Abstract
Activity-induced pain is common in those with chronic musculoskeletal pain and limits participation in daily activities and exercise. Our laboratory developed a model of activity-induced pain and shows that depletion of muscle macrophages prevents development of hyperalgesia. Adenosine triphosphate (ATP) is released from fatiguing muscle and activates purinergic receptors (P2X), and P2X4 receptors are expressed on macrophages. We hypothesized that exercise releases ATP to activate P2X4 receptors on muscle macrophages, which subsequently release interleukin-1β (IL-1β) to produce hyperalgesia. In an animal model of activity-induced pain, using male and female C57BL6/J mice, we show increased expression of P2X4 on muscle macrophages, and blockade of P2X4 receptors in muscle prevented development of hyperalgesia. Using a lentivirus expressing an artificial micro-RNA to P2X4 under the control of a CD68 promoter, we decreased expression of P2X4 mRNA in cultured macrophages, decreased expression of P2X4 protein in muscle macrophages in vivo, and prevented development of activity-induced hyperalgesia. We further show that macrophages primed with LPS differentially released IL-1β when treated with ATP in neutral or acidic pH. Lastly, blockade of IL-1β in muscle prevented development of hyperalgesia in this model. Thus, our data suggest that P2X4 receptors could be a valid pharmacological target to control activity-induced muscle pain experienced by patients with chronic musculoskeletal pain.




Similar content being viewed by others
References
Gaskin DJ, Richard P (2012) The economic costs of pain in the United States. J Pain 13(8):715–724
Palazzo C, Ravaud JF, Papelard A, Ravaud P, Poiraudeau S (2014) The burden of musculoskeletal conditions. PLoS One 9(3):e90633
Rice AS, Smith BH, Blyth FM (2016) Pain and the global burden of disease. Pain 157(4):791–796
Bidonde J, Busch AJ, Bath B, Milosavljevic S (2014) Exercise for adults with fibromyalgia: an umbrella systematic review with synthesis of best evidence. Curr Rheumatol Rev 10(1):45–79
Fransen M, McConnell S, Harmer AR, van der Esch M, Simic M, Bennell KL (2015) Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev 1:CD004376
Hoeger Bement MK, Sluka KA (2016) Exercise-induced hypoalgesia: an evidence-based review. In: Sluka KA (ed) Pain mechanisms and management for the physical therapist. Wolters Kluwer, Philadelphia, pp. 177–202
Bair MJ, Matthias MS, Nyland KA, Huffman MA, Stubbs DL, Kroenke K, Damush TM (2009) Barriers and facilitators to chronic pain self-management: a qualitative study of primary care patients with comorbid musculoskeletal pain and depression. Pain Med 10(7):1280–1290
Dailey DL, Keffala VJ, Sluka KA (2015) Do cognitive and physical fatigue tasks enhance pain, cognitive fatigue, and physical fatigue in people with fibromyalgia? Arthritis Care Res 67(2):288–296
Kadetoff D, Kosek E (2007) The effects of static muscular contraction on blood pressure, heart rate, pain ratings and pressure pain thresholds in healthy individuals and patients with fibromyalgia. Eur J Pain 11(1):39–47
Heneweer H, Staes F, Aufdemkampe G (2011) Van RM, Vanhees L. physical activity and low back pain: a systematic review of recent literature. Eur Spine J 20(6):826–845
Kop WJ, Lyden A, Berlin AA, Ambrose K, Olsen C, Gracely RH, Williams DA, Clauw DJ (2005) Ambulatory monitoring of physical activity and symptoms in fibromyalgia and chronic fatigue syndrome. Arthritis Rheum 52(1):296–303
McLoughlin MJ, Colbert LH, Stegner AJ, Cook DB (2011) Are women with fibromyalgia less physically active than healthy women? Med Sci Sports Exerc 43(5):905–912
Merriwether EN, Rakel BA, Zimmerman MB, Dailey DL, Vance CG, Darghosian L, Golchha M, Geasland KM et al (2016) Reliability and construct validity of the patient-reported outcomes measurement information system (PROMIS) instruments in women with fibromyalgia. Pain Med 18:1485–1495
