Abstract
Focal cortical dysplasia (FCD) is associated with blood-brain barrier (BBB) dysfunction in patients with difficult-to-treat epilepsy. However, the underlying cellular and molecular factors in cortical dysplasia (CD) associated with progressive neurovascular challenges during the pro-epileptic phase, post-seizure, and during epileptogenesis remain unclear. We studied the BBB function in a rat model of congenital (in utero radiation-induced, first hit) CD and longitudinally examined the cortical brain tissues at baseline and the progressive neurovascular alterations, glucose transporter-1 (GLUT1) expression, and glucose metabolic activity at 2, 15, and 30 days following a second hit using pentylenetetrazole-induced seizure. Our study revealed through immunoblotting, immunohistochemistry, and biochemical analysis that (1) altered vascular density and prolongation of BBB albumin leakages in CD rats continued through 30 days post-seizure; (2) CD brain tissues showed elevated matrix metalloproteinase-9 levels at 2 days post-seizure and microglial overactivation through 30 days post-seizure; (3) BBB tight junction protein and GLUT1 levels were decreased and neuronal monocarboxylate transporter-2 (MCT2) and mammalian target of rapamycin (mTOR) levels were increased in the CD rat brain: (4) ATPase activity is elevated and a low glucose/high lactate imbalance exists in CD rats; and (5) the mTOR pathway is activated and MCT2 levels are elevated in the presence of high lactate during glucose starvation in vitro. Together, this study suggests that BBB dysfunction, including decreased GLUT1 expression and metabolic disturbance, may contribute to epileptogenesis in this CD rat model through multiple mechanisms that could be translated to FCD therapy in medically refractory epilepsy.







Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request. Some data may not be made available because of privacy or ethical restrictions.
References
Neuwelt EA, Bauer B, Fahlke C, Fricker G, Iadecola C, Janigro D, Leybaert L, Molnar Z, O'Donnell ME, Povlishock JT, Saunders NR, Sharp F, Stanimirovic D, Watts RJ, Drewes LR (2011) Engaging neuroscience to advance translational research in brain barrier biology. Nat Rev Neurosci 12(3):169–182. https://doi.org/10.1038/nrn2995
Zlokovic BV (2008) The blood-brain barrier in health and chronic neurodegenerative disorders. Neuron 57(2):178–201. https://doi.org/10.1016/j.neuron.2008.01.003
Gorter JA, Aronica E, van Vliet EA (2019) The roof is leaking and a storm is raging: repairing the blood-brain barrier in the fight against epilepsy. Epilepsy Curr 19(3):177–181. https://doi.org/10.1177/1535759719844750
Seiffert E, Dreier JP, Ivens S, Bechmann I, Tomkins O, Heinemann U, Friedman A (2004) Lasting blood-brain barrier disruption induces epileptic focus in the rat somatosensory cortex. J Neurosci 24(36):7829–7836. https://doi.org/10.1523/JNEUROSCI.1751-04.2004
van Vliet EA, da Costa AS, Redeker S, van Schaik R, Aronica E, Gorter JA (2007) Blood-brain barrier leakage may lead to progression of temporal lobe epilepsy. Brain 130(Pt 2):521–534. https://doi.org/10.1093/brain/awl318
Weissberg I, Reichert A, Heinemann U, Friedman A (2011) Blood-brain barrier dysfunction in epileptogenesis of the temporal lobe. Epilepsy Res Treat 2011:143908. https://doi.org/10.1155/2011/143908
Abbott NJ, Patabendige AA, Dolman DE, Yusof SR, Begley DJ (2010) Structure and function of the blood-brain barrier. Neurobiol Dis 37(1):13–25. https://doi.org/10.1016/j.nbd.2009.07.030
Williams S, Hossain M, Ferguson L, Busch RM, Marchi N, Gonzalez-Martinez J, Perucca E, Najm IM, Ghosh C (2019) Neurovascular drug biotransformation machinery in focal human epilepsies: brain CYP3A4 correlates with seizure frequency and antiepileptic drug therapy. Mol Neurobiol 56(12):8392–8407. https://doi.org/10.1007/s12035-019-01673-y
