Abstract
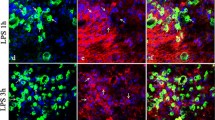
Regulation of microglial activation and neuroinflammation are critical factors in the pathogenesis of ischemic brain injury. Interest in protease-activated receptor 2 (PAR2) as a pharmaceutical target for various diseases is creasing. However, it is unclear the expression and functions of PAR2 in hypoxia-ischemic (HI) brain injury. Mice with HI and cells with oxygen–glucose deprivation and reoxygenation (OGD/R) were studied. Immunoblot and qRT-PCR were used to study the differential gene expression in cultured microglia and neurons. Immunofluorescent staining was used to study the expression pattern of PAR2 in the HI brain and phagocytotic activity of microglia after OGD/R. In neonatal mice brain after HI, we found PAR2 expression was abundant in neurons, but barely in microglia from the contralateral side of cortex and hippocampus. Conversely, PAR2 expression was barely in neurons while significantly increased in activated microglia from the ipsilateral side of cortex and hippocampus. The activations of PAR2 were increased in both microglia and neuron in a cell model of OGD/R. PAR2 activation mediated the cross-talk between microglia and neurons including the following: microglial PAR2 mediated inflammatory responses that induced neuronal damage; neuronal PAR2 regulated chemokines that recruited activated microglia to damage area; microglia PAR2 controlled the phagocytosis of degenerating neurons. These data suggested differential expression and distinct roles of PAR2 in microglia and neurons after HI injury; thereby, interventions targeting PAR2 may provide insights into the inflammatory-related diseases.





Similar content being viewed by others
Data Availability
The data used in this study are available from the corresponding authors upon reasonable request.
Abbreviations
- CatB:
-
Cathepsin B
- CCK-8:
-
Cell-Counting Kit
- CCL2:
-
C–C motif chemokine ligand 2
- CLSM:
-
Confocal laser scanning microscope
- CNS:
-
Central nervous system
- CXCL1:
-
C-X-C motif chemokine ligand 1
- DDW:
-
Double-distilled water
- DMEM:
-
Dulbecco’s modified Eagle’s medium
- FBS:
-
Fetal bovine serum
- FSR:
-
FSLLRY-NH2
- HAND:
-
HIV-associated neurocognitive disorders
- HE:
-
Hematoxylin–eosin
- HI:
-
Hypoxia–ischemia
- HRP:
-
Horseradish peroxidase
- IL-1β:
-
Interleukin-1β
- MCM:
-
Microglia-conditioned medium
- NF-κB:
-
Nuclear factor kappa B
- OGD/R:
-
Oxygen–glucose deprivation and reoxygenation
- PAR2:
-
Protease-activated receptor 2
- PBS:
-
Phosphate buffer saline
- PEI:
-
Polyethyleneimine
- PFA:
-
Paraformaldehyde
- SD:
-
Standard deviation
- SDS:
-
Sodium dodecyl sulfate
- TNF-α:
-
Tumor necrosis factor-α
References
Al Ahmad A, Gassmann M, Ogunshola OO (2012) Involvement of oxidative stress in hypoxia-induced blood-brain barrier breakdown. Microvasc Res 84(2):222–225. https://doi.org/10.1016/j.mvr.2012.05.008
Muntsant A, Shrivastava K, Recasens M, Gimenez-Llort L (2019) Severe perinatal hypoxic-ischemic brain injury induces long-term sensorimotor deficits, anxiety-like behaviors and cognitive impairment in a sex-, age- and task-selective manner in C57BL/6 mice but can be modulated by neonatal handling. Front Behav Neurosci 13:7. https://doi.org/10.3389/fnbeh.2019.00007
Umekawa T, Osman AM, Han W, Ikeda T, Blomgren K (2015) Resident microglia, rather than blood-derived macrophages, contribute to the earlier and more pronounced inflammatory reaction in the immature compared with the adult hippocampus after hypoxia-ischemia. Glia 63(12):2220–2230. https://doi.org/10.1002/glia.22887
Ni J, Wu Z, Peterts C, Yamamoto K, Qing H, Nakanishi H (2015) The critical role of proteolytic relay through cathepsins B and E in the phenotypic change of microglia/macrophage. J Neurosci 35(36):12488–12501. https://doi.org/10.1523/JNEUROSCI.1599-15.2015
Koike M, Shibata M, Tadakoshi M, Gotoh K, Komatsu M, Waguri S, Kawahara N, Kuida K et al (2008) Inhibition of autophagy prevents hippocampal pyramidal neuron death after hypoxic-ischemic injury. Am J Pathol 172(2):454–469. https://doi.org/10.2353/ajpath.2008.070876
Sheldon RA, Hall JJ, Noble LJ, Ferriero DM (2001) Delayed cell death in neonatal mouse hippocampus from hypoxia-ischemia is neither apoptotic nor necrotic. Neurosci Lett 304(3):165–168. https://doi.org/10.1016/s0304-3940(01)01788-8