Segura-Jimenez V, Borges-Cosic M, Soriano-Maldonado A, Estevez-Lopez F, Alvarez-Gallardo IC, Herrador-Colmenero M, Delgado-Fernandez M, Ruiz JR (2017) Association of sedentary time and physical activity with pain, fatigue, and impact of fibromyalgia: the al-Andalus study. Scand J Med Sci Sports 27(1):83–92
Li J, King NC, Sinoway LI (2003) ATP concentrations and muscle tension increase linearly with muscle contraction. J Appl Physiol 95(2):577–583
Pollak KA, Swenson JD, Vanhaitsma TA, Hughen RW, Jo D, Light KC, Schweinhardt P, Amann M et al (2014) Exogenously applied muscle metabolites synergistically evoke sensations of muscle fatigue and pain in human subjects. Exp Physiol 99(2):368–380
Sahlin K, Harris RC, Nylind B, Hultman E (1976) Lactate content and pH in muscle obtained after dynamic exercise. Pflugers Arch 367(2):143–149
Spriet LL, Soderlund K, Thomson JA, Hultman E (1985) pH measurement in human skeletal muscle samples: effect of phosphagen hydrolysis. J Appl Physiol 1986;61(5):1949–1954
Birdsong WT, Fierro L, Williams FG, Spelta V, Naves LA, Knowles M, Marsh-Haffner J, Adelman JP et al (2010) Sensing muscle ischemia: coincident detection of acid and ATP via interplay of two ion channels. Neuron 68(4):739–749
Gregory NS, Whitley PE, Sluka KA (2015) Effect of intramuscular protons, lactate, and ATP on muscle hyperalgesia in rats. PLoS One 10(9):e0138576
Immke DC, McCleskey EW (2001) Lactate enhances the acid-sensing Na+ channel on ischemia-sensing neurons. Nat Neurosci 4(9):869–870
Light AR, Hughen RW, Zhang J, Rainier J, Liu Z, Lee J (2008) Dorsal root ganglion neurons innervating skeletal muscle respond to physiological combinations of protons, ATP, and lactate mediated by ASIC, P2X, and TRPV1. J Neurophysiol 100(3):1184–1201
McGaraughty S, Wismer CT, Zhu CZ, Mikusa J, Honore P, Chu KL, Lee CH, Faltynek CR et al (2003) Effects of A-317491, a novel and selective P2X3/P2X2/3 receptor antagonist, on neuropathic, inflammatory and chemogenic nociception following intrathecal and intraplantar administration. Br J Pharmacol 140(8):1381–1388
Oliveira MC, Pelegrini-da-Silva A, Tambeli CH, Parada CA (2009) Peripheral mechanisms underlying the essential role of P2X3,2/3 receptors in the development of inflammatory hyperalgesia. Pain 141(1–2):127–134
Teixeira JM, Bobinski F, Parada CA, Sluka KA, Tambeli CH (2017) P2X3 and P2X2/3 receptors play a crucial role in articular hyperalgesia development through inflammatory mechanisms in the knee joint experimental Synovitis. Mol Neurobiol 54(8):6174–6186
Ulmann L, Hirbec H, Rassendren F (2010) P2X4 receptors mediate PGE2 release by tissue-resident macrophages and initiate inflammatory pain. EMBO J 29(14):2290–2300
Light AR, White AT, Hughen RW, Light KC (2009) Moderate exercise increases expression for sensory, adrenergic, and immune genes in chronic fatigue syndrome patients but not in normal subjects. J Pain 10(10):1099–1112
Tsuda M, Kuboyama K, Inoue T, Nagata K, Tozaki-Saitoh H, Inoue K (2009) Behavioral phenotypes of mice lacking purinergic P2X4 receptors in acute and chronic pain assays. Mol Pain 5:28
Wang L, Jacobsen SE, Bengtsson A, Erlinge D (2004) P2 receptor mRNA expression profiles in human lymphocytes, monocytes and CD34+ stem and progenitor cells. BMC Immunol 5:16
Gregory NS, Brito R, Fusaro MCGO, Sluka KA (2016) ASIC3 is required for development of fatigue-induced hyperalgesia. Mol Neurobiol 53:1020–1030
Dina OA, Green PG, Levine JD (2008) Role of interleukin-6 in chronic muscle hyperalgesic priming. Neuroscience 152(2):521–525
Gong WY, Abdelhamid RE, Carvalho CS, Sluka KA (2016) Resident macrophages in muscle contribute to development of hyperalgesia in a mouse model of non-inflammatory muscle pain. J Pain 17:1081–1094
Schaible HG, Von Banchet GS, Boettger MK, Brauer R, Gajda M, Richter F, Hensellek S, Brenn D et al (2010) The role of proinflammatory cytokines in the generation and maintenance of joint pain. Ann N Y Acad Sci 1193:60–69
Watkins LR, Maier SF, Goehler LE (1995) Immune activation: the role of pro-inflammatory cytokines in inflammation, illness responses and pathological pain states. Pain 63(3):289–302