Raabe A, Schmitz AK, Pernhorst K, Grote A, von der Brelie C, Urbach H, Friedman A, Becker AJ, Elger CE, Niehusmann P (2012) Cliniconeuropathologic correlations show astroglial albumin storage as a common factor in epileptogenic vascular lesions. Epilepsia 53(3):539–548. https://doi.org/10.1111/j.1528-1167.2012.03405.x
Scott RC (2014) What are the effects of prolonged seizures in the brain? Epileptic Disord 16 Spec No 1(S6-11). https://doi.org/10.1684/epd.2014.0689
Tomkins O, Shelef I, Kaizerman I, Eliushin A, Afawi Z, Misk A, Gidon M, Cohen A, Zumsteg D, Friedman A (2008) Blood-brain barrier disruption in post-traumatic epilepsy. J Neurol Neurosurg Psychiatry 79(7):774–777. https://doi.org/10.1136/jnnp.2007.126425
Lee SK, Kim DW (2013) Focal cortical dysplasia and epilepsy surgery. J Epilepsy Res 3(2):43–47. https://doi.org/10.14581/jer.13009
Najm IM, Ying Z, Babb T, Mohamed A, Hadam J, LaPresto E, Wyllie E, Kotagal P, Bingaman W, Foldvary N, Morris H, Luders HO (2000) Epileptogenicity correlated with increased N-methyl-D-aspartate receptor subunit NR2A/B in human focal cortical dysplasia. Epilepsia 41(8):971–976. https://doi.org/10.1111/j.1528-1157.2000.tb00281.x
Lapilover EG, Lippmann K, Salar S, Maslarova A, Dreier JP, Heinemann U, Friedman A (2012) Peri-infarct blood-brain barrier dysfunction facilitates induction of spreading depolarization associated with epileptiform discharges. Neurobiol Dis 48(3):495–506. https://doi.org/10.1016/j.nbd.2012.06.024
Ivens S, Gabriel S, Greenberg G, Friedman A, Shelef I (2010) Blood-brain barrier breakdown as a novel mechanism underlying cerebral hyperperfusion syndrome. J Neurol 257(4):615–620. https://doi.org/10.1007/s00415-009-5384-z
Leen WG, Taher M, Verbeek MM, Kamsteeg EJ, van de Warrenburg BP, Willemsen MA (2014) GLUT1 deficiency syndrome into adulthood: a follow-up study. J Neurol 261(3):589–599. https://doi.org/10.1007/s00415-014-7240-z
Stafstrom CE (2006) Epilepsy: a review of selected clinical syndromes and advances in basic science. J Cereb Blood Flow Metab 26(8):983–1004. https://doi.org/10.1038/sj.jcbfm.9600265
Van Skike CE, Jahrling JB, Olson AB, Sayre NL, Hussong SA, Ungvari Z, Lechleiter JD, Galvan V (2018) Inhibition of mTOR protects the blood-brain barrier in models of Alzheimer's disease and vascular cognitive impairment. Am J Physiol Heart Circ Physiol 314(4):H693–H703. https://doi.org/10.1152/ajpheart.00570.2017
Jansen LA, Mirzaa GM, Ishak GE, O'Roak BJ, Hiatt JB, Roden WH, Gunter SA, Christian SL, Collins S, Adams C, Riviere JB, St-Onge J, Ojemann JG, Shendure J, Hevner RF, Dobyns WB (2015) PI3K/AKT pathway mutations cause a spectrum of brain malformations from megalencephaly to focal cortical dysplasia. Brain 138(Pt 6):1613–1628. https://doi.org/10.1093/brain/awv045
Lim JS, Kim WI, Kang HC, Kim SH, Park AH, Park EK, Cho YW, Kim S, Kim HM, Kim JA, Kim J, Rhee H, Kang SG, Kim HD, Kim D, Kim DS, Lee JH (2015) Brain somatic mutations in MTOR cause focal cortical dysplasia type II leading to intractable epilepsy. Nat Med 21(4):395–400. https://doi.org/10.1038/nm.3824
Nakashima M, Saitsu H, Takei N, Tohyama J, Kato M, Kitaura H, Shiina M, Shirozu H, Masuda H, Watanabe K, Ohba C, Tsurusaki Y, Miyake N, Zheng Y, Sato T, Takebayashi H, Ogata K, Kameyama S, Kakita A, Matsumoto N (2015) Somatic mutations in the MTOR gene cause focal cortical dysplasia type IIb. Ann Neurol 78(3):375–386. https://doi.org/10.1002/ana.24444
Nemes AD, Ayasoufi K, Ying Z, Zhou QG, Suh H, Najm IM (2017) Growth associated protein 43 (GAP-43) as a novel target for the diagnosis, treatment and prevention of epileptogenesis. Sci Rep 7(1):17702. https://doi.org/10.1038/s41598-017-17377-z
