Abstract
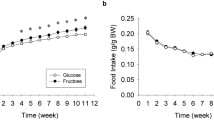
Excessive sugar intake has been related to cognitive alterations, but it remains unclear whether these effects are related exclusively to increased energy intake, and the molecular mechanisms involved are not fully understood. We supplemented Sprague-Dawley female rats with 10% w/v fructose in drinking water or with isocaloric glucose solution for 7 months. Cognitive function was assessed through the Morris water maze (MWM) and the novel object recognition (NOR) tests. Plasma parameters and protein/mRNA expression in the frontal cortex and hippocampus were determined. Results showed that only fructose-supplemented rats displayed postprandial and fasting hypertriglyceridemia (1.4 and 1.9-fold, p < 0.05) and a significant reduction in the discrimination index in the NOR test, whereas the results of the MWM test showed no differences between groups. Fructose-drinking rats displayed an abnormal glucose tolerance test and impaired insulin signaling in the frontal cortex, as revealed by significant reductions in insulin receptor substrate-2 protein levels (0.77-fold, p < 0.05) and Akt phosphorylation (0.72-fold, p < 0.05), and increased insulin-degrading enzyme levels (1.86-fold, p < 0.001). Fructose supplementation reduced the expression of antioxidant enzymes and altered the amount of proteins involved in mitochondrial fusion/fission in the frontal cortex. In conclusion, cognitive deficits induced by chronic liquid fructose consumption are not exclusively related to increased caloric intake and are correlated with hypertriglyceridemia, impaired insulin signaling, increased oxidative stress and altered mitochondrial dynamics, especially in the frontal cortex.








Similar content being viewed by others
References
de la Monte SM, Longato L, Tong M, Wands JR (2009) Insulin resistance and neurodegeneration: roles of obesity, type 2 diabetes mellitus and non-alcoholic steatohepatitis. Curr Opin Investig Drugs 10(10):1049–1060. https://doi.org/10.1016/j.ygyno.2014.12.035.Pharmacologic
Biessels GJ, Reagan LP (2015) Hippocampal insulin resistance and cognitive dysfunction. Nat Rev Neurosci 16(11):660–671. https://doi.org/10.1038/nrn4019
Dekker MJ, Su Q, Baker C, Rutledge AC, Adeli K (2010) Fructose: a highly lipogenic nutrient implicated in insulin resistance, hepatic steatosis, and the metabolic syndrome. Am J Physiol Endocrinol Metab 299(5):E685–E694. https://doi.org/10.1152/ajpendo.00283.2010
Tappy L, Lê KA, Tran C, Paquot N (2010) Fructose and metabolic diseases: new findings, new questions. Nutrition 26(11-12):1044–1049. https://doi.org/10.1016/j.nut.2010.02.014
Stanhope KL, Havel PJ (2008) Endocrine and metabolic effects of consuming beverages sweetened with fructose, glucose, sucrose, or high fructose corn syrup. Am J Clin Nutr 88(6):1733S–1737S. https://doi.org/10.3945/ajcn.2008.25825D.Endocrine
Campos VC, Tappy L (2016) Physiological handling of dietary fructose-containing sugars: implications for health. Int J Obes 40(S1):S6–S11. https://doi.org/10.1038/ijo.2016.8
Lakhan S, Kirchgessner A (2013) The emerging role of dietary fructose in obesity and cognitive decline. Nutr J 12(1):1–12. https://doi.org/10.1186/1475-2891-12-114
Beilharz JE, Maniam J, Morris MJ (2015) Diet-induced cognitive deficits: the role of fat and sugar, potential mechanisms and nutritional interventions. Nutrients 7(8):6719–6738. https://doi.org/10.3390/nu7085307
