Abstract
Cancer is one of the most challenging diseases to manage. A sizeable number of researches are done each year to find better diagnostic and therapeutic strategies. At the present time, a package of chemotherapy, targeted therapy, radiotherapy, and immunotherapy is available to cope with cancer cells. Regarding chemo-radiation therapy, low effectiveness and normal tissue toxicity are like barriers against optimal response. To remedy the situation, some agents have been proposed as adjuvants to improve tumor responses. Statins, the known substances for reducing lipid, have shown a considerable capability for cancer treatment. Among them, atorvastatin as a reductase (HMG-CoA) inhibitor might affect proliferation, migration, and survival of cancer cells. Since finding an appropriate adjutant is of great importance, numerous studies have been conducted to precisely unveil antitumor effects of atorvastatin and its associated pathways. In this review, we aim to comprehensively review the most highlighted studies which focus on the use of atorvastatin in cancer therapy.

Similar content being viewed by others
Data Availability
All the data used in the article is available.
Abbreviations
- ATV/AVT/AT:
-
Atorvastatin
- HMG-CoA:
-
3-hydroxy-3-methylglutaryl coenzyme A
- HMGCR:
-
3-hydroxy-3-methylglutaryl coenzyme A reductase
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- VLDL:
-
Very -low-density lipoprotein
- LDL-C:
-
Low-density lipoprotein cholesterol
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- ROS:
-
Reactive oxygen species
- SOD:
-
Superoxide dismutase
- CAT:
-
Catalase
- GSH:
-
Glutathione
- GPx:
-
Glutathione peroxidase
- MDA:
-
Malondialdehyde
- NADPH:
-
Nicotinamide Adenine Dinucleotide Phosphate
- NOX:
-
Nicotinamide Adenine Dinucleotide Phosphate oxidase
- OSA:
-
Obstructive sleep apnea
- COX-2 :
-
Cyclooxygenase-2
- ERK:
-
Extracellular signal-regulated kinase
- MEK:
-
Mitogen-activated protein kinase kinase
- IκBα:
-
Nuclear factor-kappa B inhibitor alpha
- IL-1:
-
Interleukin-1
- TNF-α:
-
Tumor necrosis factor alpha
- apoE/LDL:
-
Apolipoprotein E /Low-density lipoprotein
- CRP:
-
C-reactive protein
- ACS:
-
Acute coronary syndrome
- COPD:
-
Chronic obstructive pulmonary disease
- DM:
-
Diabetes mellitus
- sVCAM‐1:
-
Soluble vascular cell adhesion molecule‐1
- ADMA:
-
Asymmetrical dimethyl arginine
- JNK:
-
Jun N-terminal kinases
- GGPP:
-
Geranylgeranyldiphosphate
- MEV:
-
Mevalonate
- AKT/mTOR:
-
Protein kinase B /mammalian target of rapamycin
- MAPK:
-
Mitogen-activated protein kinases
- NLCs:
-
Nanostructured lipid carriers
- LC3-II:
-
Light chain 3B-phosphatidylethanolamine conjugate
- Bcl-2:
-
B-cell lymphoma 2
- PC:
-
Prostate cancer
- PARP:
-
Poly ADP ribose polymerase
- PGE2:
-
Prostaglandin E2
- MA:
-
Mannitol
- TZB:
-
Trastuzumab
- CCA:
-
Cholangiocarcinoma
- DOX:
-
Doxorubicin
- 5-FU:
-
5-fluorouracil
- Hsp70:
-
Heat shock protein 70
- HCC:
-
Hepatocellular carcinoma
- BC:
-
Breast cancer
- MMP2:
-
Matrix metalloprotease 2
- VEGFR:
-
Vascular endothelial growth factor receptor
- PDGFR:
-
Platelet-derived growth factor receptor
- RAS:
-
Rat sarcoma virus
- RAF:
-
Rapidly accelerated fibrosarcoma
- EGFR:
-
Epidermal growth factor receptor
- KRAS:
-
Kirsten rat sarcoma virus
- PIK3:
-
Phosphoinositide 3-kinases
- PTEN:
-
Phosphatase and Tensin homolog
- RhoA:
-
Ras homolog family member A
- ROCK:
-
Rho‐associated coiled‐coil containing kinase
- HDM2:
-
Human Double Minute-2
- mRNA:
-
Messenger Ribonucleic acid
- NBS-1:
-
Nijmegen Breakage Syndrome-1
- TM:
-
Thrombomodulin
- PAI-1:
-
Plasminogen activator inhibitor-1
- Cx43:
-
Connexin 43
- miR-21:
-
MicroRNA-21
- HIF-1:
-
Hypoxia-Inducible Factor 1
- MSH2:
-
Mismatch repair protein 2
- IR:
-
Ionizing Radiation
- BIM:
-
Bcl-2-like protein 11
- TKI:
-
Tyrosine kinase inhibitor
- PT:
-
Phloretin
- MM:
-
Multiple myeloma
- SREBP-2:
-
Sterol regulatory element-binding protein
- γ-TT:
-
γ-Tocotrienol
- CXIB:
-
Celecoxib
- SM:
-
Silymarin
- HCV:
-
Hepatitis C virus
- GTP:
-
Guanosine triphosphate
References
Chaffer CL, Weinberg RA. A perspective on cancer cell metastasis. Science. 2011. https://doi.org/10.1126/science.1203543.
Smith RA, Andrews KS, Brooks D, Fedewa SA, Manassaram-Baptiste D, Saslow D, Wender RC. Cancer screening in the United States, 2019: A review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. 2019. https://doi.org/10.3322/caac.21557.
Smith RA, Oeffinger KC. The importance of cancer screening. Med Clin North Am. 2020. https://doi.org/10.1016/j.mcna.2020.08.008.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021. https://doi.org/10.3322/caac.21660.
Hausman DM. What is cancer? Perspect Biol Med. 2019. https://doi.org/10.1353/pbm.2019.0046.
Alizadeh AA, Aranda V, Bardelli A, Blanpain C, Bock C, Borowski C, Caldas C, Califano A, Doherty M, Elsner M, Esteller M, Fitzgerald R, Korbel JO, Lichter P, Mason CE, Navin N, Pe’er D, Polyak K, Roberts CW, Siu L, Snyder A, Stower H, Swanton C, Verhaak RG, Zenklusen JC, Zuber J, Zucman-Rossi J. Toward understanding and exploiting tumor heterogeneity. Nat Med. 2015. https://doi.org/10.1038/nm.3915.
Kentsis A. Why do young people get cancer? Pediatr Blood Cancer. 2020. https://doi.org/10.1002/pbc.28335.
Marusyk A, Almendro V, Polyak K. Intra-tumour heterogeneity: a looking glass for cancer? Nat Rev Cancer. 2012. https://doi.org/10.1038/nrc3261.
Arruebo M, Vilaboa N, Sáez-Gutierrez B, Lambea J, Tres A, Valladares M, González-Fernández A. Assessment of the evolution of cancer treatment therapies. Cancers (Basel). 2011. https://doi.org/10.3390/cancers3033279.
Liu YQ, Wang XL, He DH, Cheng YX. Protection against chemotherapy- and radiotherapy-induced side effects: a review based on the mechanisms and therapeutic opportunities of phytochemicals. Phytomedicine. 2021. https://doi.org/10.1016/j.phymed.2020.153402.