Nemes AD, O'Dwyer R, Najm IM, Ying Z, Gonzalez-Martinez J, Alexopoulos AV (2017) Treatment with lacosamide impedes generalized seizures in a rodent model of cortical dysplasia. Epilepsia 58(10):1755–1761. https://doi.org/10.1111/epi.13856
Oghlakian RO, Tilelli CQ, Hiremath GK, Alexopoulos AV, Najm IM (2009) Single injection of a low dose of pentylenetetrazole leads to epileptogenesis in an animal model of cortical dysplasia. Epilepsia 50(4):801–810. https://doi.org/10.1111/j.1528-1167.2008.01815.x
Cavaglia M, Dombrowski SM, Drazba J, Vasanji A, Bokesch PM, Janigro D (2001) Regional variation in brain capillary density and vascular response to ischemia. Brain Res 910(1-2):81–93. https://doi.org/10.1016/s0006-8993(01)02637-3
Marchi N, Betto G, Fazio V, Fan Q, Ghosh C, Machado A, Janigro D (2009) Blood-brain barrier damage and brain penetration of antiepileptic drugs: role of serum proteins and brain edema. Epilepsia 50(4):664–677. https://doi.org/10.1111/j.1528-1167.2008.01989.x
Hossain M, Williams S, Ferguson L, Bingaman W, Ghosh A, Najm IM, Ghosh C (2020) Heat shock proteins accelerate the maturation of brain endothelial cell glucocorticoid receptor in focal human drug-resistant epilepsy. Mol Neurobiol. https://doi.org/10.1007/s12035-020-02043-9
Lauritzen F, Perez EL, Melillo ER, Roh JM, Zaveri HP, Lee TS, Wang Y, Bergersen LH, Eid T (2012) Altered expression of brain monocarboxylate transporter 1 in models of temporal lobe epilepsy. Neurobiol Dis 45(1):165–176. https://doi.org/10.1016/j.nbd.2011.08.001
Hutter-Schmid B, Kniewallner KM, Humpel C (2015) Organotypic brain slice cultures as a model to study angiogenesis of brain vessels. Front Cell Dev Biol 3:52. https://doi.org/10.3389/fcell.2015.00052
Ghosh C, Hossain M, Mishra S, Khan S, Gonzalez-Martinez J, Marchi N, Janigro D, Bingaman W, Najm I (2018) Modulation of glucocorticoid receptor in human epileptic endothelial cells impacts drug biotransformation in an in vitro blood-brain barrier model. Epilepsia. https://doi.org/10.1111/epi.14567
Ghosh C, Hossain M, Spriggs A, Ghosh A, Grant GA, Marchi N, Perucca E, Janigro D (2015) Sertraline-induced potentiation of the CYP3A4-dependent neurotoxicity of carbamazepine: an in vitro study. Epilepsia 56(3):439–449. https://doi.org/10.1111/epi.12923
Shaw G, Morse S, Ararat M, Graham FL (2002) Preferential transformation of human neuronal cells by human adenoviruses and the origin of HEK 293 cells. FASEB J 16(8):869–871. https://doi.org/10.1096/fj.01-0995fje
Loscher W, Potschka H, Sisodiya SM, Vezzani A (2020) Drug resistance in epilepsy: clinical impact, potential mechanisms, and new innovative treatment options. Pharmacol Rev 72(3):606–638. https://doi.org/10.1124/pr.120.019539
Friedman A (2011) Blood-brain barrier dysfunction, status epilepticus, seizures, and epilepsy: a puzzle of a chicken and egg? Epilepsia 52(Suppl 8):19–20. https://doi.org/10.1111/j.1528-1167.2011.03227.x
Friedman A, Dingledine R (2011) Molecular cascades that mediate the influence of inflammation on epilepsy. Epilepsia 52(Suppl 3):33–39. https://doi.org/10.1111/j.1528-1167.2011.03034.x
van Vliet EA, Aronica E, Gorter JA (2014) Role of blood-brain barrier in temporal lobe epilepsy and pharmacoresistance. Neuroscience 277:455–473. https://doi.org/10.1016/j.neuroscience.2014.07.030
Najm IM, Tilelli CQ, Oghlakian R (2007) Pathophysiological mechanisms of focal cortical dysplasia: a critical review of human tissue studies and animal models. Epilepsia 48(Suppl 2):21–32. https://doi.org/10.1111/j.1528-1167.2007.01064.x
Salar S, Maslarova A, Lippmann K, Nichtweiss J, Weissberg I, Sheintuch L, Kunz WS, Shorer Z, Friedman A, Heinemann U (2014) Blood-brain barrier dysfunction can contribute to pharmacoresistance of seizures. Epilepsia 55(8):1255–1263. https://doi.org/10.1111/epi.12713