Kerschensteiner M, Meinl E, Hohlfeld R (2010) Neuro-immune crosstalk in CNS diseases. Results Probl Cell Differ 51:197–216. https://doi.org/10.1007/400_2009_6
Biber K, Neumann H, Inoue K, Boddeke HW (2007) Neuronal ‘on’ and ‘off’ signals control microglia. Trends Neurosci 30(11):596–602. https://doi.org/10.1016/j.tins.2007.08.007
Marinelli S, Basilico B, Marrone MC, Ragozzino D (2019) Microglia-neuron crosstalk: signaling mechanism and control of synaptic transmission. Semin Cell Dev Biol 94:138–151. https://doi.org/10.1016/j.semcdb.2019.05.017
Vu TK, Hung DT, Wheaton VI, Coughlin SR (1991) Molecular cloning of a functional thrombin receptor reveals a novel proteolytic mechanism of receptor activation. Cell 64(6):1057–1068. https://doi.org/10.1016/0092-8674(91)90261-v
Gerszten RE, Chen J, Ishii M, Ishii K, Wang L, Nanevicz T, Turck CW, Vu TK et al (1994) Specificity of the thrombin receptor for agonist peptide is defined by its extracellular surface. Nature 368(6472):648–651. https://doi.org/10.1038/368648a0
Noorbakhsh F, Tsutsui S, Vergnolle N, Boven LA, Shariat N, Vodjgani M, Warren KG, Andrade-Gordon P et al (2006) Proteinase-activated receptor 2 modulates neuroinflammation in experimental autoimmune encephalomyelitis and multiple sclerosis. J Exp Med 203(2):425–435. https://doi.org/10.1084/jem.20052148
Bushell TJ, Cunningham MR, McIntosh KA, Moudio S, Plevin R (2016) Protease-activated receptor 2: are common functions in glial and immune cells linked to inflammation-related CNS disorders? Curr Drug Targets 17(16):1861–1870. https://doi.org/10.2174/1389450117666151209115232
Liu Y, Wu Z, Nakanishi Y, Ni J, Hayashi Y, Takayama F, Zhou Y, Kadowaki T et al (2017) Infection of microglia with Porphyromonas gingivalis promotes cell migration and an inflammatory response through the gingipain-mediated activation of protease-activated receptor-2 in mice. Sci Rep 7(1):11759. https://doi.org/10.1038/s41598-017-12173-1
Jin G, Hayashi T, Kawagoe J, Takizawa T, Nagata T, Nagano I, Syoji M, Abe K (2005) Deficiency of PAR-2 gene increases acute focal ischemic brain injury. J Cereb Blood Flow Metab 25(3):302–313. https://doi.org/10.1038/sj.jcbfm.9600021
Noorbakhsh F, Vergnolle N, McArthur JC, Silva C, Vodjgani M, Andrade-Gordon P, Hollenberg MD, Power C (2005) Proteinase-activated receptor-2 induction by neuroinflammation prevents neuronal death during HIV infection. J Immunol 174(11):7320–7329. https://doi.org/10.4049/jimmunol.174.11.7320
Svensson KJ, Kucharzewska P, Christianson HC, Skold S, Lofstedt T, Johansson MC, Morgelin M, Bengzon J et al (2011) Hypoxia triggers a proangiogenic pathway involving cancer cell microvesicles and PAR-2-mediated heparin-binding EGF signaling in endothelial cells. Proc Natl Acad Sci U S A 108(32):13147–13152. https://doi.org/10.1073/pnas.1104261108
Vannucci RC, Vannucci SJ (1997) A model of perinatal hypoxic-ischemic brain damage. Ann N Y Acad Sci 835:234–249. https://doi.org/10.1111/j.1749-6632.1997.tb48634.x
Rice JE 3rd, Vannucci RC, Brierley JB (1981) The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann Neurol 9(2):131–141. https://doi.org/10.1002/ana.410090206
Ni J, Wu Z, Stoka V, Meng J, Hayashi Y, Peters C, Qing H, Turk V et al (2019) Increased expression and altered subcellular distribution of cathepsin B in microglia induce cognitive impairment through oxidative stress and inflammatory response in mice. Aging Cell 18(1):e12856. https://doi.org/10.1111/acel.12856
Meng J, Liu Y, Xie Z, Qing H, Lei P, Ni J (2020) Nucleus distribution of cathepsin B in senescent microglia promotes brain aging through degradation of sirtuins. Neurobiol Aging 96:255–266. https://doi.org/10.1016/j.neurobiolaging.2020.09.001
Jiang M, Meng J, Zeng F, Qing H, Hook G, Hook V, Wu Z, Ni J (2020) Cathepsin B inhibition blocks neurite outgrowth in cultured neurons by regulating lysosomal trafficking and remodeling. J Neurochem 155(3):300–312. https://doi.org/10.1111/jnc.15032
Ni J, Zhao J, Zhang X, Reinheckel T, Turk V, Nakanishi H (2021) Cathepsin H deficiency decreases hypoxia-ischemia-induced hippocampal atrophy in neonatal mice through attenuated TLR3/IFN-beta signaling. J Neuroinflammation 18(1):176. https://doi.org/10.1186/s12974-021-02227-7
