Abstract
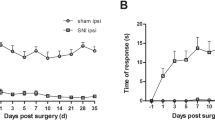
CTK 01512–2 toxin is a recombinant peptide of the Phα1β version derived from the venom of the Phoneutria nigriventer spider. It acts as an N-type voltage-gated calcium channel (VGCC) blocker and shows a prolonged effect on preventing and reducing nociception. Herein, CTK 01512–2 was tested on two models of persistent pain, the chronic post-ischemia pain (CPIP) and the paclitaxel-induced peripheral neuropathy, to evaluate its systemic, intrathecal, and intracerebroventricular effects on mechanical hypersensitivity and thermal allodynia. Glial cell viability was also investigated using the MTT test. The results showed that CTK 01512–2 intrathecal and systemic treatments reduced the mechanical hypersensitivity induced by CPIP, mainly between 1–4 h after its administration. Additionally, intrathecal treatment reduced the CPIP-induced thermal allodynia. In its turn, the intracerebroventricular treatment showed mechanical antihyperalgesic and thermal antiallodynic effects in the paclitaxel-induced peripheral neuropathy. These data reinforce the therapeutic potential of CTK 01512–2 to treat persistent pain conditions and offer a perspective to use the systemic route. Moreover, CTK 01512–2 increased the glial cell viability in the MTT reduction assay, and it may indicate a new approach to managing chronic pain. The results found in this study help to pave new perspectives of pain relief treatments to patients affected by chronic pain.







Similar content being viewed by others
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- CRPS-I:
-
Complex regional pain syndrome-type I
- CPIP:
-
Chronic post-ischemia pain
- IR:
-
Ischemia and reperfusion
- TRP:
-
Transient receptor potential channel
- LAIF:
-
Laboratory of Autoimmunity and Immunopharmacology
- CEUA:
-
Committee on Ethics in the Use of Animals
- ANOVA:
-
Analysis of variance
- ARRIVE:
-
Animal Research: Reporting in vivo Experiments
- CNS:
-
Central nervous system
- IL:
-
Interleukin
- CONCEA:
-
Brazilian Council of Animal Experimentation
- g:
-
Grams
- h:
-
Hours
- i.p.:
-
Intraperitoneal
- kg:
-
Kilograms
- mg:
-
Milligrams
- min:
-
Minutes
- ml:
-
Milliliters
- PTX:
-
Paclitaxel
- PWT:
-
Paw withdrawal threshold
- SEM:
-
Standard error of mean
- mmol:
-
Millimolar
- UFSC:
-
Universidade Federal de Santa Catarina
- AUC:
-
Area under the curve
- μl:
-
Microliters
- LPS:
-
Lipopolysaccharide
- CGRP:
-
Calcitonin gene-related peptide
- MTT:
-
Methyl-thiazolyl diphenyl-tetrazolium bromide
References
Reedijk WB, van Rijn MA, Roelofs K et al (2008) Psychological features of patients with complex regional pain syndrome type I related dystonia. Mov Disord 23:1551–1559. https://doi.org/10.1002/mds.22159
Gierthmühlen J, Binder A, Baron R (2014) Mechanism-based treatment in complex regional pain syndromes. Nat Rev Neurol 10:518–528. https://doi.org/10.1038/nrneurol.2014.140
Tajerian M, Clark JD (2016) New Concepts in Complex Regional Pain Syndrome. Hand Clin 32:41–49. https://doi.org/10.1016/j.hcl.2015.08.003
Coderre TJ, Xanthos DN, Francis L, Bennett GJ (2004) Chronic post-ischemia pain (CPIP): a novel animal model of complex regional pain syndrome-Type I (CRPS-I; reflex sympathetic dystrophy) produced by prolonged hindpaw ischemia and reperfusion in the rat. Pain 112(1–2):94–105. https://doi.org/10.1016/j.pain.2004.08.001
Tang C, Li J, Tai WL et al (2017) Sex differences in complex regional pain syndrome type I (CRPS-I) in mice. J Pain Res 10:1811–1819. https://doi.org/10.2147/JPR.S139365