Wintermark P, Lechpammer M, Warfield SK, Kosaras B, Takeoka M, Poduri A, Madsen JR, Bergin AM, Whalen S, Jensen FE (2013) Perfusion imaging of focal cortical dysplasia using arterial spin labeling: correlation with histopathological vascular density. J Child Neurol 28(11):1474–1482. https://doi.org/10.1177/0883073813488666
Deng Z, Huang H, Wu X, Wu M, He G, Guo J (2017) Distinct expression of various angiogenesis factors in mice brain after whole-brain irradiation by X-ray. Neurochem Res 42(2):625–633. https://doi.org/10.1007/s11064-016-2118-3
Vezzani A, Aronica E, Mazarati A, Pittman QJ (2013) Epilepsy and brain inflammation. Exp Neurol 244:11–21. https://doi.org/10.1016/j.expneurol.2011.09.033
Imai Y, Ibata I, Ito D, Ohsawa K, Kohsaka S (1996) A novel gene iba1 in the major histocompatibility complex class III region encoding an EF hand protein expressed in a monocytic lineage. Biochem Biophys Res Commun 224(3):855–862. https://doi.org/10.1006/bbrc.1996.1112
Ito D, Imai Y, Ohsawa K, Nakajima K, Fukuuchi Y, Kohsaka S (1998) Microglia-specific localisation of a novel calcium binding protein, Iba1. Brain Res Mol Brain Res 57(1):1–9. https://doi.org/10.1016/s0169-328x(98)00040-0
Ohsawa K, Imai Y, Kanazawa H, Sasaki Y, Kohsaka S (2000) Involvement of Iba1 in membrane ruffling and phagocytosis of macrophages/microglia. J Cell Sci 113(Pt 17):3073–3084
Bronisz E, Kurkowska-Jastrzebska I (2016) Matrix metalloproteinase 9 in epilepsy: the role of neuroinflammation in seizure development. Mediat Inflamm 2016:7369020. https://doi.org/10.1155/2016/7369020
Liu JY, Thom M, Catarino CB, Martinian L, Figarella-Branger D, Bartolomei F, Koepp M, Sisodiya SM (2012) Neuropathology of the blood-brain barrier and pharmaco-resistance in human epilepsy. Brain 135(Pt 10):3115–3133. https://doi.org/10.1093/brain/aws147
Jha MK, Morrison BM (2018) Glia-neuron energy metabolism in health and diseases: new insights into the role of nervous system metabolic transporters. Exp Neurol 309:23–31. https://doi.org/10.1016/j.expneurol.2018.07.009
Leroy C, Pierre K, Simpson IA, Pellerin L, Vannucci SJ, Nehlig A (2011) Temporal changes in mRNA expression of the brain nutrient transporters in the lithium-pilocarpine model of epilepsy in the immature and adult rat. Neurobiol Dis 43(3):588–597. https://doi.org/10.1016/j.nbd.2011.05.007
Zeng LH, Rensing NR, Wong M (2009) The mammalian target of rapamycin signaling pathway mediates epileptogenesis in a model of temporal lobe epilepsy. J Neurosci 29(21):6964–6972. https://doi.org/10.1523/JNEUROSCI.0066-09.2009
Huang C, Sheng S, Li R, Sun X, Liu J, Huang G (2015) Lactate promotes resistance to glucose starvation via upregulation of Bcl-2 mediated by mTOR activation. Oncol Rep 33(2):875–884. https://doi.org/10.3892/or.2014.3655
Hegde M, Lowenstein DH (2014) The search for circulating epilepsy biomarkers. Biomark Med 8(3):413–427. https://doi.org/10.2217/bmm.13.142
Marin-Valencia I, Good LB, Ma Q, Duarte J, Bottiglieri T, Sinton CM, Heilig CW, Pascual JM (2012) Glut1 deficiency (G1D): epilepsy and metabolic dysfunction in a mouse model of the most common human phenotype. Neurobiol Dis 48(1):92–101. https://doi.org/10.1016/j.nbd.2012.04.011
Jiang X, Kenerson H, Aicher L, Miyaoka R, Eary J, Bissler J, Yeung RS (2008) The tuberous sclerosis complex regulates trafficking of glucose transporters and glucose uptake. Am J Pathol 172(6):1748–1756. https://doi.org/10.2353/ajpath.2008.070958
Code Availability
Not applicable.
Funding
This work is supported in part by the National Institute of Neurological Disorders and Stroke/National Institutes of Health grant R01NS095825 awarded to Chaitali Ghosh.