Pelegrin P, Barroso-Gutierrez C, Surprenant A (2008) P2X7 receptor differentially couples to distinct release pathways for IL-1beta in mouse macrophage. J Immunol 180(11):7147–7157
Ferron M, Vacher J (2005) Targeted expression of Cre recombinase in macrophages and osteoclasts in transgenic mice. Genesis 41(3):138–145
Patsouris D, Li PP, Thapar D, Chapman J, Olefsky JM, Neels JG (2008) Ablation of CD11c-positive cells normalizes insulin sensitivity in obese insulin resistant animals. Cell Metab 8(4):301–309
Osten P, Dittgen T, Licznerski P (2006) Lentivirus-based genetic manipulation in neurons in vivo. In: Kittler JT, Moss SJ (eds) The dynamic synapse: molecular methods in Ionotropic receptor biology. CRC Press, Boca Raton
Gregory NS, Gibson-Corley K, Frey-Law L, Sluka KA (2013) Fatigue-enhanced hyperalgesia in response to muscle insult: induction and development occur in a sex-dependent manner. Pain 154:2668–2676
Sluka KA, Kalra A, Moore SA (2001) Unilateral intramuscular injections of acidic saline produce a bilateral, long-lasting hyperalgesia. Muscle Nerve 24:37–46
Yokoyama T, Lisi TL, Moore SA, Sluka KA (2007) Muscle fatigue increases the probability of developing hyperalgesia in mice. J Pain 8:692–699
Skyba DA, Radhakrishnan R, Sluka KA (2005) Characterization of a method for measuring primary hyperalgesia of deep somatic tissue. J Pain 6(1):41–47
Balazs B, Danko T, Kovacs G, Koles L, Hediger MA, Zsembery A (2013) Investigation of the inhibitory effects of the benzodiazepine derivative, 5-BDBD on P2X4 purinergic receptors by two complementary methods. Cell Physiol Biochem 32(1):11–24
Coddou C, Sandoval R, Hevia MJ, Stojilkovic SS (2019) Characterization of the antagonist actions of 5-BDBD at the rat P2X4 receptor. Neurosci Lett 690:219–224
Mosser DM, Edwards JP (2008) Exploring the full spectrum of macrophage activation. Nat Rev Immunol 8(12):958–969
Ghasemlou N, Chiu IM, Julien JP, Woolf CJ (2015) CD11b+Ly6G- myeloid cells mediate mechanical inflammatory pain hypersensitivity. Proc Natl Acad Sci U S A 112(49):E6808–E6817
Shepherd AJ, Mickle AD, Golden JP, Mack MR, Halabi CM, de Kloet AD, Samineni VK, Kim BS et al (2018) Macrophage angiotensin II type 2 receptor triggers neuropathic pain. Proc Natl Acad Sci U S A 115(34):E8057–E8066
Willemen HL, Eijkelkamp N, Garza CA, Wang H, Mack M, Zijlstra J, Heijnen CJ, Kavelaars A (2014) Monocytes/macrophages control resolution of transient inflammatory pain. J Pain 15(5):496–506
Shepherd AJ, Copits BA, Mickle AD, Karlsson P, Kadunganattil S, Haroutounian S, Tadinada SM, de Kloet AD et al (2018) Angiotensin II triggers peripheral macrophage-to-sensory neuron redox crosstalk to elicit pain. J Neurosci 38(32):7032–7057
da Silva MD, Bobinski F, Sato KL, Kolker SJ, Sluka KA, Santos AR (2015) IL-10 cytokine released from M2 macrophages is crucial for analgesic and anti-inflammatory effects of acupuncture in a model of inflammatory muscle pain. Mol Neurobiol 51:19–31
Mueller M, Leonhard C, Wacker K, Ringelstein EB, Okabe M, Hickey WF, Kiefer R (2003) Macrophage response to peripheral nerve injury: the quantitative contribution of resident and hematogenous macrophages. Lab Investig 83(2):175–185
Mueller M, Wacker K, Ringelstein EB, Hickey WF, Imai Y, Kiefer R (2001) Rapid response of identified resident endoneurial macrophages to nerve injury. Am J Pathol 159(6):2187–2197
Muller M, Wacker K, Getts D, Ringelstein EB, Kiefer R (2008) Further evidence for a crucial role of resident endoneurial macrophages in peripheral nerve disorders: lessons from acrylamide-induced neuropathy. Glia 56(9):1005–1016
Bangsbo J, Krustrup P, Gonzalez-Alonso J, Saltin B (2001) ATP production and efficiency of human skeletal muscle during intense exercise: effect of previous exercise. Am J Physiol Endocrinol Metab 280(6):E956–E964
Hood VL, Chubert C, Keller U, Muller S (1988) Effect of systemic pH on pHi and lactic acid generation in exhaustive forearm exercise. Am J Phys 255:F479–F485
Naves LA, McCleskey EW (2005) An acid-sensing ion channel that detects ischemic pain. Braz J Med Biol Res 38(11):1561–1569