Vieira G, Cavalli J, Gonçalves ECD et al (2017) Effects of simvastatin beyond dyslipidemia: exploring its Antinociceptive action in an animal model of complex regional pain syndrome-type I. Front Pharmacol 8:584. https://doi.org/10.3389/fphar.2017.00584
Chiba T, Oka Y, Kambe T et al (2016) Paclitaxel-induced peripheral neuropathy increases substance P release in rat spinal cord. Eur J Pharmacol 770:46–51. https://doi.org/10.1016/j.ejphar.2015.11.055
Wilson L, Jordan MA (2004) New Microtubule / Tubulin-Targeted Anticancer Drugs and Novel Chemotherapeutic Strategies. J Chemother 16:83–85. https://doi.org/10.1179/joc.2004.16.Supplement-1.83
Polomano RC, Mannes AJ, Clark US, Bennett GJ (2001) A painful peripheral neuropathy in the rat produced by the chemotherapeutic drug, paclitaxel. Pain 94(3):293–304. https://doi.org/10.1016/S0304-3959(01)00363-3
Cata JP, Weng H-R, Chen J-H, Dougherty PM (2006) Altered discharges of spinal wide dynamic range neurons and down-regulation of glutamate transporter expression in rats with paclitaxel-induced hyperalgesia. Neuroscience 138:329–338. https://doi.org/10.1016/j.neuroscience.2005.11.009
Li Y, North RY, Rhines LD et al (2018) DRG Voltage-Gated Sodium Channel 1.7 Is Upregulated in Paclitaxel-Induced Neuropathy in Rats and in Humans with Neuropathic Pain. J Neurosci 38:1124–1136. https://doi.org/10.1523/JNEUROSCI.0899-17.2017
Silva RBM, Greggio S, Venturin GT et al (2018) Beneficial Effects of the Calcium Channel Blocker CTK 01512–2 in a Mouse Model of Multiple Sclerosis. Mol Neurobiol 55:9307–9327. https://doi.org/10.1007/s12035-018-1049-1
Silva JF da, Binda NS, Pereira EMR, et al (2021) Analgesic effects of Phα1β toxin: a review of mechanisms of action involving pain pathways. J Venom Anim Toxins Incl Trop Dis 27: https://doi.org/10.1590/1678-9199-jvatitd-2021-0001
Rigo FK, Trevisan G, De Prá SD-T et al (2017) The spider toxin Phα1β recombinant possesses strong analgesic activity. Toxicon 133:145–152. https://doi.org/10.1016/j.toxicon.2017.05.018
Wormwood KL, Ngounou Wetie AG, Gomez MV et al (2018) Structural Characterization and Disulfide Assignment of Spider Peptide Phα1β by Mass Spectrometry. J Am Soc Mass Spectrom 29:827–841. https://doi.org/10.1007/s13361-018-1904-3
Peigneur S, de Lima ME, Tytgat J (2018) Phoneutria nigriventer venom: A pharmacological treasure. Toxicon 151:96–110. https://doi.org/10.1016/j.toxicon.2018.07.008
Souza AH, Ferreira J, Cordeiro MDN et al (2008) Analgesic effect in rodents of native and recombinant Phα1β toxin, a high-voltage-activated calcium channel blocker isolated from armed spider venom. Pain 140(1):115–126. https://doi.org/10.1016/j.pain.2008.07.014
Zamponi GW, Striessnig J, Koschak A, Dolphin AC (2015) The Physiology, Pathology, and Pharmacology of Voltage-Gated Calcium Channels and Their Future Therapeutic Potential. Pharmacol Rev 67:821–870. https://doi.org/10.1124/pr.114.009654
Stevens EB, Stephens GJ (2018) Recent advances in targeting ion channels to treat chronic pain. Br J Pharmacol 175:2133–2137. https://doi.org/10.1111/bph.14215
Patel R, Montagut-Bordas C, Dickenson AH (2018) Calcium channel modulation as a target in chronic pain control. Br J Pharmacol 175:2173–2184. https://doi.org/10.1111/bph.13789
Silva RBM, Sperotto NDM, Andrade EL et al (2015) Spinal blockage of P/Q- or N-type voltage-gated calcium channels modulates functional and symptomatic changes related to haemorrhagic cystitis in mice. Br J Pharmacol 172:924–939. https://doi.org/10.1111/bph.12966
Caminski ES, de Freitas LM, Dallegrave E et al (2020) Analgesic effects of the CTK 01512–2 toxin in different models of orofacial pain in rats. Pharmacol Reports 72:600–611. https://doi.org/10.1007/s43440-020-00108-z
