Abstract
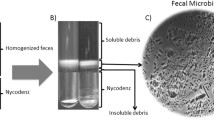
Fecal microbiota transplantation is an emerging disease-modifying therapy. The viability of the microbiome in feces and its successful transfer depends on the preparation of fecal microbiota suspension. However, currently, no standard operation procedure is proposed for fecal suspension preparation. This study aims to compare the effect of different preparation methods on the composition of fecal microbiota composition in the rat. Four methods were used to collect the fecal suspension from fresh rat fecal (Group A), including stirring with normal saline (Group B), stirring with normal saline and then standing (Group C), stirring with normal saline and filtered with gauze (Group D), and stirring with normal saline and centrifuged (Group E). 16S ribosomal RNA gene (16S rDNA) sequencing technology was used to analyze the microbiota diversity and composition of each group of samples. Compared with fresh feces, the bacterial richness of the fecal suspension obtained by the four methods was significantly decreased (P < 0.05). The structural similarity with fresh fecal microbiota from high to low is groups B, D, C, and E. All four methods changed the microbiota structure to varying degrees, thus may affect the effect of FMT. In conclusion, choosing different methods to prepare fecal suspensions may help to better optimize the application of FMT.






Similar content being viewed by others
Data Availability
The data generated in the study have been uploaded to the NCBI Sequence Read Archive (SRA) under accession PRJNA827478. Now the data are available for reviewers (https://dataview.ncbi.nlm.nih.gov/object/PRJNA827478?reviewer=lqau50mvmdm0jilpgasc99ln3r).
References
Martin, R., Miquel, S., Langella, P., & Bermudez-Humaran, L. G. (2014). The role of metagenomics in understanding the human microbiome in health and disease. Virulence, 5, 413–423.
Fehily, S. R., Basnayake, C., Wright, E. K., & Kamm, M. A. (2021). Fecal microbiota transplantation therapy in Crohn’s disease: Systematic review. Journal of Gastroenterology and Hepatology, 36, 2672–2686.
Aira, A., Rubio, E., Vergara Gomez, A., Feher, C., Casals-Pascual, C., Gonzalez, B., Morata, L., Rico, V., & Soriano, A. (2021). rUTI resolution after FMT for Clostridioides difficile Infection: A case report. Infectious Diseases and Therapy, 10, 1065–1071.
Danne, C., Rolhion, N., & Sokol, H. (2021). Recipient factors in faecal microbiota transplantation: One stool does not fit all. Nature Reviews. Gastroenterology & Hepatology, 18, 503–513.
Cui, B., Xu, F., & Zhang, F. (2016). Methodology, not concept of fecal microbiota transplantation, affects clinical findings. Gastroenterology, 150, 285–286.
Zhang, X. Y., Chen, Q. Y., Li, N., & Qin, H. L. (2020) [Indication selection and clinical application strategies of fecal microbiota transplantation]. Zhonghua Wei Chang Wai Ke Za Zhi = Chinese Journal of Gastrointestinal Surgery, 23, 509–515.
Papanicolas, L. E., Choo, J. M., Wang, Y., Leong, L. E. X., Costello, S. P., Gordon, D. L., Wesselingh, S. L., & Rogers, G. B. (2019). Bacterial viability in faecal transplants: Which bacteria survive? eBioMedicine, 41, 509–516.
Lin, C., Wan, J., Lu, Y., Zhang, H., Chen, X., Su, Y., & Zhu, W. (2019). Active bacterial communities of pig fecal microbiota transplantation suspension prepared and preserved under different conditions. AMB Express, 9, 63.
Wu, Z., Huang, S., Li, T., Li, N., Han, D., Zhang, B., Xu, Z. Z., Zhang, S., Pang, J., Wang, S., Zhang, G., Zhao, J., & Wang, J. (2021). Gut microbiota from green tea polyphenol-dosed mice improves intestinal epithelial homeostasis and ameliorates experimental colitis. Microbiome, 9, 184.
