Abstract
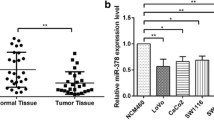
Accumulating studies have demonstrated that CADM2 modulated malignant phenotype of various cancer cells, while its regulatory function and mechanism have not yet been reported. In this study, qRT-PCR was utilized to measure CADM2 mRNA level in normal cells and colon cancer cells, also, IHC and WB were applied to detect CADM2 protein expression in colon tissues, exhibiting low mRNA and protein levels of CADM2 in colon cancer. Applying cell function experiments, the impacts of CADM2 on colon cell phenotypes were examined, and the results illustrated that upregulating CADM2 remarkably repressed proliferation, invasion, migration, cell cycle of colon cancer cells, and facilitated cell apoptosis. Thus, it could be considered that CADM2 served as a tumor repressor gene in colon cancer. Moreover, the outcomes of dual-luciferase assay displayed that miR-17-5p could target CADM2, and overexpressing miR-17-5p could notably inhibit the mRNA and protein expression levels of CADM2. We, therefore, assumed that CADM2 was a downstream target of miR-139-5p. qRT-PCR was conducted to assess miR-17-5p level in colon cancer cells and normal cells, verifying a high miR-17-5p expression in the cancer cells. The effects of miR-17-5p on colon cell phenotypes were examined as well, where we determined that miR-17-5p served as a tumor-promoting factor. Finally, the rescue experiments exhibited that miR-17-5p could activate tumor-promoting phenotypes, while such activating effects could be reversed by upregulating CADM2. In short, the study proved that miR-17-5p facilitated malignant progression of colon cancer through targeting CADM2 at a post-transcriptional level. Our findings offer new insight into molecular therapy of colon cancer patients.








Similar content being viewed by others
Data Availability
The data used to support the findings of this study are included within the article. The data and materials in the current study are available from the corresponding author on reasonable request.
References
Wu, J., Long, Z., Cai, H., Du, C., Liu, X., Yu, S. & Wang, Y. (2016). High expression of WISP1 in colon cancer is associated with apoptosis, invasion and poor prognosis. Oncotarget, 7, 49834–49847. https://doi.org/10.18632/oncotarget.10486
Shi, Y., Huang, X. X., Chen, G. B., Wang, Y., Zhi, Q., Liu, Y. S., Wu, X. L., Wang, L. F., Yang, B., Xiao, C. X., Xing, H. Q., Ren, J. L., Xia, Y. & Guleng, B. (2016). Dragon (RGMb) induces oxaliplatin resistance in colon cancer cells. Oncotarget, 7, 48027–48037. https://doi.org/10.18632/oncotarget.10338
Li, C., Shen, Z., Zhou, Y., & Yu, W. (2018). Independent prognostic genes and mechanism investigation for colon cancer. Biological Research, 51, 10. https://doi.org/10.1186/s40659-018-0158-7
Dienstmann, R., Salazar, R., & Tabernero, J. (2015). Personalizing colon cancer adjuvant therapy: Selecting optimal treatments for individual patients. Journal of Clinical Oncology, 33, 1787–1796. https://doi.org/10.1200/JCO.2014.60.0213
Fritzmann, J., Morkel, M., Besser, D., Budczies, J., Kosel, F., Brembeck, F. H., Stein, U., Fichtner, I., Schlag, P. M. & Birchmeier, W. (2009). A colorectal cancer expression profile that includes transforming growth factor beta inhibitor BAMBI predicts metastatic potential. Gastroenterology, 137, 165–175. https://doi.org/10.1053/j.gastro.2009.03.041