Ricardo Carvalho VP, Figueira da Silva J, Buzelin MA et al (2021) Calcium channels blockers toxins attenuate abdominal hyperalgesia and inflammatory response associated with the cerulein-induced acute pancreatitis in rats. Eur J Pharmacol 891:173672. https://doi.org/10.1016/j.ejphar.2020.173672
Tenza-Ferrer H, Magno LAV, Romano-Silva MA et al (2019) Phα1β spider Tpider toxin reverses glial structural plasticity upon peripheral inflammation. Front Cell Neurosci 13:306. https://doi.org/10.3389/fncel.2019.00306
de Souza AH, Castro CJ, Rigo FK et al (2013) An Evaluation of the Antinociceptive Effects of Phα1β, a Neurotoxin from the Spider Phoneutria nigriventer, and ω-Conotoxin MVIIA, a Cone Snail Conus magus Toxin, in Rat Model of Inflammatory and Neuropathic Pain. Cell Mol Neurobiol 33:59–67. https://doi.org/10.1007/s10571-012-9871-x
Rosa F, Trevisan G, Rigo FK et al (2014) Phα1β, a peptide from the venom of the spider phoneutria nigriventer shows antinociceptive effects after continuous infusion in a neuropathic pain model in rats. Anesth Analg 119(1):196–202. https://doi.org/10.1213/ANE.0000000000000249
Antunes FTT, de Souza AH, Caminski ES et al (2021) Neuroprotective effects of the CTK 01512–2 toxin against neurotoxicity induced by 3-nitropropionic acid in rats. Neurotoxicology 87:30–42. https://doi.org/10.1016/j.neuro.2021.08.016
Rigo FK, Trevisan G, Rosa F et al (2013) Spider peptide Phα1β induces analgesic effect in a model of cancer pain. Cancer Sci 104:1226–1230. https://doi.org/10.1111/cas.12209
Nicoletti NF, Erig TC, Zanin RF et al (2017) Pre-clinical evaluation of voltage-gated calcium channel blockers derived from the spider P. nigriventer in glioma progression. Toxicon 129:58–67. https://doi.org/10.1016/j.toxicon.2017.02.001
Ferreira LA, Aoki CT, Santos DC et al (2021) Antinociceptive synergism upon the joint use of methadone and Phα1β in a model of cancer-related pain in C57BL/6J mice. Life Sci 278:119582. https://doi.org/10.1016/j.lfs.2021.119582
de Souza AH, da Costa Lopes AM, Castro CJ et al (2014) The effects of Phα1β, a spider toxin, calcium channel blocker, in a mouse fibromyalgia model. Toxicon 81:37–42. https://doi.org/10.1016/j.toxicon.2014.01.015
Garcia Mendes MP, Carvalho dos Santos D, Rezende MJS et al (2021) Effects of intravenous administration of recombinant Phα1β toxin in a mouse model of fibromyalgia. Toxicon 195:104–110. https://doi.org/10.1016/j.toxicon.2021.03.012
Martel MO, Finan PH, Dolman AJ et al (2015) Self-reports of medication side effects and pain-related activity interference in patients with chronic pain: a longitudinal cohort study. Pain 156:1092–1100. https://doi.org/10.1097/j.pain.0000000000000154
DosSantos MF, Holanda-Afonso RC, Lima RL et al (2014) The role of the blood-brain barrier in the development and treatment of migraine and other pain disorders. Front Cell Neurosci 8:302. https://doi.org/10.3389/fncel.2014.00302
Deer TR, Pope JE, Hanes MC, McDowell GC (2019) Intrathecal Therapy for Chronic Pain: A Review of Morphine and Ziconotide as Firstline Options. Pain Med 20:784–798. https://doi.org/10.1093/pm/pny132
Delhaas EM, Huygen FJPM (2020) Complications associated with intrathecal drug delivery systems. BJA Educ 20:51–57. https://doi.org/10.1016/j.bjae.2019.11.002
McGrath JC, Lilley E (2015) Implementing guidelines on reporting research using animals (ARRIVE etc.): new requirements for publication in BJP. Br J Pharmacol 172:3189–3193. https://doi.org/10.1111/bph.12955
Percie du Sert N, Hurst V, Ahluwalia A et al (2020) The ARRIVE guidelines 2.0: Updated guidelines for reporting animal research. BMC Vet Res 16:242. https://doi.org/10.1186/s12917-020-02451-y