Yagi J, Wenk HN, Naves LA, McCleskey EW (2006) Sustained currents through ASIC3 ion channels at the modest pH changes that occur during myocardial ischemia. Circ Res 99(5):501–509
North RA (2002) Molecular physiology of P2X receptors. Physiol Rev 82(4):1013–1067
Stojilkovic SS, Tomic M, He ML, Yan Z, Koshimizu TA, Zemkova H (2005) Molecular dissection of purinergic P2X receptor channels. Ann N Y Acad Sci 1048:116–130
Niemand C, Nimmesgern A, Haan S, Fischer P, Schaper F, Rossaint R, Heinrich PC, Muller-Newen G (2003) Activation of STAT3 by IL-6 and IL-10 in primary human macrophages is differentially modulated by suppressor of cytokine signaling 3. J Immunol 170(6):3263–3272
Valentine RJ, Jefferson MA, Kohut ML (2018) Eo H. Imoxin attenuates LPS-induced inflammation and MuRF1 expression in mouse skeletal muscle. Phys Rep:6(23)
Borghi SM, Zarpelon AC, Pinho-Ribeiro FA, Cardoso RD, Cunha TM, Alves-Filho JC, Ferreira SH, Cunha FQ et al (2014) Targeting interleukin-1beta reduces intense acute swimming-induced muscle mechanical hyperalgesia in mice. J Pharm Pharmacol 66(7):1009–1020
Ferreira SH, Lorenzetti BB, Bristow AF, Poole S (1988) Interleukin-1 beta as a potent hyperalgesic agent antagonized by a tripeptide analogue. Nature 334(6184):698–700
Fukuoka H, Kawatani M, Hisamitsu T, Takeshige C (1994) Cutaneous hyperalgesia induced by peripheral injection of interleukin-1 beta in the rat. Brain Res 657(1–2):133–140
Cunha JM, Cunha FQ, Poole S, Ferreira SH (2000) Cytokine-mediated inflammatory hyperalgesia limited by interleukin-1 receptor antagonist. Br J Pharmacol 130(6):1418–1424
Safieh-Garabedian B, Poole S, Allchorne A, Winter J, Woolf CJ (1995) Contribution of interleukin-1 beta to the inflammation-induced increase in nerve growth factor levels and inflammatory hyperalgesia. Br J Pharmacol 115(7):1265–1275
Perez-Flores G, Levesque SA, Pacheco J, Vaca L, Lacroix S, Perez-Cornejo P, Arreola J (2015) The P2X7/P2X4 interaction shapes the purinergic response in murine macrophages. Biochem Biophys Res Commun 467(3):484–490
Kobayashi K, Fukuoka T, Yamanaka H, Dai Y, Obata K, Tokunaga A, Noguchi K (2005) Differential expression patterns of mRNAs for P2X receptor subunits in neurochemically characterized dorsal root ganglion neurons in the rat. J Comp Neurol 481(4):377–390
Mapplebeck JCS, Dalgarno R, Tu Y, Moriarty O, Beggs S, Kwok CHT, Halievski K, Assi S et al (2018) Microglial P2X4R-evoked pain hypersensitivity is sexually dimorphic in rats. Pain 159(9):1752–1763
Sorge RE, Mapplebeck JC, Rosen S, Beggs S, Taves S, Alexander JK, Martin LJ, Austin JS et al (2015) Different immune cells mediate mechanical pain hypersensitivity in male and female mice. Nat Neurosci 18(8):1081–1083
Gregory NS, Gautam M, Benson CJ, Sluka KA (2018) Acid sensing Ion Channel 1a (ASIC1a) mediates activity-induced pain by modulation of Heteromeric ASIC Channel kinetics. Neuroscience 386:166–174
Huang P, Zou Y, Zhong XZ, Cao Q, Zhao K, Zhu MX, Murrell-Lagnado R, Dong XP (2014) P2X4 forms functional ATP-activated cation channels on lysosomal membranes regulated by luminal pH. J Biol Chem 289(25):17658–17667
Murrell-Lagnado RD (2018) A role for P2X4 receptors in lysosome function. J Gen Physiol 150(2):185–187
Rajamaki K, Nordstrom T, Nurmi K, Akerman KE, Kovanen PT, Oorni K, Eklund KK (2013) Extracellular acidosis is a novel danger signal alerting innate immunity via the NLRP3 inflammasome. J Biol Chem 288(19):13410–13419
Kosek E, Ekholm J, Hansson P (1996) Modulation of pressure pain thresholds during and following isometric contraction in patients with fibromyalgia and in healthy controls. Pain 64:415–423
Light AR, Bateman L, Jo D, Hughen RW, Vanhaitsma TA, White AT, Light KC (2012) Gene expression alterations at baseline and following moderate exercise in patients with chronic fatigue syndrome and fibromyalgia syndrome. J Intern Med 271(1):64–81
Acknowledgments
The authors would like to thank Dr. Steven P. Wilson, Professor Emeritus, University of South Carolina, for help with design, development, and writing of methods for using of the lentiviral vector.