Ng WL, Huang Q, Liu X, Zimmerman M, Li F, Li CY. Molecular mechanisms involved in tumor repopulation after radiotherapy. Transl Cancer Res. 2013. https://doi.org/10.3978/j.issn.2218-676X.2013.10.03.
Selzer E, Kornek G. Targeted drugs in combination with radiotherapy for the treatment of solid tumors: current state and future developments. Expert Rev Clin Pharmacol. 2013. https://doi.org/10.1586/17512433.2013.841540.
Asghari M, Shaghaghi Z, Farzipour S, Ghasemi A, Hosseinimehr SJ. Radioprotective effect of olanzapine as an anti-psychotic drug against genotoxicity and apoptosis induced by ionizing radiation on human lymphocytes. Mol Biol Rep. 2019. https://doi.org/10.1007/s11033-019-05024-x.
Pouri M, Shaghaghi Z, Ghasemi A, Hosseinimehr SJ. Radioprotective effect of gliclazide as an anti-hyperglycemic agent against genotoxicity induced by ionizing radiation on human lymphocytes. Cardiovasc Hematol Agents Med Chem. 2019. https://doi.org/10.2174/1871525717666190524092918.
Shaghaghi Z, Alvandi M, Nosrati S, Hadei SK. Potential utility of peptides against damage induced by ionizing radiation. Future Oncol. 2021. https://doi.org/10.2217/fon-2020-0577.
Reiss AB, Wirkowski E. Statins in neurological disorders: mechanisms and therapeutic value. Sci World J. 2009. https://doi.org/10.1100/tsw.2009.141.
Ferro D, Parrotto S, Basili S, Alessandri C, Violi F. Simvastatin inhibits the monocyte expression of proinflammatory cytokines in patients with hypercholesterolemia. J Am Coll Cardiol. 2000. https://doi.org/10.1016/s0735-1097(00)00771-3.
Solheim S, Seljeflot I, Arnesen H, Eritsland J, Eikvar L. Reduced levels of TNF alpha in hypercholesterolemic individuals after treatment with pravastatin for 8 weeks. Atherosclerosis. 2001. https://doi.org/10.1016/s0021-9150(00)00725-5.
Zhou Q, Liao JK. Pleiotropic effects of statins-basic research and clinical perspectives. Circ J. 2010;74(5):818–26.
Hosseinimehr SJ, Ghasemi F, Flahatgar F, Rahmanian N, Ghasemi A, Asgarian-Omran H. Atorvastatin sensitizes breast and lung cancer cells to ionizing radiation. Iran J Pharm Res. 2020. https://doi.org/10.22037/ijpr.2020.15487.13126.
Beckwitt CH, Shiraha K, Wells A. Lipophilic statins limit cancer cell growth and survival, via involvement of Akt signaling. PLoS One. 2018. https://doi.org/10.1371/journal.pone.0197422.
Cai J, Yu X, Zhang B, Zhang H, Fang Y, Liu S, Liu T, Ding X. Atorvastatin improves survival of implanted stem cells in a rat model of renal ischemia-reperfusion injury. Am J Nephrol. 2014. https://doi.org/10.1159/000362623.
Crevar-Sakac M, Vujić Z, Kotur-Stevuljević J, Ivanisević J, Jelić-Ivanović Z, Milenković M, Markelić M, Vujcić Z. Effects of atorvastatin and artichoke leaf tincture on oxidative stress in hypercholesterolemic rats. Vojnosanit Pregl. 2016. https://doi.org/10.2298/vsp140917148c.
Davignon J. Beneficial cardiovascular pleiotropic effects of statins. Circulation. 2004. https://doi.org/10.1161/01.CIR.0000131517.20177.5a.
Jaikumkao K, Pongchaidecha A, Thongnak LO, Wanchai K, Arjinajarn P, Chatsudthipong V, Chattipakorn N, Lungkaphin A. Amelioration of renal inflammation, endoplasmic reticulum stress and apoptosis underlies the protective effect of low dosage of atorvastatin in gentamicin-induced nephrotoxicity. PLoS One. 2016. https://doi.org/10.1371/journal.pone.0164528.
Ramanjaneyulu SV, Trivedi PP, Kushwaha S, Vikram A, Jena GB. Protective role of atorvastatin against doxorubicin-induced cardiotoxicity and testicular toxicity in mice. J Physiol Biochem. 2013. https://doi.org/10.1007/s13105-013-0240-0.
Yang PM, Liu YL, Lin YC, Shun CT, Wu MS, Chen CC. Inhibition of autophagy enhances anticancer effects of atorvastatin in digestive malignancies. Cancer Res. 2010. https://doi.org/10.1158/0008-5472.CAN-10-1626.
Zhang K, He X, Zhou Y, Gao L, Qi Z, Chen J, Gao X. Atorvastatin ameliorates radiation-induced cardiac fibrosis in rats. Radiat Res. 2015. https://doi.org/10.1667/RR14075.1.
Wiklund O, Mattsson-Hultén L, Hurt-Camejo E, Oscarsson J. Effects of simvastatin and atorvastatin on inflammation markers in plasma. J Intern Med. 2002. https://doi.org/10.1046/j.1365-2796.2002.00966.x.
Pal S, Sarkar A, Pal PB, Sil PC. Protective effect of arjunolic acid against atorvastatin induced hepatic and renal pathophysiology via MAPK, mitochondria and ER dependent pathways. Biochimie. 2015. https://doi.org/10.1016/j.biochi.2015.02.016.
Furberg CD. Natural statins and stroke risk. Circulation. 1999. https://doi.org/10.1161/01.cir.99.2.185.
Profumo E, Buttari B, Saso L, Rigano R. Pleiotropic effects of statins in atherosclerotic disease: focus on the antioxidant activity of atorvastatin. Curr Top Med Chem. 2014. https://doi.org/10.2174/1568026614666141203130324.
Oryan A, Kamali A, Moshiri A. Potential mechanisms and applications of statins on osteogenesis: current modalities, conflicts and future directions. J Control Release. 2015. https://doi.org/10.1016/j.jconrel.2015.07.022.
Gazzerro P, Proto MC, Gangemi G, Malfitano AM, Ciaglia E, Pisanti S, Santoro A, Laezza C, Bifulco M. Pharmacological actions of statins: a critical appraisal in the management of cancer. Pharmacol Rev. 2012. https://doi.org/10.1124/pr.111.004994.
Bedi O, Dhawan V, Sharma PL, Kumar P. Pleiotropic effects of statins: new therapeutic targets in drug design. Naunyn Schmiedebergs Arch Pharmacol. 2016. https://doi.org/10.1007/s00210-016-1252-4.
Dulak J, Józkowicz A. Anti-angiogenic and anti-inflammatory effects of statins: relevance to anti-cancer therapy. Curr Cancer Drug Targets. 2005. https://doi.org/10.2174/156800905774932824.
Endres M. Statins and stroke. J Cereb Blood Flow Metab. 2005. https://doi.org/10.1038/sj.jcbfm.9600116.
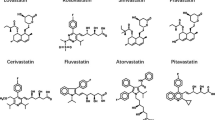
Hamelin BA, Turgeon J. Hydrophilicity/lipophilicity: relevance for the pharmacology and clinical effects of HMG-CoA reductase inhibitors. Trends Pharmacol Sci. 1998. https://doi.org/10.1016/s0165-6147(97)01147-4.