Zhang X, Wu Z, Hayashi Y, Okada R, Nakanishi H (2014) Peripheral role of cathepsin S in Th1 cell-dependent transition of nerve injury-induced acute pain to a chronic pain state. J Neurosci 34(8):3013–3022. https://doi.org/10.1523/JNEUROSCI.3681-13.2014
Hamdy N, Eide S, Sun HS, Feng ZP (2020) Animal models for neonatal brain injury induced by hypoxic ischemic conditions in rodents. Exp Neurol 334:113457. https://doi.org/10.1016/j.expneurol.2020.113457
Sommer CJ (2017) Ischemic stroke: experimental models and reality. Acta Neuropathol 133(2):245–261. https://doi.org/10.1007/s00401-017-1667-0
Neher JJ, Neniskyte U, Zhao JW, Bal-Price A, Tolkovsky AM, Brown GC (2011) Inhibition of microglial phagocytosis is sufficient to prevent inflammatory neuronal death. J Immunol 186(8):4973–4983. https://doi.org/10.4049/jimmunol.1003600
Marin-Teva JL, Dusart I, Colin C, Gervais A, van Rooijen N, Mallat M (2004) Microglia promote the death of developing Purkinje cells. Neuron 41(4):535–547. https://doi.org/10.1016/s0896-6273(04)00069-8
Meng J, Ni J, Wu Z, Jiang M, Zhu A, Qing H, Nakanishi H (2018) The critical role of IL-10 in the antineuroinflammatory and antioxidative effects of Rheum tanguticum on activated microglia. Oxid Med Cell Longev 2018:1083596. https://doi.org/10.1155/2018/1083596
Antoniak S, Rojas M, Spring D, Bullard TA, Verrier ED, Blaxall BC, Mackman N, Pawlinski R (2010) Protease-activated receptor 2 deficiency reduces cardiac ischemia/reperfusion injury. Arterioscler Thromb Vasc Biol 30(11):2136–2142. https://doi.org/10.1161/ATVBAHA.110.213280
Schmidlin F, Amadesi S, Dabbagh K, Lewis DE, Knott P, Bunnett NW, Gater PR, Geppetti P et al (2002) Protease-activated receptor 2 mediates eosinophil infiltration and hyperreactivity in allergic inflammation of the airway. J Immunol 169(9):5315–5321. https://doi.org/10.4049/jimmunol.169.9.5315
Ferrell WR, Lockhart JC, Kelso EB, Dunning L, Plevin R, Meek SE, Smith AJ, Hunter GD et al (2003) Essential role for proteinase-activated receptor-2 in arthritis. J Clin Invest 111(1):35–41. https://doi.org/10.1172/JCI16913
Jahan I, Fujimoto J, Alam SM, Sato E, Tamaya T (2008) Role of protease activated receptor-2 in lymph node metastasis of uterine cervical cancers. BMC Cancer 8:301. https://doi.org/10.1186/1471-2407-8-301
Jin E, Fujiwara M, Pan X, Ghazizadeh M, Arai S, Ohaki Y, Kajiwara K, Takemura T et al (2003) Protease-activated receptor (PAR)-1 and PAR-2 participate in the cell growth of alveolar capillary endothelium in primary lung adenocarcinomas. Cancer 97(3):703–713. https://doi.org/10.1002/cncr.11087
Jahan I, Fujimoto J, Alam SM, Sato E, Sakaguchi H, Tamaya T (2007) Role of protease activated receptor-2 in tumor advancement of ovarian cancers. Ann Oncol 18(9):1506–1512. https://doi.org/10.1093/annonc/mdm190
Sachan V, Lodge R, Mihara K, Hamelin J, Power C, Gelman BB, Hollenberg MD, Cohen EA et al (2019) HIV-induced neuroinflammation: impact of PAR1 and PAR2 processing by Furin. Cell Death Differ 26(10):1942–1954. https://doi.org/10.1038/s41418-018-0264-7
Funding
This work was supported by the National Natural Science Foundation of China (32070954 and 82001167); the Beijing Natural Science Foundation (7212066); the Beijing Institute of Technology Research Fund Program (2020CX04166); and the Zhejiang Provincial Natural Science Foundation (Q20H140040).
Author information
Authors and Affiliations
Contributions
Y.L. conducted most of the experiments, analyzed the data, and wrote the manuscript. H.L. and J.H. conducted most of the experiments and analyzed the data. Z.W., J.M., Y.H., and H.N. provided valuable advice and unpublished reagents/analytic tools. H.Q. designed part of the study. J.N. designed the whole study and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yicong Liu, Hui Li, and Jiangqi Hu contributed equally to this work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, Y., Li, H., Hu, J. et al. Differential Expression and Distinct Roles of Proteinase-Activated Receptor 2 in Microglia and Neurons in Neonatal Mouse Brain After Hypoxia-Ischemic Injury. Mol Neurobiol 59, 717–730 (2022). https://doi.org/10.1007/s12035-021-02594-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-021-02594-5