Benson, A. B., Venook, A. P., Al-Hawary, M. M., Arain, M. A., Chen, Y. J., Ciombor, K. K., Cohen, S., Cooper, H. S., Deming, D., Garrido-Laguna, I., Grem, J. L., Gunn, A., Hoffe, S., Hubbard, J., Hunt, S., Kirilcuk, N., Krishnamurthi, S., Messersmith, W. A., Meyerhardt, J., Miller, E. D., Mulcahy, M. F., Nurkin, S., Overman, M. J., Parikh, A., Patel, H., Pedersen, K., Saltz, L., Schneider, C., Shibata, D., Skibber, J. M., Sofocleous, C. T., Stoffel, E. M., Stotsky-Himelfarb, E., Willett, C. G., Johnson-Chilla, A. & Gurski, L. A. (2020). NCCN guidelines insights: Rectal cancer, version 6.2020. Journal of the National Comprehensive Cancer Network, 18, 806–815. https://doi.org/10.6004/jnccn.2020.0032
Huynh, J. C., Schwab, E., Ji, J., Kim, E., Joseph, A., Hendifar, A., Cho, M. & Gong, J. (2020). Recent advances in targeted therapies for advanced gastrointestinal malignancies. Cancers (Basel). https://doi.org/10.3390/cancers12051168
Chang, G., Xu, S., Dhir, R., Chandran, U., O'Keefe, D. S., Greenberg, N. M. & Gingrich, J. R. (2010). Hypoexpression and epigenetic regulation of candidate tumor suppressor gene CADM-2 in human prostate cancer. Clinical Cancer Research, 16, 5390–5401. https://doi.org/10.1158/1078-0432.CCR-10-1461
Morris, J., Bailey, M. E. S., Baldassarre, D., Cullen, B., de Faire, U., Ferguson, A., Gigante, B., Giral, P., Goel, A., Graham, N., Hamsten, A., Humphries, S. E., Johnston, K. J. A., Lyall, D. M., Lyall, L. M., Sennblad, B., Silveira, A., Smit, A. J., Tremoli, E., Veglia, F., Ward, J., Watkins, H., Smith, D. J. & Strawbridge, R. J. (2019). Genetic variation in CADM2 as a link between psychological traits and obesity. Science and Reports, 9, 7339. https://doi.org/10.1038/s41598-019-43861-9
Greenbaum, L., Ravona-Springer, R., Livny, A., Shelly, S., Sharvit-Ginon, I., Ganmore, I., Alkelai, A., Heymann, A. & Schnaider Beeri, M. (2019). The CADM2 gene is associated with processing speed performance—Evidence among elderly with type 2 diabetes. The World Journal of Biological Psychiatry, 20, 577–583. https://doi.org/10.1080/15622975.2017.1366055
Hiruma, A., Ikeda, S., Terui, T., Ozawa, M., Hashimoto, T., Yasumoto, S., Nakayama, J., Kubota, Y., Iijima, M., Sueki, H., Matsumoto, Y., Kato, M., Akasaka, E., Ikoma, N., Mabuchi, T., Tamiya, S., Matsuyama, T., Ozawa, A., Inoko, H. & Oka, A. (2011). A novel splicing variant of CADM2 as a protective transcript of psoriasis. Biochemical and Biophysical Research Communications, 412, 626–632. https://doi.org/10.1016/j.bbrc.2011.08.013
Liu, Y., Li, Y., Ren, Z., Si, W., Li, Y., Wei, G., Zhao, W., Zhou, J., Tian, Y. & Chen, D. (2017). MicroRNA-125a-3p is involved in early behavioral disorders in stroke-afflicted rats through the regulation of Cadm2. International Journal of Molecular Medicine, 40, 1851–1859. https://doi.org/10.3892/ijmm.2017.3179
Dai, L., Zhao, J., Yin, J., Fu, W., & Chen, G. (2020). Cell adhesion molecule 2 (CADM2) promotes brain metastasis by inducing epithelial-mesenchymal transition (EMT) in human non-small cell lung cancer. Annals of Translational Medicine, 8, 465. https://doi.org/10.21037/atm.2020.03.85
Liu, N., Yang, C., Bai, W., Wang, Z., Wang, X., Johnson, M., Wang, W., Zhang, P., Yang, H., Liu, H., Cheng, Y. & Tu, Y. (2019). CADM2 inhibits human glioma proliferation, migration and invasion. Oncology Reports, 41, 2273–2280. https://doi.org/10.3892/or.2019.7010