Kato S, Smalley S, Sadarangani A, Chen-Lin K, Oliva B, Brañes J, Carvajal J, Gejman R, Owen GI, Cuello M. Lipophilic but not hydrophilic statins selectively induce cell death in gynaecological cancers expressing high levels of HMGCoA reductase. J Cell Mol Med. 2010. https://doi.org/10.1111/j.1582-4934.2009.00771.x.
Kim J, Choi EA, Han YE, Lee JW, Kim YS, Kim Y, You HS, Hyun HJ, Kang HT. Association between statin use and all-cause mortality in cancer survivors, based on the Korean health insurance service between 2002 and 2015. Nutr Metab Cardiovasc Dis. 2020. https://doi.org/10.1016/j.numecd.2019.11.002.
Ling Q, Tejada-Simon MV. Statins and the brain: new perspective for old drugs. Prog Neuropsychopharmacol Biol Psychiatry. 2016. https://doi.org/10.1016/j.pnpbp.2015.11.013.
Roth BD. The discovery and development of atorvastatin, a potent novel hypolipidemic agent. Prog Med Chem. 2002. https://doi.org/10.1016/s0079-6468(08)70080-8.
van Leuven SI, Kastelein JJ. Atorvastatin. Expert Opin Pharmacother. 2005. https://doi.org/10.1517/14656566.6.7.1191.
Kawahara T, Nishikawa M, Kawahara C, Inazu T, Sakai K, Suzuki G. Atorvastatin, etidronate, or both in patients at high risk for atherosclerotic aortic plaques: a randomized, controlled trial. Circulation. 2013. https://doi.org/10.1161/CIRCULATIONAHA.113.001534.
Kurogi K, Sugiyama S, Sakamoto K, Tayama S, Nakamura S, Biwa T, Matsui K, Ogawa H; COMPACT-CAD Investigators (2013) Comparison of pitavastatin with atorvastatin in increasing HDL-cholesterol and adiponectin in patients with dyslipidemia and coronary artery disease: the COMPACT-CAD study. J Cardiol. https://doi.org/10.1016/j.jjcc.2013.03.008
Blum CB. Comparison of properties of four inhibitors of 3-hydroxy-3-methylglutaryl-coenzyme A reductase. Am J Cardiol. 1994. https://doi.org/10.1016/0002-9149(94)90626-2.
Malhotra HS, Goa KL. Atorvastatin: an updated review of its pharmacological properties and use in dyslipidaemia. Drugs. 2001. https://doi.org/10.2165/00003495-200161120-00012.
Rackley CE. Monotherapy with HMG-CoA reductase inhibitors and secondary prevention in coronary artery disease. Clin Cardiol. 1996. https://doi.org/10.1002/clc.4960190903.
Jose MA, Anandkumar S, Narmadha MP, Sandeep M. A comparative effect of atorvastatin with other statins in patients of hyperlipidemia. Indian J Pharmacol. 2012. https://doi.org/10.4103/0253-7613.93864.
Wassmann S, Laufs U, Müller K, Konkol C, Ahlbory K, Bäumer AT, Linz W, Böhm M, Nickenig G. Cellular antioxidant effects of atorvastatin in vitro and in vivo. Arterioscler Thromb Vasc Biol. 2002. https://doi.org/10.1161/hq0202.104081.
Sarath TS, Waghe P, Gupta P, Choudhury S, Kannan K, Pillai AH, Harikumar SK, Mishra SK, Sarkar SN. Atorvastatin ameliorates arsenic-induced hypertension and enhancement of vascular redox signaling in rats. Toxicol Appl Pharmacol. 2014. https://doi.org/10.1016/j.taap.2014.08.032.
Chandra J, Samali A, Orrenius S. Triggering and modulation of apoptosis by oxidative stress. Free Radic Biol Med. 2000. https://doi.org/10.1016/s0891-5849(00)00302-6.
Poli G, Leonarduzzi G, Biasi F, Chiarpotto E. Oxidative stress and cell signalling. Curr Med Chem. 2004. https://doi.org/10.2174/0929867043365323.
Pillai CK, Pillai KS. Antioxidants in health. Indian J Physiol Pharmacol. 2002;46:1–5.
Hosseinimehr SJ. A review of preventive and therapeutic effects of curcumin in patients with cancer. J Clin Excell. 2014;2:50–63.
Andjelkovic M, Buha Djordjevic A, Antonijevic E, Antonijevic B, Stanic M, Kotur-Stevuljevic J, Spasojevic-Kalimanovska V, Jovanovic M, Boricic N, Wallace D, Bulat Z. Toxic effect of acute cadmium and lead exposure in rat blood, liver, and kidney. Int J Environ Res Public Health. 2019. https://doi.org/10.3390/ijerph16020274.
Hormozi M, Mirzaei R, Nakhaee A, Izadi S, Dehghan Haghighi J. The biochemical effects of occupational exposure to lead and cadmium on markers of oxidative stress and antioxidant enzymes activity in the blood of glazers in tile industry. Toxicol Ind Health. 2018. https://doi.org/10.1177/0748233718769526.
Lambeth JD. NOX enzymes and the biology of reactive oxygen. Nat Rev Immunol. 2004. https://doi.org/10.1038/nri1312.
Zhao W, Robbins ME. Inflammation and chronic oxidative stress in radiation-induced late normal tissue injury: therapeutic implications. Curr Med Chem. 2009. https://doi.org/10.2174/092986709787002790.
Zhou S, Zhao P, Li Y, Deng T, Tian L, Li H. Renoprotective effect of atorvastatin on STZ-diabetic rats through attenuating kidney-associated dysmetabolism. Eur J Pharmacol. 2014. https://doi.org/10.1016/j.ejphar.2014.06.055.
Violi F, Carnevale R, Calvieri C, Nocella C, Falcone M, Farcomeni A, Taliani G, Cangemi R; SIXTUS study group (2015) Nox2 up-regulation is associated with an enhanced risk of atrial fibrillation in patients with pneumonia. Thorax. https://doi.org/10.1136/thoraxjnl-2015-207178
Goettsch C, Goettsch W, Muller G, Seebach J, Schnittler HJ, Morawietz H. Nox4 overexpression activates reactive oxygen species and p38 MAPK in human endothelial cells. Biochem Biophys Res Commun. 2009. https://doi.org/10.1016/j.bbrc.2009.01.107.
Dhesi S, Chu MP, Blevins G, Paterson I, Larratt L, Oudit GY, Kim DH. Cyclophosphamide-induced cardiomyopathy: a case report, review, and recommendations for management. J Investig Med High Impact Case Rep. 2013. https://doi.org/10.1177/2324709613480346.
Kardes O, Civi S, Tufan K, Oyar EO, Omeroglu S, Aykol S. Effects of atorvastatin on experimental spinal cord ischemia-reperfusion injury in rabbits. Turk Neurosurg. 2017. https://doi.org/10.5137/1019-5149.JTN.16627-15.2.
Pignatelli P, Carnevale R, Pastori D, Cangemi R, Napoleone L, Bartimoccia S, Nocella C, Basili S, Violi F. Immediate antioxidant and antiplatelet effect of atorvastatin via inhibition of Nox2. Circulation. 2012. https://doi.org/10.1161/CIRCULATIONAHA.112.095554.