Lowette K, Roosen L, Tack J, Van den Berghe P (2015) Effects of high-fructose diets on central appetite signaling and cognitive function. Front Nutr 2:5. https://doi.org/10.3389/fnut.2015.00005
Popkin BM, Hawkes C (2016) Sweetening of the global diet, particularly beverages: patterns, trends, and policy responses. Lancet Diabetes Endocrinol 4(2):174–186. https://doi.org/10.1016/S2213-8587(15)00419-2
Stanhope KL, Schwarz JM, Keim NL et al (2009) Consuming fructose-sweetened, not glucose-sweetened, beverages increase visceral adiposity and lipids and decrease insulin sensitivity in overweight/obese men. J Clin Invest 1334:1322–1334. https://doi.org/10.1172/JCI37385DS1
Schaefer EJ, Gleason JA, Dansinger ML (2009) Dietary fructose and glucose differentially affect lipid and glucose homeostasis1–3. J Nutr 139(6):1257S–1262S. https://doi.org/10.3945/jn.108.098186
Baena M, Sangüesa G, Dávalos A, Latasa MJ, Sala-Vila A, Sánchez RM, Roglans N, Laguna JC et al (2016) Fructose, but not glucose, impairs insulin signaling in the three major insulin-sensitive tissues. Sci Rep 6(1):26149. https://doi.org/10.1038/srep26149
Sangüesa G, Shaligram S, Akhter F et al (2017) Type of supplemented simple sugar, not merely calorie intake, determines adverse effects on metabolism and aortic function in female rats. Am J Physiol Heart Circ Physiol 312(2):H289–H304. https://doi.org/10.1152/ajpheart.00339.2016
Geda YE, Ragossnig M, Roberts LA, Roberts RO, Pankratz VS, Christianson TJ, Mielke MM, Levine JA et al (2013) Caloric intake, aging, and mild cognitive impairment: a population-based study. J Alzheimers Dis 34(2):501–507. https://doi.org/10.3233/JAD-121270
Roberts RO, Roberts LA, Geda YE, Cha RH, Pankratz VS, O'Connor HM, Knopman DS, Petersen RC (2012) Relative intake of macronutrients impacts risk of mild cognitive impairment or dementia. J Alzheimers Dis 32(2):329–339. https://doi.org/10.3233/JAD-2012-120862
Vilà L, Roglans N, Perna V, Sánchez RM, Vázquez-Carrera M, Alegret M, Laguna JC (2011) Liver AMP/ATP ratio and fructokinase expression are related to gender differences in AMPK activity and glucose intolerance in rats ingesting liquid fructose. J Nutr Biochem 22(8):741–751. https://doi.org/10.1016/j.jnutbio.2010.06.005
Sengupta P (2013) The laboratory rat: relating age with human’s. Int J Prev Med 4(6):624–630
Helenius M, Hänninen M, Lehtinen SK, Salminen A (1996) Aging-induced up-regulation of nuclear binding activities of oxidative stress responsive NF-kB transcription factor in mouse cardiac muscle. J Mol Cell Cardiol 28(3):487–498. https://doi.org/10.1006/jmcc.1996.0045
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72(1-2):248–254. https://doi.org/10.1016/0003-2697(76)90527-3
Roglans N, Vilà L, Farré M, Alegret M, Sánchez RM, Vázquez-Carrera M, Laguna JC (2007) Impairment of hepatic Stat-3 activation and reduction of PPARalpha activity in fructose-fed rats. Hepatology 45(3):778–788. https://doi.org/10.1002/hep.21499
Bedse G, Di Domenico F, Serviddio G, Cassano T (2015) Aberrant insulin signaling in Alzheimer’s disease: current knowledge. Front Neurosci 9:1–13. https://doi.org/10.3389/fnins.2015.00204
Benton D, Maconie A, Williams C (2007) The influence of the glycaemic load of breakfast on the behaviour of children in school. Physiol Behav 92(4):717–724. https://doi.org/10.1016/j.physbeh.2007.05.065