Zhong, Y., Cao, J., Deng, Z., Ma, Y., Liu, J., & Wang, H. (2021). Effect of fiber and fecal microbiota transplantation donor on recipient mice gut microbiota. Frontiers in Microbiology, 12, 757372.
Zhou, D., Pan, Q., Shen, F., Cao, H. X., Ding, W. J., Chen, Y. W., & Fan, J. G. (2017). Total fecal microbiota transplantation alleviates high-fat diet-induced steatohepatitis in mice via beneficial regulation of gut microbiota. Science and Reports, 7, 1529.
Ding, N., Zhang, X., Zhang, X. D., Jing, J., Liu, S. S., Mu, Y. P., Peng, L. L., Yan, Y. J., Xiao, G. M., Bi, X. Y., Chen, H., Li, F. H., Yao, B., & Zhao, A. Z. (2020). Impairment of spermatogenesis and sperm motility by the high-fat diet-induced dysbiosis of gut microbes. Gut, 69, 1608–1619.
He, Y., Li, X., Yu, H., Ge, Y., Liu, Y., Qin, X., Jiang, M., & Wang, X. (2019). The functional role of fecal microbiota transplantation on dextran sulfate sodium-induced colitis in mice. Frontiers in Cellular and Infection Microbiology, 9, 393.
Magne, F., Gotteland, M., Gauthier, L., Zazueta, A., Pesoa, S., Navarrete, P., & Balamurugan, R. (2020). The firmicutes/bacteroidetes ratio: A relevant marker of gut dysbiosis in obese patients? Nutrients, 12(5), 1474.
Yang, X., Tang, T., Wen, J., Li, M., Chen, J., Li, T., Dai, Y., & Cheng, Q. (2021). Effects of S24–7 on the weight of progeny rats after exposure to ceftriaxone sodium during pregnancy. BMC Microbiology, 21, 166.
Galle, F., Valeriani, F., Cattaruzza, M. S., Gianfranceschi, G., Liguori, R., Antinozzi, M., Mederer, B., Liguori, G., & Romano Spica, V. (2020). Mediterranean diet, physical activity and gut microbiome composition: A cross-sectional study among healthy young italian adults. Nutrients, 12(7), 2164.
Chen, T., Ding, R., Chen, X., Lu, Y., Shi, J., Lu, Y., Tang, B., Zhang, W., Ye, C., Yuan, M., & Yang, Z. (2021). Firmicutes and Blautia in gut microbiota lessened in chronic liver diseases and hepatocellular carcinoma patients: A pilot study. Bioengineered, 12, 8233–8246.
Zou, Y., Ju, X., Chen, W., Yuan, J., Wang, Z., Aluko, R. E., & He, R. (2020). Rice bran attenuated obesity via alleviating dyslipidemia, browning of white adipocytes and modulating gut microbiota in high-fat diet-induced obese mice. Food & Function, 11, 2406–2417.
Bervoets, L., Van Hoorenbeeck, K., Kortleven, I., Van Noten, C., Hens, N., Vael, C., Goossens, H., Desager, K. N., & Vankerckhoven, V. (2013). Differences in gut microbiota composition between obese and lean children: A cross-sectional study. Gut Pathogens, 5, 10.
Pinart, M., Dotsch, A., Schlicht, K., Laudes, M., Bouwman, J., Forslund, S. K., Pischon, T., & Nimptsch, K. (2021). Gut microbiome composition in obese and non-obese persons: A systematic review and meta-analysis. Nutrients, 14, 12.
Grigor’eva, I. N. (2020). Gallstone disease, obesity and the firmicutes/bacteroidetes ratio as a possible biomarker of gut dysbiosis. Journal of Personalized Medicine, 11, 13.
Ormerod, K. L., Wood, D. L., Lachner, N., Gellatly, S. L., Daly, J. N., Parsons, J. D., Dal’Molin, C. G., Palfreyman, R. W., Nielsen, L. K., Cooper, M. A., Morrison, M., Hansbro, P. M., & Hugenholtz, P. (2016). Genomic characterization of the uncultured Bacteroidales family S24–7 inhabiting the guts of homeothermic animals. Microbiome, 4, 36.