Takemoto M, Node K, Nakagami H, Liao Y, Grimm M, Takemoto Y, Kitakaze M, Liao JK. Statins as antioxidant therapy for preventing cardiac myocyte hypertrophy. J Clin Invest. 2001. https://doi.org/10.1172/JCI13350.
Zhang XB, Cheng HJ, Yuan YT, Chen Y, Chen YY, Chiu KY, Zeng HQ. Atorvastatin attenuates intermittent hypoxia-induced myocardial oxidative stress in a mouse obstructive sleep apnea model. Aging (Albany NY). 2021. https://doi.org/10.18632/aging.203339.
Ghoreshi ZA, Kabirifar R, Khodarahmi A, Karimollah A, Moradi A. The preventive effect of atorvastatin on liver fibrosis in the bile duct ligation rats via antioxidant activity and down-regulation of Rac1 and NOX1. Iran J Basic Med Sci. 2020. https://doi.org/10.22038/IJBMS.2019.33663.8047.
Zhou Q, Liao JK. Pleiotropic effects of statins. Basic research and clinical perspectives. Circ J. 2010. https://doi.org/10.1253/circj.cj-10-0110.
Shao Q, Shen LH, Hu LH, Pu J, Jing Q, He B. Atorvastatin suppresses inflammatory response induced by oxLDL through inhibition of ERK phosphorylation, IκBα degradation, and COX-2 expression in murine macrophages. J Cell Biochem. 2012;113:611–8.
Fraker D, Alexander H, Pass H. Biologic therapy with TNF: systemic administration and isolation-perfusion. In: De Vita V, Hellman S, Rosenberg S, editors. Biologic therapy of cancer: principles and practice. Philadelphia: Lippincott Co.; 1995. p. 329–45.
Nachtigal P, Pospisilova N, Jamborova G, Pospechova K, Solichova D, Andrys C, Zdansky P, Micuda S, Semecky V. Atorvastatin has hypolipidemic and anti-inflammatory effects in apoE/LDL receptor-double-knockout mice. Life Sci. 2008. https://doi.org/10.1016/j.lfs.2008.01.006.
Hoving S, Heeneman S, Gijbels MJ, te Poele JA, Pol JF, Gabriels K, Russell NS, Daemen MJ, Stewart FA. Anti-inflammatory and anti-thrombotic intervention strategies using atorvastatin, clopidogrel and knock-down of CD40L do not modify radiation-induced atherosclerosis in ApoE null mice. Radiother Oncol. 2011. https://doi.org/10.1016/j.radonc.2011.09.019.
Jain MK, Ridker PM. Anti-inflammatory effects of statins: clinical evidence and basic mechanisms. Nat Rev Drug Discov. 2005. https://doi.org/10.1038/nrd1901.
Sun Y, Ji Q, Mei Y, Wang X, Feng J, Cai J, Chi L. Role of preoperative atorvastatin administration in protection against postoperative atrial fibrillation following conventional coronary artery bypass grafting. Int Heart J. 2011. https://doi.org/10.1536/ihj.52.7.
Zheng Z, Jayaram R, Jiang L, Emberson J, Zhao Y, Li Q, Du J, Guarguagli S, Hill M, Chen Z, Collins R, Casadei B. Perioperative rosuvastatin in cardiac surgery. N Engl J Med. 2016. https://doi.org/10.1056/NEJMoa1507750.
Singh P, Emami H, Subramanian S, Maurovich-Horvat P, Marincheva-Savcheva G, Medina HM, Abdelbaky A, Alon A, Shankar SS, Rudd JH, Fayad ZA, Hoffmann U, Tawakol A. Coronary plaque morphology and the anti-inflammatory impact of atorvastatin: a multicenter 18F-fluorodeoxyglucose positron emission tomographic/computed tomographic study. Circ Cardiovasc Imaging. 2016. https://doi.org/10.1161/CIRCIMAGING.115.004195.
Blanco-Colio LM, Martín-Ventura JL, de Teresa E, Farsang C, Gaw A, Gensini G, Leiter LA, Langer A, Martineau P, Egido J; ACTFAST investigators (2008) Atorvastatin decreases elevated soluble CD40L in subjects at high cardiovascular risk. Atorvastatin on inflammatory markers study: a substudy of ACTFAST. Kidney Int Suppl. https://doi.org/10.1038/ki.2008.514
Macin SM, Perna ER, Farías EF, Franciosi V, Cialzeta JR, Brizuela M, Medina F, Tajer C, Doval H, Badaracco R. Atorvastatin has an important acute anti-inflammatory effect in patients with acute coronary syndrome: results of a randomized, double-blind, placebo-controlled study. Am Heart J. 2005. https://doi.org/10.1016/j.ahj.2004.07.041.
Thomson NC, Charron CE, Chaudhuri R, Spears M, Ito K, McSharry C. Atorvastatin in combination with inhaled beclometasone modulates inflammatory sputum mediators in smokers with asthma. Pulm Pharmacol Ther. 2015;31:1–8. https://doi.org/10.1016/j.pupt.2015.01.001.
Liu M, Wang F, Wang Y, Jin R. Atorvastatin improves endothelial function and cardiac performance in patients with dilated cardiomyopathy: the role of inflammation. Cardiovasc Drugs Ther. 2009. https://doi.org/10.1007/s10557-009-6186-3.
Arad Y, Spadaro LA, Roth M, Newstein D, Guerci AD. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin C, and vitamin E: the St. Francis Heart Study randomized clinical trial. J Am Coll Cardiol. 2005. https://doi.org/10.1016/j.jacc.2005.02.089.
Cadirci E, Oral A, Odabasoglu F, Kilic C, Coskun K, Halici Z, Suleyman H, Nuri Keles O, Unal B. Atorvastatin reduces tissue damage in rat ovaries subjected to torsion and detorsion: biochemical and histopathologic evaluation. Naunyn Schmiedebergs Arch Pharmacol. 2010. https://doi.org/10.1007/s00210-010-0504-y.
Castro PF, Miranda R, Verdejo HE, Greig D, Gabrielli LA, Alcaino H, Chiong M, Bustos C, Garcia L, Mellado R, Vukasovic JL, Godoy I, Lavandero S. Pleiotropic effects of atorvastatin in heart failure: role in oxidative stress, inflammation, endothelial function, and exercise capacity. J Heart Lung Transplant. 2008. https://doi.org/10.1016/j.healun.2008.01.012.
Zhang S, Zhang Y, Ahsan MZ, Yuan Y, Liu G, Han X, Zhang J, Zhao X, Bai B, Li Y. Atorvastatin attenuates cold-induced hypertension by preventing gut barrier injury. J Cardiovasc Pharmacol. 2019. https://doi.org/10.1097/FJC.0000000000000690.
Fuentes-Orozco C, Garcia-Salazar SJ, Gómez-Navarro B, González-Espinoza E, Zepeda-González A, Ramírez-Robles JN, Castañeda-Espinoza R, Yáñez-Sánchez I, Gálvez-Gastelum FJ, Cervantes-Guevara G, Cervantes-Cardona GA, Contreras-Hernández GI, Pérez-Landeros JE, García-Martinez D, González-Ojeda A. Anti-inflammatory effect of atorvastatin on the kidney graft of living donor transplants. Ann Transplant. 2018. https://doi.org/10.12659/AOT.908521.