Nabb S, Benton D (2006) The influence on cognition of the interaction between the macro-nutrient content of breakfast and glucose tolerance. Physiol Behav 87(1):16–23. https://doi.org/10.1016/j.physbeh.2005.08.034
Smith MA, Foster JK (2008) The impact of a high versus a low glycaemic index breakfast cereal meal on verbal episodic memory in healthy adolescents. Nutr Neurosci 11(5):219–227. https://doi.org/10.1179/147683008X344110
Messier C (2004) Glucose improvement of memory: a review. Eur J Pharmacol 490(1-3):33–57. https://doi.org/10.1016/j.ejphar.2004.02.043
Stollery B, Christian L (2016) Glucose improves object-location binding in visual-spatial working memory. Psychopharmacology 233(3):529–547. https://doi.org/10.1007/s00213-015-4125-5
Kanoski SE, Davidson TL (2011) Western diet consumption and cognitive impairment: Links to hippocampal dysfunction and obesity. Physiol Behav 103(1):59–68. https://doi.org/10.1016/j.physbeh.2010.12.003
Antunes M, Biala G (2012) The novel object recognition memory: neurobiology, test procedure, and its modifications. Cogn Process 13(2):93–110. https://doi.org/10.1007/s10339-011-0430-z
Sharma S, Rakoczy S, Brown-Borg H (2010) Assessment of spatial memory in mice. Life Sci 87(17-18):521–536. https://doi.org/10.1016/j.lfs.2010.09.004
Francis BM, Kim J, Barakat ME, Fraenkl S, Yücel YH, Peng S, Michalski B, Fahnestock M et al (2012) Object recognition memory and BDNF expression are reduced in young TgCRND8 mice. Neurobiol Aging 33(3):555–563. https://doi.org/10.1016/j.neurobiolaging.2010.04.003
Brown MW, Barker GRI, Aggleton JP, Warburton EC (2012) What pharmacological interventions indicate concerning the role of the perirhinal cortex in recognition memory. Neuropsychologia 50(13):3122–3140. https://doi.org/10.1016/j.neuropsychologia.2012.07.034
Ross AP, Bartness TJ, Mielke JG, Parent MB (2009) A high fructose diet impairs spatial memory in male rats. Neurobiol Learn Mem 92(3):410–416. https://doi.org/10.1016/j.nlm.2009.05.007
Yin QQ, Pei JJ, Xu S, Luo DZ, Dong SQ, Sun MH, You L, Sun ZJ et al (2013) Pioglitazone improves cognitive function via increasing insulin sensitivity and strengthening antioxidant defense system in fructose-drinking insulin resistance rats. PLoS One 8(3):e59313. https://doi.org/10.1371/journal.pone.0059313
Bruggeman EC, Li C, Ross AP, Doherty JM, Williams BF, Frantz KJ, Parent MB (2011) A high fructose diet does not affect amphetamine self-administration or spatial water maze learning and memory in female rats. Pharmacol Biochem Behav 99(3):356–364. https://doi.org/10.1016/j.pbb.2011.05.014
Abbott KN, Morris MJ, Westbrook RF, Reichelt AC (2016) Sex-specific effects of daily exposure to sucrose on spatial memory performance in male and female rats, and implications for estrous cycle stage. Physiol Behav 162:52–60. https://doi.org/10.1016/j.physbeh.2016.01.036
Stranahan AM, Norman ED, Lee K, Cutler RG, Telljohann RS, Egan JM, Mattson MP (2008) Diet-induced insulin resistance impairs hippocampal synaptic plasticity and cognition in middle-aged rats. Hippocampus 18(11):1085–1088. https://doi.org/10.1002/hipo.20470
Molteni R, Barnard RJ, Ying Z, Roberts CK, Gómez-Pinilla F (2002) A high-fat, refined sugar diet reduces hippocampal brain-derived neurotrophic factor, neuronal plasticity, and learning. Neuroscience 112(4):803–814. https://doi.org/10.1016/S0306-4522(02)00123-9