Percie du Sert N, Hurst V, Ahluwalia A et al (2020) The ARRIVE guidelines 2.0: Updated guidelines for reporting animal research. PLoS Biol 18:e3000410–e3000410. https://doi.org/10.1371/journal.pbio.3000410
Millecamps M, Laferrière A, Ragavendran JV et al (2010) Role of peripheral endothelin receptors in an animal model of complex regional pain syndrome type 1 (CRPS-I). Pain 151:174–183. https://doi.org/10.1016/j.pain.2010.07.003
Mazzardo-Martins L, Martins DF, Marcon R et al (2010) High-Intensity Extended Swimming Exercise Reduces Pain-Related Behavior in Mice: Involvement of Endogenous Opioids and the Serotonergic System. J Pain 11:1384–1393. https://doi.org/10.1016/j.jpain.2010.03.015
Costa R, Motta EM, Dutra RC et al (2011) Anti-nociceptive effect of kinin B1 and B2 receptor antagonists on peripheral neuropathy induced by paclitaxel in mice. Br J Pharmacol 164:681–693. https://doi.org/10.1111/j.1476-5381.2011.01408.x
Segat GC, Manjavachi MN, Matias DO et al (2017) Antiallodynic effect of β-caryophyllene on paclitaxel-induced peripheral neuropathy in mice. Neuropharmacology 125:207–219. https://doi.org/10.1016/j.neuropharm.2017.07.015
Stepanenko AA, Dmitrenko VV (2015) Pitfalls of the MTT assay: Direct and off-target effects of inhibitors can result in over/underestimation of cell viability. Gene 574:193–203. https://doi.org/10.1016/j.gene.2015.08.009
dos Santos AQ, Nardin P, Funchal C et al (2006) Resveratrol increases glutamate uptake and glutamine synthetase activity in C6 glioma cells. Arch Biochem Biophys 453:161–167. https://doi.org/10.1016/j.abb.2006.06.025
Bobermin LD, Quincozes-Santos A, Guerra MC et al (2012) Resveratrol Prevents Ammonia Toxicity in Astroglial Cells. PLoS ONE 7:e52164
Webster LR (2015) The Relationship Between the Mechanisms of Action and Safety Profiles of Intrathecal Morphine and Ziconotide: A Review of the Literature. Pain Med 16:1265–1277. https://doi.org/10.1111/pme.12666
Bäckryd E (2018) Do the potential benefits outweigh the risks? An update on the use of ziconotide in clinical practice. Eur J Pain 22:1193–1202. https://doi.org/10.1002/ejp.1229
Hylden JLK, Wilcox GL (1980) Intrathecal morphine in mice: A new technique. Eur J Pharmacol 67:313–316. https://doi.org/10.1016/0014-2999(80)90515-4
Laursen SE, Belknap JK (1986) Intracerebroventricular injections in mice: Some methodological refinements. J Pharmacol Methods 16:355–357. https://doi.org/10.1016/0160-5402(86)90038-0
De Prá SDT, Antoniazzi CTD, Ferro PR et al (2019) Nociceptive mechanisms involved in the acute and chronic phases of a complex regional pain syndrome type 1 model in mice. Eur J Pharmacol 859:172555. https://doi.org/10.1016/j.ejphar.2019.172555
Chen X-Y, Li K, Light AR, Fu K-Y (2013) Simvastatin attenuates formalin-induced nociceptive behaviors by inhibiting microglial RhoA and p38 MAPK activation. J pain 14:1310–1319. https://doi.org/10.1016/j.jpain.2013.05.011
Bortalanza LB, Ferreira J, Hess SC et al (2002) Anti-allodynic action of the tormentic acid, a triterpene isolated from plant, against neuropathic and inflammatory persistent pain in mice. Eur J Pharmacol 453:203–208. https://doi.org/10.1016/S0014-2999(02)02428-7
Gonçalves ECD, Vieira G, Gonçalves TR et al (2021) Bradykinin Receptors Play a Critical Role in the Chronic Post-ischaemia Pain Model. Cell Mol Neurobiol 41:63–78. https://doi.org/10.1007/s10571-020-00832-3
Navratilova E, Nation K, Remeniuk B et al (2020) Selective modulation of tonic aversive qualities of neuropathic pain by morphine in the central nucleus of the amygdala requires endogenous opioid signaling in the anterior cingulate cortex. Pain 161:609–618. https://doi.org/10.1097/j.pain.0000000000001748