Mroz RM, Lisowski P, Tycinska A, Bierla J, Trzeciak PZ, Minarowski L, Milewski R, Lisowska A, Boros P, Sobkowicz B, Duszewska AM, Chyczewska E, Musial WJ, MacNee W. Anti-inflammatory effects of atorvastatin treatment in chronic obstructive pulmonary disease. A controlled pilot study. J Physiol Pharmacol. 2015;66:111–28.
Khodayar MJ, Kiani M, Hemmati AA, Rezaie A, Zerafatfard MR, Rashidi Nooshabadi MR, Goudarzi M. The preventive effect of atorvastatin on paraquat-induced pulmonary fibrosis in the rats. Adv Pharm Bull. 2014. https://doi.org/10.5681/apb.2014.050.
Tousoulis D, Antoniades C, Vasiliadou C, Kourtellaris P, Koniari K, Marinou K, Charakida M, Ntarladimas I, Siasos G, Stefanadis C. Effects of atorvastatin and vitamin C on forearm hyperaemic blood flow, asymmentrical dimethylarginine levels and the inflammatory process in patients with type 2 diabetes mellitus. Heart. 2007. https://doi.org/10.1136/hrt.2006.093112.
Baluna RG, Eng TY, Thomas CR. Adhesion molecules in radiotherapy. Radiat Res. 2006. https://doi.org/10.1667/RR0380.1.
Furuta Y, Hunter N, Barkley T, Hall E, Milas L. Increase in radioresponse of murine tumors by treatment with indomethacin. Cancer Res. 1988;48:3008–13.
Hallahan D, Kuchibhotla J, Wyble C. Cell adhesion molecules mediate radiation-induced leukocyte adhesion to the vascular endothelium. Cancer Res. 1996;56:5150–5.
Hallahan DE, Virudachalam S. Accumulation of P-selectin in the lumen of irradiated blood vessels. Radiat Res. 1999;152:6–13.
Hong JH, Chiang CS, Campbell IL, Sun JR, Withers HR, McBride WH. Induction of acute phase gene expression by brain irradiation. Int J Radiat Oncol Biol Phys. 1995. https://doi.org/10.1016/0360-3016(95)00279-8.
Richter KK, Fink LM, Hughes BM, Sung CC, Hauer-Jensen M. Is the loss of endothelial thrombomodulin involved in the mechanism of chronicity in late radiation enteropathy? Radiother Oncol. 1997. https://doi.org/10.1016/s0167-8140(97)00063-7.
Rubin P, Johnston CJ, Williams JP, McDonald S, Finkelstein JN. A perpetual cascade of cytokines postirradiation leads to pulmonary fibrosis. Int J Radiat Oncol Biol Phys. 1995. https://doi.org/10.1016/0360-3016(95)00095-G.
Wondergem J, Wedekind LE, Bart CI, Chin A, van der Laarse A, Beekhuizen H. Irradiation of mechanically-injured human arterial endothelial cells leads to increased gene expression and secretion of inflammatory and growth promoting cytokines. Atherosclerosis. 2004. https://doi.org/10.1016/j.atherosclerosis.2004.02.018.
He Z, Yuan J, Qi P, Zhang L, Wang Z. Atorvastatin induces autophagic cell death in prostate cancer cells in vitro. Mol Med Rep. 2015. https://doi.org/10.3892/mmr.2015.3334.
Kang M, Jeong CW, Ku JH, Kwak C, Kim HH. Inhibition of autophagy potentiates atorvastatin-induced apoptotic cell death in human bladder cancer cells in vitro. Int J Mol Sci. 2014. https://doi.org/10.3390/ijms15058106.
Alarcon Martinez T, Zeybek ND, Müftüoğlu S. Evaluation of the cytotoxic and autophagic effects of atorvastatin on MCF-7 breast cancer cells. Balkan Med J. 2018. https://doi.org/10.4274/balkanmedj.2017.0604.
Liang Z, Li W, Liu J, Li J, He F, Jiang Y, Yang L, Li P, Wang B, Wang Y, Ren Y, Yang J, Luo Z, Vaziri C, Liu P. Simvastatin suppresses the DNA replication licensing factor MCM7 and inhibits the growth of tamoxifen-resistant breast cancer cells. Sci Rep. 2017. https://doi.org/10.1038/srep41776.
Liu H, Liang SL, Kumar S, Weyman CM, Liu W, Zhou A. Statins induce apoptosis in ovarian cancer cells through activation of JNK and enhancement of Bim expression. Cancer Chemother Pharmacol. 2009. https://doi.org/10.1007/s00280-008-0830-7.
Sánchez CA, Rodríguez E, Varela E, Zapata E, Páez A, Massó FA, Montaño LF, Lóopez-Marure R. Statin-induced inhibition of MCF-7 breast cancer cell proliferation is related to cell cycle arrest and apoptotic and necrotic cell death mediated by an enhanced oxidative stress. Cancer Invest. 2008. https://doi.org/10.1080/07357900701874658.
Toepfer N, Childress C, Parikh A, Rukstalis D, Yang W. Atorvastatin induces autophagy in prostate cancer PC3 cells through activation of LC3 transcription. Cancer Biol Ther. 2011. https://doi.org/10.4161/cbt.12.8.15978.
Warita K, Warita T, Beckwitt CH, Schurdak ME, Vazquez A, Wells A, Oltvai ZN. Statin-induced mevalonate pathway inhibition attenuates the growth of mesenchymal-like cancer cells that lack functional E-cadherin mediated cell cohesion. Sci Rep. 2014. https://doi.org/10.1038/srep07593.
Jones HM, Fang Z, Sun W, Clark LH, Stine JE, Tran AQ, Sullivan SA, Gilliam TP, Zhou C, Bae-Jump VL. Atorvastatin exhibits anti-tumorigenic and anti-metastatic effects in ovarian cancer in vitro. Am J Cancer Res. 2017;7(12):2478–90 (Erratum in: Am J Cancer Res. 2018;8:915).
Gambhire VM, Salunkhe SM, Gambhire MS. Atorvastatin-loaded lipid nanoparticles: antitumor activity studies on MCF-7 breast cancer cells. Drug Dev Ind Pharm. 2018. https://doi.org/10.1080/03639045.2018.1492605.
Beckwitt CH, Clark AM, Ma B, Whaley D, Oltvai ZN, Wells A. Statins attenuate outgrowth of breast cancer metastases. Br J Cancer. 2018. https://doi.org/10.1038/s41416-018-0267-7.
Hu MB, Zhang JW, Gao JB, Qi YW, Gao Y, Xu L, Ma Y, Wei ZZ. Atorvastatin induces autophagy in MDA-MB-231 breast cancer cells. Ultrastruct Pathol. 2018. https://doi.org/10.1080/01913123.2018.1522406.
Wang Z, Zhang L, Wan Z, He Y, Huang H, Xiang H, Wu X, Zhang K, Liu Y, Goodin S, Du Z, Zheng X. Atorvastatin and caffeine in combination regulates apoptosis, migration, invasion and tumorspheres of prostate cancer cells. Pathol Oncol Res. 2020. https://doi.org/10.1007/s12253-018-0415-7.
Cai S, Chen Q, Xu Y, Zhuang Q, Ji S. Atorvastatin inhibits pancreatic cancer cells proliferation and invasion likely by suppressing neurotrophin receptor signaling. Transl Cancer Res. 2020. https://doi.org/10.21037/tcr.2020.01.27.