Funding
This study was supported by the National Institute of Arthritis, Musculoskeletal and Skin Diseases (NIAMS) AR061371 and AR073187, the Carver College of Medicine at the University of Iowa, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001, and the Sao Paulo Research Foundation (FAPESP) [grant number 2014/01119-4].
Author information
Authors and Affiliations
Contributions
Maria Claudia Oliveira-Fusaro designed the project, performed and analyzed behavioral experiments and some of immunofluorescence assays, collected tissue samples, wrote the manuscript; Nicholas S. Gregory provided support during fatigue experiments, collected tissue samples, designed lentivirus; Lynn Rasmussen provided support during behavioral experiments, performed and analyzed some of immunofluorescence assays; Sandra J. Kolker performed all experiments and analysis using cultured macrophages and images from some immunofluorescence assays; Lee-Ann H. Allen provided training and support for cytokine assays from cultured macrophages, design, and revised the manuscript, Kathleen A. Sluka conceived the study, was in charge of overall direction and planning, analyzed all final data, wrote and revised the manuscript. All authors provided critical feedback and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Fig1
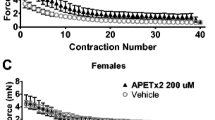
Behavioral data analyzed for sex differences. a,b. Scatter plots with mean ± S.E.M. showing withdrawal thresholds of the ipsilateral (a) and contralateral (b) muscle 24h after induction of the model for male (blue) and female (red) mice treated with vehicle or 5, 50, or 500μM 5-BDBD on Day 5 prior to the fatiguing contraction and second intramuscular saline injection. For comparison withdrawal threshold from the vehicle treated mouse prior to induction of the model are shown (gray, N). +, p<0.05 compared to vehicle. c.d. Scatter plots mean ± S.E.M. showing withdrawal thresholds of the ipsilateral (c) and contralateral (d) muscle 24h after induction of the model for male (blue) and female (red) mice treated with vehicle or 500μM 5-BDBD prior to the 1st intramuscular saline injection. For comparison withdrawal threshold from the vehicle treated mouse prior to induction of the model are shown (gray, N). +, p<0.05 compared to vehicle. e,f. Scatter plots mean+S.E.M. showing withdrawal thresholds of the ipsilateral (e) and contralateral (f) muscle 24h after induction of the model for male (blue) and female (red) mice treated with a lentivirus expressing a control miRNA (miR_C) or an artificial miRNA to P2X4 (miR_P2X4) prior to the 1st intramuscular saline injection. For comparison withdrawal threshold from the vehicle treated mouse prior to induction of the model are shown (gray, N). +, p<0.05 compared to vehicle. Data are represented as the mean and SEM. (JPG 58 kb)
Supplementary Fig2
Effects of ATP, pH and LPS on release of cytokines from cultured macrophages. Scatter plots with mean and SEM for GM-CSF (a), IL-5 (b), IL-4 (c), IFNγ (d), IL-10 (e), and TNFα (f) released from cultured peritoneal macrophages treated different combinations of LPS, ATP or acidic pH. ATP evoked release of GM-CSF with or without acidic pH, LPS evoked release of IL-5 and IL-4 regardless of treatment with ATP or pH, and there were no consistent changes in IFNγ, IL-10 or TNFα. * P<0.05 compared to LPS-/ATP-/pH7.4 condition. (JPG 90 kb)
Rights and permissions
About this article
Cite this article
Oliveira-Fusaro, M.C., Gregory, N.S., Kolker, S.J. et al. P2X4 Receptors on Muscle Macrophages Are Required for Development of Hyperalgesia in an Animal Model of Activity-Induced Muscle Pain. Mol Neurobiol 57, 1917–1929 (2020). https://doi.org/10.1007/s12035-019-01852-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-019-01852-x