Chaplan SR, Bach FW, Pogrel JW et al (1994) Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 53:55–63. https://doi.org/10.1016/0165-0270(94)90144-9
Choi DJ, Choi S-I, Choi B-R et al (2019) Cartilage protective and anti-analgesic effects of ALM16 on monosodium iodoacetate induced osteoarthritis in rats. BMC Complement Altern Med 19:325. https://doi.org/10.1186/s12906-019-2746-7
Flatters SJL, Bennett GJ (2004) Ethosuximide reverses paclitaxel- and vincristine-induced painful peripheral neuropathy. Pain 109(1–2):150–61. https://doi.org/10.1016/j.pain.2004.01.029
Deuis JR, Dvorakova LS, Vetter I (2017) Methods used to evaluate pain behaviors in rodents. Front Mol Neurosci 6(10):284. https://doi.org/10.3389/fnmol.2017.00284
Trevisan G, Maldaner G, Velloso NA et al (2009) Antinociceptive Effects of 14-Membered Cyclopeptide Alkaloids. J Nat Prod 72:608–612. https://doi.org/10.1021/np800377y
Dalenogare DP, Ferro PR, De Prá SDT et al (2019) Antinociceptive activity of Copaifera officinalis Jacq. L oil and kaurenoic acid in mice. Inflammopharmacology 27:829–844. https://doi.org/10.1007/s10787-019-00588-3
Antunes FTT, Angelo SG, Dallegrave E et al (2020) Recombinant peptide derived from the venom the Phoneutria nigriventer spider relieves nociception by nerve deafferentation. Neuropeptides 79:101980. https://doi.org/10.1016/j.npep.2019.101980
Dallegrave E, Taschetto E, Bainy Leal M et al (2018) Acute Toxicity of the Recombinant and Native Phα1β Toxin: New Analgesic from Phoneutria nigriventer Spider Venom. Toxins (Basel) 10:531. https://doi.org/10.3390/toxins10120531
Diniz DM, de Souza AH, Pereira EMR et al (2014) Effects of the calcium channel blockers Phα1β and ω-conotoxin MVIIA on capsaicin and acetic acid-induced visceral nociception in mice. Pharmacol Biochem Behav 126:97–102. https://doi.org/10.1016/j.pbb.2014.09.017
Rigo FK, Dalmolin GD, Trevisan G et al (2013) Effect of ω-conotoxin MVIIA and Phα1β on paclitaxel-induced acute and chronic pain. Pharmacol Biochem Behav 114–115:16–22. https://doi.org/10.1016/j.pbb.2013.10.014
Leppert W, Malec-Milewska M, Zajaczkowska R, Wordliczek J (2018) Transdermal and Topical Drug Administration in the Treatment of Pain. Molecules 23:681. https://doi.org/10.3390/molecules23030681
Nicholson B (2003) Responsible Prescribing of Opioids for the Management of Chronic Pain. Drugs 63:17–32. https://doi.org/10.2165/00003495-200363010-00002
Rigo FK, Rossato MF, Borges V et al (2020) Analgesic and side effects of intravenous recombinant Phα1β. J Venom Anim Toxins Incl Trop Dis 26:e20190070–e20190070. https://doi.org/10.1590/1678-9199-JVATITD-2019-0070
Gerriets V, Anderson J, Nappe TM (2022) Acetaminophen. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island (FL)
Wehling M (2014) Non-steroidal anti-inflammatory drug use in chronic pain conditions with special emphasis on the elderly and patients with relevant comorbidities: management and mitigation of risks and adverse effects. Eur J Clin Pharmacol 70:1159–1172. https://doi.org/10.1007/s00228-014-1734-6
Brune K, Patrignani P (2015) New insights into the use of currently available non-steroidal anti-inflammatory drugs. J Pain Res 8:105–118. https://doi.org/10.2147/JPR.S75160
Manchikanti L, Kaye AM, Knezevic NN et al (2017) Responsible, Safe, and Effective Prescription of Opioids for Chronic Non-Cancer Pain: American Society of Interventional Pain Physicians (ASIPP) Guidelines. Pain Physician 20:S3–S92
Wie CS, Derian A (2022) Ziconotide. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island (FL)