Sheng B, Song Y, Zhang J, Li R, Wang Z, Zhu X. Atorvastatin suppresses the progression of cervical cancer via regulation of autophagy. Am J Transl Res. 2020;12:5252–68.
Cai S, Gao Z. Atorvastatin inhibits proliferation and promotes apoptosis of colon cancer cells via COX-2/PGE2/β-catenin pathway. J BUON. 2021;26:1219–25.
Tulbah AS, Gamal A. Design and characterization of atorvastatin dry powder formulation as a potential lung cancer treatment. Saudi Pharm J. 2021. https://doi.org/10.1016/j.jsps.2021.11.002.
Abolghasemi R, Ebrahimi-Barough S, Bahrami N, Ai J. Atorvastatin inhibits viability and migration of MCF7 breast cancer cells. Asian Pac J Cancer Prev. 2022. https://doi.org/10.31557/APJCP.2022.23.3.867.
Abolghasemi R, Ebrahimi-Barough S, Mohamadnia A, Ai J. Synergistic inhibitory effect of human umbilical cord matrix mesenchymal stem cells-conditioned medium and atorvastatin on MCF7 cancer cells viability and migration. Cell Tissue Bank. 2022. https://doi.org/10.1007/s10561-021-09984-y.
Parada B, Reis F, Pinto Â, Sereno J, Xavier-Cunha M, Neto P, Rocha-Pereira P, Mota A, Figueiredo A, Teixeira F. Chemopreventive efficacy of Atorvastatin against nitrosamine-induced rat bladder cancer: antioxidant, anti-proliferative and anti-inflammatory properties. Int J Mol Sci. 2012. https://doi.org/10.3390/ijms13078482.
Lee S, Lee HJ, Kang H, Kim EH, Lim YC, Park H, Lim SM, Lee YJ, Kim JM, Kim JS. Trastuzumab induced chemobrain, atorvastatin rescued chemobrain with enhanced anticancer effect and without hair loss-side effect. J Clin Med. 2019. https://doi.org/10.3390/jcm8020234.
Bao H, Zheng N, Li Z, Zhi Y. Synergistic effect of tangeretin and atorvastatin for colon cancer combination therapy: targeted delivery of these dual drugs using RGD peptide decorated nanocarriers. Drug Des Devel Ther. 2020. https://doi.org/10.2147/DDDT.S256636.
Kitagawa K, Moriya K, Kaji K, Saikawa S, Sato S, Nishimura N, Namisaki T, Akahane T, Mitoro A, Yoshiji H. Atorvastatin augments gemcitabine-mediated anti-cancer effects by inhibiting yes-associated protein in human cholangiocarcinoma cells. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21207588.
El-Khashab IH. Antiangiogenic and proapoptotic activities of atorvastatin and ganoderma lucidum in tumor mouse model via VEGF and caspase-3 pathways. Asian Pac J Cancer Prev. 2021. https://doi.org/10.31557/APJCP.2021.22.4.1095.
Wang SP, Zhou HJ, Chen XP, Ren GY, Ruan XX, Zhang Y, Zhang RL, Chen J. Loss of expression of Kruppel-like factor 6 in primary hepatocellular carcinoma and hepatoma cell lines. J Exp Clin Cancer Res. 2007;26:117–24.
Chanchevalap S, Nandan MO, McConnell BB, Charrier L, Merlin D, Katz JP, Yang VW. Kruppel-like factor 5 is an important mediator for lipopolysaccharide-induced proinflammatory response in intestinal epithelial cells. Nucleic Acids Res. 2006. https://doi.org/10.1093/nar/gkl014.
Mukai S, Hiyama T, Tanaka S, Yoshihara M, Arihiro K, Chayama K. Involvement of Kruppel-like factor 6 (KLF6) mutation in the development of nonpolypoid colorectal carcinoma. World J Gastroenterol. 2007. https://doi.org/10.3748/wjg.v13.i29.3932.
Velarde MC, Zeng Z, McQuown JR, Simmen FA, Simmen RC. Kruppel-like factor 9 is a negative regulator of ligand-dependent estrogen receptor alpha signaling in Ishikawa endometrial adenocarcinoma cells. Mol Endocrinol. 2007. https://doi.org/10.1210/me.2007-0242.
Feldt M, Bjarnadottir O, Kimbung S, Jirström K, Bendahl PO, Veerla S, Grabau D, Hedenfalk I, Borgquist S. Statin-induced anti-proliferative effects via cyclin D1 and p27 in a window-of-opportunity breast cancer trial. J Transl Med. 2015. https://doi.org/10.1186/s12967-015-0486-0.
Tamburrino D, Crippa S, Partelli S, Archibugi L, Arcidiacono PG, Falconi M, Capurso G. Statin use improves survival in patients with pancreatic ductal adenocarcinoma: a meta-analysis. Dig Liver Dis. 2020. https://doi.org/10.1016/j.dld.2020.01.008.
Barnes TA, Amir E, Templeton AJ, Gomez-Garcia S, Navarro B, Seruga B, Ocana A. Efficacy, safety, tolerability and price of newly approved drugs in solid tumors. Cancer Treat Rev. 2017. https://doi.org/10.1016/j.ctrv.2017.03.011.
DeVita VT Jr, Chu E. A history of cancer chemotherapy. Cancer Res. 2008. https://doi.org/10.1158/0008-5472.CAN-07-6611.
Raymond E. Les médicaments chimioprotecteurs. Mécanismes d’action et applications cliniques [Chemoprotectors. Mechanisms of action and clinical applications]. Rev Med Intern. 1996. https://doi.org/10.1016/0248-8663(96)88125-2.
Du X, Li D, Wang G, Fan Y, Li N, Chai L, Li G, Li J. Chemoprotective effect of atorvastatin against benzo(a)pyrene-induced lung cancer via the inhibition of oxidative stress and inflammatory parameters. Ann Transl Med. 2021. https://doi.org/10.21037/atm-20-7770 (Erratum in: Ann Transl Med. 2021 Jul;9(14):1214.).
Tu Q, Cao H, Zhong W, Ding B, Tang X. Atorvastatin protects against cerebral ischemia/reperfusion injury through anti-inflammatory and antioxidant effects. Neural Regen Res. 2014;9(3):268–75. https://doi.org/10.4103/1673-5374.128220.
El-Moselhy MA, El-Sheikh AA. Protective mechanisms of atorvastatin against doxorubicin-induced hepato-renal toxicity. Biomed Pharmacother. 2014. https://doi.org/10.1016/j.biopha.2013.09.001.
Mounier NM, Wahdan SA, Gad AM, Azab SS. Role of inflammatory, oxidative, and ER stress signaling in the neuroprotective effect of atorvastatin against doxorubicin-induced cognitive impairment in rats. Naunyn Schmiedebergs Arch Pharmacol. 2021. https://doi.org/10.1007/s00210-021-02081-7.
Campos MI, Vieira WD, Campos CN, Aarestrup FM, Aarestrup BJ. Atorvastatin and trans-caryophyllene for the prevention of leukopenia in an experimental chemotherapy model in Wistar rats. Mol Clin Oncol. 2015. https://doi.org/10.3892/mco.2015.544.
Hamzeh M, Hosseinimehr SJ, Khalatbary AR, Mohammadi HR, Dashti A, Amiri FT. Atorvastatin mitigates cyclophosphamide-induced hepatotoxicity via suppression of oxidative stress and apoptosis in rat model. Res Pharm Sci. 2018. https://doi.org/10.4103/1735-5362.236837.