Drew P, Smith E, Thomas P (1998) Fat distribution and changes in the blood brain barrier in a rat model of cerebral arterial fat embolism. J Neurol Sci 156(2):138–143. https://doi.org/10.1016/S0022-510X(98)00039-2
Farr SA, Yamada KA, Butterfield DA, Abdul HM, Xu L, Miller NE, Banks WA, Morley JE (2008) Obesity and hypertriglyceridemia produce cognitive impairment. Endocrinology 149(5):2628–2636. https://doi.org/10.1210/en.2007-1722
Agrawal R, Gomez-Pinilla F (2012) “Metabolic syndrome” in the brain: deficiency in omega-3 fatty acid exacerbates dysfunctions in insulin receptor signalling and cognition. J Physiol 590(10):2485–2499. https://doi.org/10.1113/jphysiol.2012.230078
Lewis GF, Carpentier A, Adeli K, Giacca A (2002) Disordered fat storage and mobilization in the pathogenesis of insulin resistance and type 2 diabetes. Endocr Rev 23(2):201–229. https://doi.org/10.1210/edrv.23.2.0461
Yarchoan M, Arnold SE (2014) Repurposing diabetes drugs for brain insulin resistance in Alzheimer disease. Diabetes 63(7):2253–2261. https://doi.org/10.2337/db14-0287
Mielke JG, Taghibiglou C, Liu L, Zhang Y, Jia Z, Adeli K, Wang YT (2005) A biochemical and functional characterization of diet-induced brain insulin resistance. J Neurochem 93(6):1568–1578. https://doi.org/10.1111/j.1471-4159.2005.03155.x
Cigliano L, Spagnuolo MS, Crescenzo R, Cancelliere R, Iannotta L, Mazzoli A, Liverini G, Iossa S (2017) Short-term fructose feeding induces inflammation and oxidative stress in the hippocampus of young and adult rats. Mol Neurobiol. https://doi.org/10.1007/s12035-017-0518-2
McNay EC, Recknagel AK (2011) Brain insulin signaling: a key component of cognitive processes and a potential basis for cognitive impairment in type 2 diabetes. Neurobiol Learn Mem 96(4):517–528. https://doi.org/10.1016/j.nlm.2011.11.001
Monti JM, Moulton CJ, Cohen NJ (2015) The role of nutrition on cognition and brain health in ageing: a targeted approach. Nutr Res Rev 28(02):167–180. https://doi.org/10.1017/S0954422415000141
Kleinridders A, Ferris HA, Cai W, Kahn CR (2014) Insulin action in brain regulates systemic metabolism and brain function. Diabetes 63(7):2232–2243. https://doi.org/10.2337/db14-0568
Ho L, Qin W, Pompl PN et al (2004) Diet-induced insulin resistance promotes amyloidosis in a transgenic mouse model of Alzheimer’s disease. FASEB J 18:902–904. https://doi.org/10.1096/fj.03-0978fje
Zhao L (2004) Insulin-degrading enzyme as a downstream target of insulin receptor signaling cascade: implications for Alzheimer’s disease intervention. J Neurosci 24(49):11120–11126. https://doi.org/10.1523/JNEUROSCI.2860-04.2004
Di Luccia B, Crescenzo R, Mazzoli A, Cigliano L, Venditti P, Walser JC, Widmer A, Baccigalupi L et al (2015) Rescue of fructose-induced metabolic syndrome by antibiotics or faecal transplantation in a rat model of obesity. PLoS One 10(8):1–19. https://doi.org/10.1371/journal.pone.0134893
Sangüesa G, Baena M, Hutter N, Montañés J, Sánchez R, Roglans N, Laguna J, Alegret M (2017) The addition of liquid fructose to a western-type diet in LDL-R-/- mice induces liver inflammation and fibrogenesis markers without disrupting insulin receptor signalling after an insulin challenge. Nutrients 9(3):1–15. https://doi.org/10.3390/nu9030278
