brain magnesiuM. Neuron 65:165–177. https://doi.org/10.1016/j.neuron.2009.12.026
Greengard P, Valtorta F, Czernik AJ, Benfenati F (1993) Synaptic vesicle phosphoproteins and regulation of synaptic function. Science 259:780–785. https://doi.org/10.1126/science.8430330
Polydoro M, Acker CM, Duff K et al (2009) Age-dependent impairment of cognitive and synaptic function in the htau mouse model of Tau pathology. J Neurosci 29:10741–10749. https://doi.org/10.1523/JNEUROSCI.1065-09.2009
Di Meco A, Li JG, Barrero C et al (2019) Elevated levels of brain homocysteine directly modulate the pathological phenotype of a mouse model of tauopathy. Mol Psychiatry 24:1696–1706. https://doi.org/10.1038/s41380-018-0062-0
Germolec DR, Shipkowski KA, Frawley RP, Evans E (2018) Markers of inflammation. Methods Mol Biol 1803:57–79. https://doi.org/10.1007/978-1-4939-8549-4_5
de Araújo Boleti AP, de Oliveira Flores TM, Moreno SE et al (2020) Neuroinflammation: an overview of neurodegenerative and metabolic diseases and of biotechnological studies. Neurochem Int 136:104714. https://doi.org/10.1016/j.neuint.2020.104714
Kotilinek LA, Westerman MA, Wang Q et al (2008) Cyclooxygenase-2 inhibition improves amyloid-β-mediated suppression of memory and synaptic plasticity. Brain 131:651–664. https://doi.org/10.1093/brain/awn008
Tegeder I, Pfeilschifter J, Geisslinger G (2001) Cyclooxygenase-independent actions of cyclooxygenase inhibitors. FASEB J 15:2057–2072. https://doi.org/10.1096/fj.01-0390rev
Ho L, Luterman JD, Aisen PS et al (2000) Elevated CSF prostaglandin E2 levels in patients with probable AD [4] (multiple letters). Neurology 55:323. https://doi.org/10.1212/WNL.55.2.323
Kaufmann WE, Worley PF, Pegg J et al (1996) COX-2, a synaptically induced enzyme, is expressed by excitatory neurons at postsynaptic sites in rat cerebral cortex. Proc Natl Acad Sci U S A 93:2317–2321. https://doi.org/10.1073/pnas.93.6.2317
Bazan NG (2001) COX-2 as a multifunctional neuronal modulator. Nat Med 7:414–415. https://doi.org/10.1038/86477
Tocco G, Freire-Moar J, Schreiber SS et al (1997) Maturational regulation and regional induction of cyclooxygenase-2 in rat brain: implications for Alzheimer’s disease. Exp Neurol 144:339–349. https://doi.org/10.1006/exnr.1997.6429
Sade Yazdi D, Laor Bar-Yosef D, Adsi H et al (2021) Homocysteine fibrillar assemblies display cross-talk with Alzheimer’s disease β-amyloid polypeptide. Proc Natl Acad Sci U S A 118. https://doi.org/10.1073/pnas.2017575118
Wang Q, Walsh DM, Rowan MJ et al (2004) Block of long-term potentiation by naturally secreted and synthetic amyloid β-peptide in hippocampal slices is mediated via activation of the kinases c-Jun N-terminal kinase, cyclin-dependent kinase 5, and p38 mitogen-activated protein kinase as well as M. J Neurosci 24:3370–3378. https://doi.org/10.1523/JNEUROSCI.1633-03.2004
Combs CK, Johnson DE, Karlo JC et al (2000) Inflammatory mechanisms in Alzheimer’s disease: Inhibition of β- amyloid-stimulated proinflammatory responses and neurotoxicity by PPARγ agonists. J Neurosci 20:558–567. https://doi.org/10.1523/jneurosci.20-02-00558.2000
Kaufer D, Friedman A, Seidman S, Soreq H (1998) Acute stress facilitates long-lasting changes in cholinergic gene expression. Nature 393:373–377. https://doi.org/10.1038/30741
Shohami E, Kaufer D, Chen Y et al (2000) Antisense prevention of neuronal damages following head injury in mice. J Mol Med 78:228–236. https://doi.org/10.1007/s001090000104
Pavlov V, Parrish W, Rosas-Ballina M et al (2009) Levels through the cholinergic anti-inflammatory pathway. Brain Behav Immun 23:41–45. https://doi.org/10.1016/j.bbi.2008.06.011.Brain
Pohanka M (2019) Inhibitors of cholinesterases in pharmacology: the current trends. Mini-Rev Med Chem. https://doi.org/10.2174/1389557519666191018170908
Akhtar A, Bishnoi M, Sah SP (2020) Sodium orthovanadate improves learning and memory in intracerebroventricular-streptozotocin rat model of Alzheimer’s disease through modulation of brain insulin resistance induced tau pathology. Brain Res Bull 164:83–97. https://doi.org/10.1016/j.brainresbull.2020.08.001