Hamzeh M, Hosseinimehr SJ, Mohammadi HR, Yaghubi Beklar S, Dashti A, Talebpour Amiri F. Atorvastatin attenuates the ovarian damage induced by cyclophosphamide in rat: an experimental study. Int J Reprod Biomed. 2018;16:323–34.
Gao G, Jiang S, Ge L, Zhang S, Zhai C, Chen W, Sui S. Atorvastatin improves doxorubicin-induced cardiac dysfunction by modulating Hsp70, Akt, and MAPK signaling pathways. J Cardiovasc Pharmacol. 2019. https://doi.org/10.1097/FJC.0000000000000646.
Karami E, Goodarzi Z, Ghanbari A, Bandegi AR, Yosefi S, Dehdashti A. In vivo antioxidant and kidney protective potential of Atorvastatin against cadmium chloride-induced kidney injury in male Wistar rat. J Toxicol Environ Health. 2022;15:1025–36.
Zamani E, Mohammadbagheri M, Fallah M, Shaki F. Atorvastatin attenuates ethanol-induced hepatotoxicity via antioxidant and anti-inflammatory mechanisms. Res Pharm Sci. 2017. https://doi.org/10.4103/1735-5362.212049.
Bertolini P, Lassalle M, Mercier G, Raquin MA, Izzi G, Corradini N, Hartmann O. Platinum compound-related ototoxicity in children: long-term follow-up reveals continuous worsening of hearing loss. J Pediatr Hematol Oncol. 2004;26:649–55.
Coradini PP, Cigana L, Selistre SG, Rosito LS, Brunetto AL. Ototoxicity from cisplatin therapy in childhood cancer. J Pediatr Hematol Oncol. 2007. https://doi.org/10.1097/MPH.0b013e318059c220.
Frisina RD, Wheeler HE, Fossa SD, Kerns SL, Fung C, Sesso HD, Monahan PO, Feldman DR, Hamilton R, Vaughn DJ, Beard CJ, Budnick A, Johnson EM, Ardeshir-Rouhani-Fard S, Einhorn LH, Lipshultz SE, Dolan ME, Travis LB. Comprehensive audiometric analysis of hearing impairment and tinnitus after cisplatin-based chemotherapy in survivors of adult-onset cancer. J Clin Oncol. 2016. https://doi.org/10.1200/JCO.2016.66.8822.
Knight KR, Chen L, Freyer D, Aplenc R, Bancroft M, Bliss B, Dang H, Gillmeister B, Hendershot E, Kraemer DF, Lindenfeld L, Meza J, Neuwelt EA, Pollock BH, Sung L. Group-Wide, Prospective Study of Ototoxicity Assessment in Children Receiving Cisplatin Chemotherapy (ACCL05C1): A Report From the Children’s Oncology Group. J Clin Oncol. 2017. https://doi.org/10.1200/JCO.2016.69.2319.
Marnitz S, Schermeyer L, Dommerich S, Köhler C, Olze H, Budach V, Martus P. Age-corrected hearing loss after chemoradiation in cervical cancer patients. Strahlenther Onkol. 2018. https://doi.org/10.1007/s00066-018-1347-6.
Fernandez KA, Allen P, Campbell M, Page B, Townes T, Li CM, Cheng H, Garrett J, Mulquin M, Clements A, Mulford D, Ortiz C, Brewer C, Dubno JR, Newlands S, Schmitt NC, Cunningham LL. Atorvastatin is associated with reduced cisplatin-induced hearing loss. J Clin Invest. 2021. https://doi.org/10.1172/JCI142616.
Guo L, Zheng J, Zeng H, Zhang Z, Shao G. Atorvastatin potentiates the chemosensitivity of human liver cancer cells to cisplatin via downregulating YAP1. Oncol Lett. 2021. https://doi.org/10.3892/ol.2020.12343.
Peng P, Wei W, Long C, Li J. Atorvastatin augments temozolomide’s efficacy in glioblastoma via prenylation-dependent inhibition of Ras signaling. Biochem Biophys Res Commun. 2017. https://doi.org/10.1016/j.bbrc.2017.05.147.
Zhou TY, Zhuang LH, Hu Y, Zhou YL, Lin WK, Wang DD, Wan ZQ, Chang LL, Chen Y, Ying MD, Chen ZB, Ye S, Lou JS, He QJ, Zhu H, Yang B. Inactivation of hypoxia-induced YAP by statins overcomes hypoxic resistance tosorafenib in hepatocellular carcinoma cells. Sci Rep. 2016. https://doi.org/10.1038/srep30483.
Murtola TJ, Visvanathan K, Artama M, Vainio H, Pukkala E. Statin use and breast cancer survival: a nationwide cohort study from Finland. PLoS One. 2014. https://doi.org/10.1371/journal.pone.0110231.
Ishikawa T, Hosaka YZ, Beckwitt C, Wells A, Oltvai ZN, Warita K. Concomitant attenuation of HMG-CoA reductase expression potentiates the cancer cell growth-inhibitory effect of statins and expands their efficacy in tumor cells with epithelial characteristics. Oncotarget. 2018. https://doi.org/10.18632/oncotarget.25448.
Fromigué O, Hamidouche Z, Marie PJ. Statin-induced inhibition of 3-hydroxy-3-methyl glutaryl coenzyme a reductase sensitizes human osteosarcoma cells to anticancer drugs. J Pharmacol Exp Ther. 2008. https://doi.org/10.1124/jpet.108.136127.
Henslee AB, Steele TA. Combination statin and chemotherapy inhibits proliferation and cytotoxicity of an aggressive natural killer cell leukemia. Biomark Res. 2018. https://doi.org/10.1186/s40364-018-0140-0.
Wilhelm SM, Adnane L, Newell P, Villanueva A, Llovet JM, Lynch M. Preclinical overview of sorafenib, a multikinase inhibitor that targets both Raf and VEGF and PDGF receptor tyrosine kinase signaling. Mol Cancer Ther. 2008. https://doi.org/10.1158/1535-7163.MCT-08-0013.
Barber TD, Vogelstein B, Kinzler KW, Velculescu VE. Somatic mutations of EGFR in colorectal cancers and glioblastomas. N Engl J Med. 2004. https://doi.org/10.1056/NEJM200412303512724.
Rich JN, Reardon DA, Peery T, Dowell JM, Quinn JA, Penne KL, Wikstrand CJ, Van Duyn LB, Dancey JE, McLendon RE, Kao JC, Stenzel TT, Ahmed Rasheed BK, Tourt-Uhlig SE, Herndon JE 2nd, Vredenburgh JJ, Sampson JH, Friedman AH, Bigner DD, Friedman HS. Phase II trial of gefitinib in recurrent glioblastoma. J Clin Oncol. 2004. https://doi.org/10.1200/JCO.2004.08.110.
Chen J, Bi H, Hou J, Zhang X, Zhang C, Yue L, Wen X, Liu D, Shi H, Yuan J, Liu J, Liu B. Atorvastatin overcomes gefitinib resistance in KRAS mutant human non-small cell lung carcinoma cells. Cell Death Dis. 2013. https://doi.org/10.1038/cddis.2013.312.