Li, X., Chen, D., Li, M., Gao, X., Shi, G. & Zhao, H. (2018). The CADM2/Akt pathway is involved in the inhibitory effect of miR-21-5p downregulation on proliferation and apoptosis in esophageal squamous cell carcinoma cells. Chemico-Biological Interactions, 288, 76–82. https://doi.org/10.1016/j.cbi.2018.04.021
Li, D., Zhang, Y., Zhang, H., Zhan, C., Li, X., Ba, T., Qiu, Z., E, F., Lv, G., Zou, C., Wang, C., Si, L., Zou, C., Li, Q. & Gao, X. (2018). CADM2, as a new target of miR-10b, promotes tumor metastasis through FAK/AKT pathway in hepatocellular carcinoma. Journal of Experimental & Clinical Cancer Research, 37, 46. https://doi.org/10.1186/s13046-018-0699-1
Yang, L., Zhao, G., Wang, F., Li, C., & Wang, X. (2018). Hypoxia-regulated miR-146a targets cell adhesion molecule 2 to promote proliferation, migration, and invasion of clear cell renal cell carcinoma. Cellular Physiology and Biochemistry, 49, 920–931. https://doi.org/10.1159/000493224
Alvarez-Garcia, I., & Miska, E. A. (2005). MicroRNA functions in animal development and human disease. Development, 132, 4653–4662. https://doi.org/10.1242/dev.02073
He, J., Zhou, X., Li, L., & Han, Z. (2020). Long noncoding MAGI2-AS3 suppresses several cellular processes of lung squamous cell carcinoma cells by regulating miR-374a/b-5p/CADM2 axis. Cancer Management and Research, 12, 289–302. https://doi.org/10.2147/CMAR.S232595
Kilpelainen, T. P., Hellinen, L., Vrijdag, J., Yan, X., Svarcbahs, R., Vellonen, K. S., Lambeir, A. M., Huttunen, H., Urtti, A., Wallen, E. A. A. & Myohanen, T. T. (2020). The effect of prolyl oligopeptidase inhibitors on alpha-synuclein aggregation and autophagy cannot be predicted by their inhibitory efficacy. Biomedicine & Pharmacotherapy, 128, 110253. https://doi.org/10.1016/j.biopha.2020.110253
Wang, J. X., Jia, X. J., Liu, Y., Dong, J. H., Ren, X. M., Xu, O., Liu, S. H. & Shan, C. G. (2020). Silencing of miR-17-5p suppresses cell proliferation and promotes cell apoptosis by directly targeting PIK3R1 in laryngeal squamous cell carcinoma. Cancer Cell International, 20, 14. https://doi.org/10.1186/s12935-020-1096-3
Xu, J., Meng, Q., Li, X., Yang, H., Xu, J., Gao, N., Sun, H., Wu, S., Familiari, G., Relucenti, M., Zhu, H., Wu, J. & Chen, R. (2019). Long noncoding RNA MIR17HG promotes colorectal cancer progression via miR-17-5p. Cancer Research, 79, 4882–4895. https://doi.org/10.1158/0008-5472.CAN-18-3880
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YW and JZ: Contributed to the study design. HL: Conducted the literature search. YW: Acquired the data. JG: Wrote the article. HY: Performed data analysis and drafted. HL: Revised the article. All the authors gave the final approval of the version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical Approval
This research approved by Ethics Committee of Tangshan Central Hospital.
Informed consent
All patients participated in were informed and supplied the consent forms.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Y., Zhao, J., Wang, Y. et al. MiR-17-5p Targets and Downregulates CADM2, Activating the Malignant Phenotypes of Colon Cancer Cells. Mol Biotechnol 64, 1388–1400 (2022). https://doi.org/10.1007/s12033-022-00515-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12033-022-00515-y