da Silva JF, Binda NS, Pereira EMR et al (2021) Analgesic effects of Phα1β toxin: a review of mechanisms of action involving pain pathways. J Venom Anim Toxins Incl Trop Dis 27:e20210001–e20210001. https://doi.org/10.1590/1678-9199-JVATITD-2021-0001
Tonello R, Fusi C, Materazzi S et al (2017) The peptide Phα1β, from spider venom, acts as a TRPA1 channel antagonist with antinociceptive effects in mice. Br J Pharmacol 174:57–69. https://doi.org/10.1111/bph.13652
Ledeboer A, Liu T, Shumilla JA et al (2006) The glial modulatory drug AV411 attenuates mechanical allodynia in rat models of neuropathic pain. Neuron Glia Biol 2:279–291. https://doi.org/10.1017/S1740925X0700035X
Sisignano M, Angioni C, Park C-K et al (2016) Targeting CYP2J to reduce paclitaxel-induced peripheral neuropathic pain. Proc Natl Acad Sci 113:12544LP – 12549. https://doi.org/10.1073/pnas.1613246113
Zhang H, Yoon S-Y, Zhang H, Dougherty PM (2012) Evidence that spinal astrocytes but not microglia contribute to the pathogenesis of Paclitaxel-induced painful neuropathy. J pain 13:293–303. https://doi.org/10.1016/j.jpain.2011.12.002
Emir TLR (2017) Neurobiology of TRP Channels. CRC Press/Taylor & Francis, Boca Raton (FL)
Julius D (2013) TRP Channels and Pain. Annu Rev Cell Dev Biol 29:355–384. https://doi.org/10.1146/annurev-cellbio-101011-155833
Haraguchi K, Kawamoto A, Isami K et al (2012) TRPM2 Contributes to Inflammatory and Neuropathic Pain through the Aggravation of Pronociceptive Inflammatory Responses in Mice. J Neurosci 32:3931LP – 3941. https://doi.org/10.1523/JNEUROSCI.4703-11.2012
Held K, Kichko T, De Clercq K et al (2015) Activation of TRPM3 by a potent synthetic ligand reveals a role in peptide release. Proc Natl Acad Sci 112:E1363LP – E1372. https://doi.org/10.1073/pnas.1419845112
Xing H, Chen M, Ling J et al (2007) TRPM8 Mechanism of Cold Allodynia after Chronic Nerve Injury. J Neurosci 27:13680LP – 13690. https://doi.org/10.1523/JNEUROSCI.2203-07.2007
Allchorne AJ, Broom DC, Woolf CJ (2005) Detection of Cold Pain, Cold Allodynia and Cold Hyperalgesia in Freely Behaving Rats. Mol Pain 1:1736–1744. https://doi.org/10.1186/1744-8069-1-36
Lippoldt EK, Elmes RR, McCoy DD et al (2013) Artemin, a glial cell line-derived neurotrophic factor family member, induces TRPM8-dependent cold pain. J Neurosci 33:12543–12552. https://doi.org/10.1523/JNEUROSCI.5765-12.2013
Cui Y-Y, Xu H, Wu H-H et al (2014) Spatio-temporal expression and functional involvement of transient receptor potential vanilloid 1 in diabetic mechanical allodynia in rats. PLoS ONE 9:e102052–e102052. https://doi.org/10.1371/journal.pone.0102052
Kremeyer B, Lopera F, Cox JJ et al (2010) A gain-of-function mutation in TRPA1 causes familial episodic pain syndrome. Neuron 66:671–680. https://doi.org/10.1016/j.neuron.2010.04.030
Tonello R, Trevisan G, Luckemeyer D et al (2020) Phα1β, a dual blocker of TRPA1 and Cav2.2, as an adjuvant drug in opioid therapy for postoperative pain. Toxicon 188:80–88. https://doi.org/10.1016/j.toxicon.2020.10.007
Bautista DM, Jordt S-E, Nikai T et al (2006) TRPA1 mediates the inflammatory actions of environmental irritants and proalgesic agents. Cell 124:1269–1282. https://doi.org/10.1016/j.cell.2006.02.023
Honda K, Shinoda M, Furukawa A et al (2014) TRPA1 contributes to capsaicin-induced facial cold hyperalgesia in rats. Eur J Oral Sci 122:391–396. https://doi.org/10.1111/eos.12157
Palhares MR, Silva JF, Rezende MJS et al (2017) Synergistic antinociceptive effect of a calcium channel blocker and a TRPV1 blocker in an acute pain model in mice. Life Sci 182:122–128. https://doi.org/10.1016/j.lfs.2017.06.018