Liang YQ, Tang XC (2004) Comparative effects of huperzine A, donepezil and rivastigmine on cortical acetylcholine level and acetylcholinesterase activity in rats. Neurosci Lett 361:56–59. https://doi.org/10.1016/j.neulet.2003.12.071
Kaur D, Sharma V, Deshmukh R (2019) Activation of microglia and astrocytes: a roadway to neuroinflammation and Alzheimer’s disease. Inflammopharmacology 27:663–677. https://doi.org/10.1007/s10787-019-00580-x
Michelucci A, Heurtaux T, Grandbarbe L et al (2009) Characterization of the microglial phenotype under specific pro-inflammatory and anti-inflammatory conditions: effects of oligomeric and fibrillar amyloid-β. J Neuroimmunol 210:3–12. https://doi.org/10.1016/j.jneuroim.2009.02.003
Wang Y, Zhu T, Wang M et al (2019) Icariin attenuates M1 activation of microglia and Aβ plaque accumulation in the hippocampus and prefrontal cortex by up-regulating PPARγ in restraint/isolation-stressed APP/PS1 mice. Front Neurosci 13:1–16. https://doi.org/10.3389/fnins.2019.00291
Zhao Q, Xie X, Fan Y et al (2015) Phenotypic dysregulation of microglial activation in young offspring rats with maternal sleep deprivation-induced cognitive impairment. Sci Rep 5:1–9. https://doi.org/10.1038/srep09513
Park J, Min JS, Kim B et al (2015) Mitochondrial ROS govern the LPS-induced pro-inflammatory response in microglia cells by regulating MAPK and NF-κB pathways. Neurosci Lett 584:191–196. https://doi.org/10.1016/j.neulet.2014.10.016
Da Cunha AA, Ferreira AGK, Loureiro SO et al (2012) Chronic hyperhomocysteinemia increases inflammatory markers in hippocampus and serum of rats. Neurochem Res 37:1660–1669. https://doi.org/10.1007/s11064-012-0769-2
Zhang B, Gaiteri C, Bodea LG et al (2013) Integrated systems approach identifies genetic nodes and networks in late-onset Alzheimer’s disease. Cell 153:707–720. https://doi.org/10.1016/j.cell.2013.03.030
Page TH, Turner JJO, Brown AC et al (2010) Nonsteroidal anti-inflammatory drugs increase TNF production in rheumatoid synovial membrane cultures and whole blood. J Immunol 185:3694–3701. https://doi.org/10.4049/jimmunol.1000906
Tröger B, Heidemann M, Osthues I et al (2020) Modulation of S. epidermidis-induced innate immune responses in neonatal whole blood. J Microbiol Immunol Infect 53:240–249. https://doi.org/10.1016/j.jmii.2018.04.008
Kunkel SL, Spengler M, May MA et al (1988) Prostaglandin E2 regulates macrophage-derived tumor necrosis factor gene expression. J Biol Chem 263:5380–5384. https://doi.org/10.1016/s0021-9258(18)60727-6
Stolina M, Sharma S, Lin Y et al (2000) Specific inhibition of cyclooxygenase 2 restores antitumor reactivity by altering the balance of IL-10 and IL-12 synthesis. J Immunol 164:361–370. https://doi.org/10.4049/jimmunol.164.1.361
Härtel C, Von Puttkamer J, Gallner F et al (2004) Dose-dependent immunomodulatory effects of acetylsalicylic acid and indomethacin in human whole blood: Potential role of cyclooxygenase-2 inhibition. Scand J Immunol 60:412–420. https://doi.org/10.1111/j.0300-9475.2004.01481.x
Suabjakyong P, Nishimura K, Toida T, Van Griensven LJLD (2015) Structural characterization and immunomodulatory effects of polysaccharides from Phellinus linteus and Phellinus igniarius on the IL-6/IL-10 cytokine balance of the mouse macrophage cell lines (RAW 264.7). Food Funct 6:2834–2844. https://doi.org/10.1039/c5fo00491h
Xing Z, Gauldie J, Cox G et al (1998) IL-6 is an antiinflammatory cytokine required for controlling local or systemic acute inflammatory responses. J Clin Invest 101:311–320. https://doi.org/10.1172/JCI1368
Eder K, Baffy N, Falus A, Fulop AK (2009) The major inflammatory mediator interleukin-6 and obesity. Inflamm Res 58:727–736. https://doi.org/10.1007/s00011-009-0060-4
Saiki P, Nakajima Y, Van Griensven LJLD, Miyazaki K (2018) Real-time monitoring of IL-6 and IL-10 reporter expression for anti-inflammation activity in live RAW 264.7 cells. Biochem Biophys Res Commun 505:885–890. https://doi.org/10.1016/j.bbrc.2018.09.173