Osborne, G., Wu, F., Yang, L., Kelly, D., Hu, J., Li, H., Jasmine, F., Kibriya, M. G., Parvez, F., Shaheen, I., Sarwar, G., Ahmed, A., Eunus, M., Islam, T., Pei, Z., Ahsan, H., & Chen, Y. (2020). The association between gut microbiome and anthropometric measurements in Bangladesh. Gut Microbes, 11, 63–76.
Yu, F., Han, W., Zhan, G., Li, S., Jiang, X., Wang, L., Xiang, S., Zhu, B., Yang, L., Luo, A., Hua, F., & Yang, C. (2019). Abnormal gut microbiota composition contributes to the development of type 2 diabetes mellitus in db/db mice. Aging, 11, 10454–10467.
Creedon, A. C., Hung, E. S., Berry, S. E., & Whelan, K. (2020). Nuts and their effect on gut microbiota, gut function and symptoms in adults: A systematic review and meta-analysis of randomised controlled trials. Nutrients, 12(8), 2347.
Liu, H., Wang, J., He, T., Becker, S., Zhang, G., Li, D., & Ma, X. (2018). Butyrate: A double-edged sword for health? Advances in Nutrition, 9, 21–29.
Coppola, S., Avagliano, C., Calignano, A., & Berni Canani, R. (2021). The protective role of butyrate against obesity and obesity-related diseases. Molecules, 26, 682.
Bourassa, M. W., Alim, I., Bultman, S. J., & Ratan, R. R. (2016). Butyrate, neuroepigenetics and the gut microbiome: Can a high fiber diet improve brain health? Neuroscience Letters, 625, 56–63.
Li, J., Ma, Y., Bao, Z., Gui, X., Li, A. N., Yang, Z., & Li, M. D. (2020). Clostridiales are predominant microbes that mediate psychiatric disorders. Journal of Psychiatric Research, 130, 48–56.
Kuehne, S. A., Rood, J. I., & Lyras, D. (2019). Clostridial genetics: Genetic manipulation of the pathogenic clostridia. Microbiology Spectrum. https://doi.org/10.1128/microbiolspec.GPP3-0040-2018
Revitt-Mills, S. A., Vidor, C. J., Watts, T. D., Lyras, D., Rood, J. I., & Adams, V. (2019). Virulence plasmids of the pathogenic clostridia. Microbiology Spectrum. https://doi.org/10.1128/microbiolspec.GPP3-0034-2018
Krych, L., Hansen, C. H., Hansen, A. K., van den Berg, F. W., & Nielsen, D. S. (2013). Quantitatively different, yet qualitatively alike: A meta-analysis of the mouse core gut microbiome with a view towards the human gut microbiome. PLoS ONE, 8, e62578.
Mayorga Reyes, L., Gonzalez Vazquez, R., Cruz Arroyo, S. M., Melendez Avalos, A., Reyes Castillo, P. A., Chavaro Perez, D. A., Ramos Terrones, I., Ramos Ibanez, N., Rodriguez Magallanes, M. M., Langella, P., Bermudez-Humaran, L. G., & Azaola Espinosa, A. (2016). Correlation between diet and gut bacteria in a population of young adults. International Journal of Food Sciences and Nutrition, 67, 470–478.
Zhong, Y., Cao, J., Deng, Z., Ma, Y., Liu, J., & Wang, H. (2021). Effect of fiber and fecal microbiota transplantation donor on recipient mice gut microbiota. Fronties in Microbiology, 12, 757372.
Funding
This research was funded by the Zhejiang Provincial Natural Science Foundation of China (Nos. LGF19H030006 and LQ20H030001), Ningbo Science and Technology Project (No. 2019C50100), and Ningbo Clinical Medicine Research Center Project (No. 2019A21003).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author reports no conflicts of interest in this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mi, F., Wang, X., Zheng, W. et al. Effects of Different Preparation Methods on Microbiota Composition of Fecal Suspension. Mol Biotechnol 65, 871–880 (2023). https://doi.org/10.1007/s12033-022-00590-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12033-022-00590-1