Andrade EL, Meotti FC, Calixto JB (2012) TRPA1 antagonists as potential analgesic drugs. Pharmacol Ther 133:189–204. https://doi.org/10.1016/j.pharmthera.2011.10.008
Story GM, Peier AM, Reeve AJ et al (2003) ANKTM1, a TRP-like Channel Expressed in Nociceptive Neurons, Is Activated by Cold Temperatures. Cell 112:819–829. https://doi.org/10.1016/S0092-8674(03)00158-2
Weng H-J, Patel KN, Jeske NA et al (2015) Tmem100 Is a Regulator of TRPA1-TRPV1 Complex and Contributes to Persistent Pain. Neuron 85:833–846. https://doi.org/10.1016/j.neuron.2014.12.065
Akopian AN (2011) Regulation of Nociceptive Transmission at the Periphery Via TRPA1-TRPV1 Interactions. Curr. Pharm. Biotechnol. 12:89–94
Castro-Junior CJ, Milano J, Souza AH et al (2013) Phα1β toxin prevents capsaicin-induced nociceptive behavior and mechanical hypersensitivity without acting on TRPV1 channels. Neuropharmacology 71:237–246. https://doi.org/10.1016/j.neuropharm.2013.04.001
Loggia ML, Chonde DB, Akeju O et al (2015) Evidence for brain glial activation in chronic pain patients. Brain 138:604–615. https://doi.org/10.1093/brain/awu377
Donnelly CR, Andriessen AS, Chen G et al (2020) Central Nervous System Targets: Glial Cell Mechanisms in Chronic Pain. Neurotherapeutics 17:846–860. https://doi.org/10.1007/s13311-020-00905-7
Sontheimer H (1994) Voltage-dependent ion channels in glial cells. Glia 11:156–172. https://doi.org/10.1002/glia.440110210
de Souza AH, da Rosa LG, Uliano MR et al (2019) Evaluation of DNA damage in spinal cord and mutagenic effect of a Phα1β recombinant toxin with analgesic properties from the Phoneutria nigriventer spider. Basic Clin Pharmacol Toxicol 124:615–620. https://doi.org/10.1111/bcpt.13171
Acknowledgements
We thank the Fundação de Amparo à Pesquisa e Inovação do Estado de Santa Catarina (FAPESC), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Universidade Federal de Santa Catarina (UFSC), Programa de Pós-Graduação em Neurociências (PPGNEURO/UFSC), and Programa INCT-INOVAMED (grant 465430/2014-7), all from Brazil.
Funding
E.C.D.G. and P.M.A are Ph.D. student in the Neuroscience and Health Program, respectively, receiving grants from the CAPES/FAPESC. A.Q.S., M.V.G., and R.C.D. are recipients of a research productivity fellowship from the CNPq.
Author information
Authors and Affiliations
Contributions
Study design and concept, and manuscript writing: JC, PMA, ECDG, LDB, AQS, RCD; experiment implementation and manuscript drafting: JC, PMA, ECDG, LDB, AQS, RCD; figure production: JC, PMA, RCD; data analysis: JC, LDB, AQS, RCD; experiment support: JC, ECDG, LDB, AQS, RCD; the manuscript draft was critically revised by JC, LDB, AQS, NRBR, MVG, RCD. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The manuscript does not contain clinical studies or patient data. The Animal Ethics Committee approved all procedures in this study involving animals of the Universidade Federal de Santa Catarina (CEUA/UFSC, protocol number 3914220319). All of the experimental procedures were conducted according to the guidelines of CONCEA and CEUA/UFSC, based on the principles of the 3Rs (Replacement, Reduction, and Refinement).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Code Availability
Not applicable.
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cavalli, J., de Assis, P.M., Cristina Dalazen Gonçalves, E. et al. Systemic, Intrathecal, and Intracerebroventricular Antihyperalgesic Effects of the Calcium Channel Blocker CTK 01512–2 Toxin in Persistent Pain Models. Mol Neurobiol 59, 4436–4452 (2022). https://doi.org/10.1007/s12035-022-02864-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-022-02864-w