Drago F, Sautière PE, Le Marrec-Croq F et al (2014) Microglia of medicinal leech (Hirudo medicinalis) express a specific activation marker homologous to vertebrate ionized calcium-binding adapter molecule 1 (Iba1/alias aif-1). Dev Neurobiol 74:987–1001. https://doi.org/10.1002/dneu.22179
Yuste JE, Tarragon E, Campuzano CM, Ros-Bernal F (2015) Implications of glial nitric oxide in neurodegenerative diseases. Front Cell Neurosci 9:1–13. https://doi.org/10.3389/fncel.2015.00322
Alderton WK, Cooper CE, Knowles RG (2001) Nitric oxide synthases: structure, function and inhibition. Biochem J 357:593–615. https://doi.org/10.1042/0264-6021:3570593
Niedzielska E, Smaga I, Gawlik M et al (2016) Oxidative stress in neurodegenerative diseases. Mol Neurobiol 53:4094–4125. https://doi.org/10.1007/s12035-015-9337-5
Pohl F, Lin PKT (2018) The potential use of plant natural products and plant extracts with antioxidant properties for the prevention/treatment of neurodegenerative diseases: in vitro, in vivo and clinical trials. Molecules 23. https://doi.org/10.3390/molecules23123283
Van Essen DC, Donahue CJ, Glasser MF (2018) Development and evolution of cerebral and cerebellar cortex. Brain Behav Evol 91:158–169. https://doi.org/10.1159/000489943
dos Santos TM, Siebert C, de Oliveira MF et al (2019) Chronic mild hyperhomocysteinemia impairs energy metabolism, promotes DNA damage and induces a Nrf2 response to oxidative stress in rats brain. Cell Mol Neurobiol 39:687–700. https://doi.org/10.1007/s10571-019-00674-8
Funding
This study was supported by INCT (EN 465671/2014–4)/Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) — Brazil, PRONEX (16/2551–0000465-0)/Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (FAPERGS) —Brazil, and Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ) (E-26/202.701/2019; E-26/010.002422/2019; E-26/010.002260/2019) — Brazil.
Author information
Authors and Affiliations
Contributions
Osmar V. Ramires Júnior: conceptualization, methodology, validation, formal analysis, investigation, data curation, writing—original draft, writing — review and editing, visualization. Tiago M. dos Santos: methodology, validation, formal analysis, investigation. Josiane S. Silveira: methodology and investigation. Raíssa Leite-Aguiar: methodology, validation, formal analysis. Robson Coutinho-Silva funding acquisition. Luiz E. B. Savio: methodology, formal analysis, resource, funding acquisition, review and editing. Angela T. S. Wyse: conceptualization, methodology, validation, formal analysis, resources, writing — original draft, writing — review and editing, visualization, supervision, project administration, funding acquisition.
Corresponding author
Ethics declarations
Ethics Approval
All animal experiments were carried out in accordance with the official government guidelines for the care of animals by the Brazilian Federal Law No. 11,794 of October 8, 2008, which regulates the Brazilian Guidelines for the Care and Use of Animals for Scientific and Educational Purposes, and according to the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health (NIH). The study was approved by the Ethics Committee of the Federal University of Rio Grande do Sul (UFRGS) (36991/2019).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The work has not been published previously, and it is not under consideration for publication elsewhere and, if accepted, it will not be published elsewhere in the same form, in English or any other language, including electronically without the written consent of the copyright holder.
Rights and permissions
About this article
Cite this article
Ramires Junior, O.V., dos Santos, T.M., Silveira, J.S. et al. Rivastigmine Reverses the Decrease in Synapsin and Memory Caused by Homocysteine: Is There Relation to Inflammation?. Mol Neurobiol 59, 4517–4534 (2022). https://doi.org/10.1007/s12035-022-02871-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-022-02871-x