Abbasi A, de Paula Vieira R, Bischof F, Walter M, Movassaghi M, Berchtold NC, Niess AM, Cotman CW et al (2016) Sex-specific variation in signaling pathways and gene expression patterns in human leukocytes in response to endotoxin and exercise. J Neuroinflammation 13(1):289. https://doi.org/10.1186/s12974-016-0758-5
Nowotny K, Jung T, Höhn A, Weber D, Grune T (2015) Advanced glycation end products and oxidative stress in type 2 diabetes mellitus. Biomol Ther 5(1):194–222. https://doi.org/10.3390/biom5010194
Guimarães ELM, Empsen C, Geerts A, van Grunsven LA (2010) Advanced glycation end products induce production of reactive oxygen species via the activation of NADPH oxidase in murine hepatic stellate cells. J Hepatol 52(3):389–397. https://doi.org/10.1016/j.jhep.2009.12.007
Bierhaus A, Humpert PM, Morcos M, Wendt T, Chavakis T, Arnold B, Stern DM, Nawroth PP (2005) Understanding RAGE, the receptor for advanced glycation end products. J Mol Med 83(11):876–886. https://doi.org/10.1007/s00109-005-0688-7
Chang Y, Chang W, Tsai N et al (2014) The roles of biomarkers of oxidative stress and antioxidant in Alzheimer’s disease: a systematic review. Biomed Res Int 2014:182303
Gugliucci A (2017) Formation of fructose-mediated advanced glycation end products and their roles in metabolic and in flammatory diseases. 54–62. https://doi.org/10.3945/an.116.013912.54
Trevisan M, Browne R, Ram M, Muti P, Freudenheim J, Carosella AM, Armstrong D (2001) Correlates of markers of oxidative status in the general population. Am J Epidemiol 154(4):348–356. https://doi.org/10.1093/aje/154.4.348
Seo AY, Joseph A-MM, Dutta D et al (2010) New insights into the role of mitochondria in aging: mitochondrial dynamics and more. J Cell Sci 123(15):2533–2542. https://doi.org/10.1242/jcs.070490
Itoh K, Nakamura K, Iijima M, Sesaki H (2013) Mitochondrial dynamics in neurodegeneration. Trends Cell Biol 23(2):64–71. https://doi.org/10.1016/j.tcb.2012.10.006
Reddy PH (2014) Inhibitors of mitochondrial fission as a therapeutic strategy for diseases with oxidative stress and mitochondrial dysfunction. J Alzheimers Dis 40(2):245–256. https://doi.org/10.3233/JAD-132060
Edwards JL, Quattrini A, Lentz SI, Figueroa-Romero C, Cerri F, Backus C, Hong Y, Feldman EL (2010) Diabetes regulates mitochondrial biogenesis and fission in mouse neurons. Diabetologia 53(1):160–169. https://doi.org/10.1007/s00125-009-1553-y
Acknowledgements
We are a Consolidated Research Group of the Autonomous Government of Catalonia (SGR13-00066). We would like to thank the University of Barcelona’s Language Advisory Service for revising the manuscript.
Funding
This study was supported by the Fundació Privada Catalana de Nutrició i Lípids, Ministry of Economy and Competitiveness (grant number SAF2013-42982-R) and European Commission FEDER funds. Miguel Baena and Gemma Sangüesa were supported by FPI and FPU grants from the Spanish Ministry of Science and Innovation.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Supplemental Table 1
(DOCX 21 kb)
Supplemental Table 2
(DOCX 20 kb)
Rights and permissions
About this article
Cite this article
Sangüesa, G., Cascales, M., Griñán, C. et al. Impairment of Novel Object Recognition Memory and Brain Insulin Signaling in Fructose- but Not Glucose-Drinking Female Rats. Mol Neurobiol 55, 6984–6999 (2018). https://doi.org/10.1007/s12035-017-0863-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-017-0863-1