Author information
Authors and Affiliations
Contributions
CG designed the experiments and wrote the manuscript. RM performed the immunohistochemistry (DAB) staining, immunohistochemistry analyses, quantification, and cell culture experiments. CO, SW, and MN cared for and treated the animals for the experiments and obtained the cortical brain tissue specimens used for analysis with the assistance of CG and IN. In addition, SW performed initial histological and immunohistochemistry staining (fluorescent) and analysis. MH performed the western blot and biochemical assays. XL performed the statistical analysis of the data. All the authors contributed to editing the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
All animal procedures were approved by the Animal Research Committee of Cleveland Clinic Foundation. All studies were performed in accordance with the approved guidelines by the Institutional Animal Care and Use Committee and the Institutional Biosafety Committee of Cleveland Clinic. All efforts were to minimize animal suffering.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Declarations
Conflict of Interest
IN serves on the Speaker Bureau for Eisai, Inc., and as a member of ad hoc advisory board for Eisai, Inc. and LivaNova. None of the other authors has any potential conflict of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information

Supplemental Fig. 1
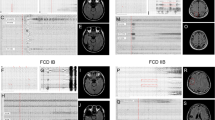
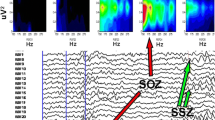
General experimental design and rat groups. NL, XRT (irradiated in utero), PTZ (seizure-induced/SE) and XRT+PTZ and the overall experimental outline is depicted (PNG 2013 kb)

Supplemental Fig. 2
Long-lasting BBB disruption post-seizure induction in rats with CD. FITC-albumin leakage as a surrogate of BBB disruption was followed with and without seizure induction in CD rats. The representative images of the brain cortex after 2 days post-PTZ (PND47), 15 days post-PTZ (PND60) and 30 days post-PTZ (PND75) show increased FITC-albumin extravasation in XRT, PTZ and XRT+PTZ cortical tissues compared to normal (NL). Quantification of BBB leakage in these areas was performed using Image J software. Increased BBB albumin leakage to the brain parenchyma was consistently elevated in the XRT+PTZ cortex, which continued until 30 days post-PTZ compared to NL. The result was expressed as mean ± SEM by two-way ANOVA, ***p<0.001. Scale bar = 200 μm (PNG 1105 kb)

Supplemental Fig. 3
GFAP expression post-seizure induction in rats with cortical malformation. GFAP (red) immunostaining showed slightly upregulated glial cell activation (reactive gliosis) in XRT+PTZ cortex regions with FITC-albumin (green) leakages in rats. Activated astrocytes were not observed in the PTZ group at 30 days post-PTZ (PND75). Scale bar = 200 μm (PND47) and 50 μm (PND75) (PNG 4015 kb)

Supplemental Fig. 4
Full western blots (a-e) for all targets analyzed. The representative blots from western blot analysis of MMP-9, Claudin-5, Claudin-1, GLUT1, mTOR, the mTOR pathway panel and MCT2 are provided with their corresponding β-actins (PNG 2037 kb)

Supplemental Fig. 5
Glucose and lactate absolute levels. Cortical glucose and lactate levels were measured and plotted in mmol/L in normal (NL), XRT, PTZ and XRT+PTZ rats. The glucose levels were significantly lower in XRT and XRT+PTZ compared to NL at PND47, PND60 and PND75. The PTZ group’s glucose levels were significantly increased at PND47 but returned to NL by PND60. Simultaneously increased lactate levels were seen in XRT and XRT+PTZ rats at PND47 but returned back to normal by PND75 (PNG 380 kb)

Supplemental Fig. 6
Exogenous high lactate treatment effect on mTOR pathway and lactate transporter in vitro. Increased protein expression of phospho-mTOR (Ser2448), phospho-S6K (Ser371) and MCT2 is found in human embryonic kidney (HEK) cells after lactate (20 mM) treatment during glucose starvation vs. normal glucose media (0 mM lactate) control, examined by western blot. β-actin is used for normalization. The results are expressed as mean ± SEM by two-sample t-test, **p<0.01, ***p<0.001 (PNG 381 kb)
Supplemental Table 1
(DOCX 25 kb)
Rights and permissions
About this article
Cite this article
Ghosh, C., Myers, R., O’Connor, C. et al. Cortical Dysplasia in Rats Provokes Neurovascular Alterations, GLUT1 Dysfunction, and Metabolic Disturbances That Are Sustained Post-Seizure Induction. Mol Neurobiol 59, 2389–2406 (2022). https://doi.org/10.1007/s12035-021-02624-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-021-02624-2