Plunkett W, Huang P, Xu YZ, Heinemann V, Grunewald R, Gandhi V. Gemcitabine: metabolism, mechanisms of action, and self-potentiation. Semin Oncol. 1995;22:3–10.
Kawashiri T, Tokunaga A, Kobayashi D, Shimazoe T. Anti-tumor activities of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors and bisphosphonates in pancreatic cell lines which show poor responses to gemcitabine. Biol Pharm Bull. 2020. https://doi.org/10.1248/bpb.b19-00435.
Arun BK, Gong Y, Liu D, Litton JK, Gutierrez-Barrera AM, Jack Lee J, Vornik L, Ibrahim NK, Cornelison T, Hortobagyi GN, Heckman-Stoddard BM, Koenig KB, Alvarez RR, Murray JL, Valero V, Lippman SM, Brown P, Sneige N. Phase I biomarker modulation study of atorvastatin in women at increased risk for breast cancer. Breast Cancer Res Treat. 2016. https://doi.org/10.1007/s10549-016-3849-1.
Borgquist S, Bjarnadottir O, Kimbung S, Ahern TP. Statins: a role in breast cancer therapy? J Intern Med. 2018. https://doi.org/10.1111/joim.12806.
Ji Y, Rounds T, Crocker A, Sussman B, Hovey RC, Kingsley F, Muss HB, Garber JE, Wood ME. The effect of atorvastatin on breast cancer biomarkers in high-risk women. Cancer Prev Res (Phila). 2016. https://doi.org/10.1158/1940-6207.CAPR-15-0300.
Farzipour S, Shaghaghi Z, Raeispour M, Alvandi M, Jalali F, Yazdi A. Evaluation the effect of chelating arms and carrier agents in radiotoxicity of TAT agents. Curr Radiopharm. 2022. https://doi.org/10.2174/1874471015666220510161047.
Shaghaghi Z, Polgardani NZ, Abbasi S, Albooyeh H, Dastranj L, Farzipour S, Alvandi M. Etodolac enhances the radiosensitivity of irradiated HT-29 human colorectal cancer cells. Curr Radiopharm. 2022. https://doi.org/10.2174/1874471015666220321143139.
Citrin DE. Recent Developments in Radiotherapy. N Engl J Med. 2017. https://doi.org/10.1056/NEJMra1608986.
Saenger EL. Radiation accidents. Ann Emerg Med. 1986. https://doi.org/10.1016/s0196-0644(86)80130-5.
Barbalata CI, Tefas LR, Achim M, Tomuta I, Porfire AS. Statins in risk-reduction and treatment of cancer. World J Clin Oncol. 2020. https://doi.org/10.5306/wjco.v11.i8.573.
Kriegs M, Kasten-Pisula U, Rieckmann T, Holst K, Saker J, Dahm-Daphi J, Dikomey E. The epidermal growth factor receptor modulates DNA double-strand break repair by regulating non-homologousend-joining. DNA Repair (Amst). 2010. https://doi.org/10.1016/j.dnarep.2010.05.005.
Rodemann HP, Dittmann K, Toulany M. Radiation-induced EGFR-signaling and control of DNA-damage repair. Int J Radiat Biol. 2007. https://doi.org/10.1080/09553000701769970.
Mahmoudi M, Gorenne I, Mercer J, Figg N, Littlewood T, Bennett M. Statins use a novel Nijmegen breakage syndrome-1-dependent pathway to accelerate DNA repair in vascular smooth muscle cells. Circ Res. 2008. https://doi.org/10.1161/CIRCRESAHA.108.182899.
Ran XZ, Ran X, Zong ZW, Liu DQ, Xiang GM, Su YP, Zheng HE. Protective effect of atorvastatin on radiation-induced vascular endothelial cell injury in vitro. J Radiat Res. 2010. https://doi.org/10.1269/jrr.09119.
Hosseinimehr SJ, Izakmehri M, Ghasemi A. In vitro protective effect of atorvastatin against ionizing radiation induced genotoxicity in human lymphocytes. Cell Mol Biol (Noisy-le-grand). 2015;61:68–71.
Naeimi RA, Talebpour Amiri F, Khalatbary AR, Ghasemi A, Zargari M, Ghesemi M, Hosseinimehr SJ. Atorvastatin mitigates testicular injuries induced by ionizing radiation in mice. Reprod Toxicol. 2017. https://doi.org/10.1016/j.reprotox.2017.06.052.
Talebpour Amiri F, Hamzeh M, Naeimi RA, Ghasemi A, Hosseinimehr SJ. Radioprotective effect of atorvastatin against ionizing radiation-induced nephrotoxicity in mice. Int J Radiat Biol. 2018. https://doi.org/10.1080/09553002.2018.1420926.
Yu H, Sun SQ, Gu XB, Wang W, Gao XS. Atorvastatin prolongs the lifespan of radiation-induced reactive oxygen species in PC-3 prostate cancer cells to enhance the cell killing effect. Oncol Rep. 2017. https://doi.org/10.3892/or.2017.5447.
Freeberg MAT, Easa A, Lillis JA, Benoit DSW, van Wijnen AJ, Awad HA. Transcriptomic analysis of cellular pathways in healing flexor tendons of plasminogen activator inhibitor 1 (PAI-1/Serpine1) null mice. J Orthop Res. 2020. https://doi.org/10.1002/jor.24448.
Guo B, Inoki K, Isono M, Mori H, Kanasaki K, Sugimoto T, Akiba S, Sato T, Yang B, Kikkawa R, Kashiwagi A, Haneda M, Koya D. MAPK/AP-1-dependent regulation of PAI-1 gene expression by TGF-beta in rat mesangial cells. Kidney Int. 2005. https://doi.org/10.1111/j.1523-1755.2005.00491.x.
Kwak SH, Wang XQ, He Q, Fang WF, Mitra S, Bdeir K, Ploplis VA, Xu Z, Idell S, Cines D, Abraham E. Plasminogen activator inhibitor-1 potentiates LPS-induced neutrophil activation through a JNK-mediated pathway. Thromb Haemost. 2006;95:829–35.
Nakajima K, Yamamoto S, Tohyama Y, Kohsaka S. Close association of p38 and JNK with plasminogen-dependent upregulation of PAI-1 in rat astrocytes in vitro. Neurosci Lett. 2010. https://doi.org/10.1016/j.neulet.2010.01.007.
Paris F, Fuks Z, Kang A, Capodieci P, Juan G, Ehleiter D, Haimovitz-Friedman A, Cordon-Cardo C, Kolesnick R. Endothelial apoptosis as the primary lesion initiating intestinal radiation damage in mice. Science. 2001. https://doi.org/10.1126/science.1060191.
Pontrelli P, Ranieri E, Ursi M, Ghosh-Choudhury G, Gesualdo L, Paolo Schena F, Grandaliano G. jun-N-terminal kinase regulates thrombin-induced PAI-1 gene expression in proximal tubular epithelial cells. Kidney Int. 2004. https://doi.org/10.1111/j.1523-1755.2004.00644.x.
Vulin AI, Stanley FM. Oxidative stress activates the plasminogen activator inhibitor type 1 (PAI-1) promoter through an AP-1 response element and cooperates with insulin for additive effects on PAI-1 transcription. J Biol Chem. 2004. https://doi.org/10.1074/jbc.M403184200.
Wang HC, Lin YL, Hsu CC, Chao YJ, Hou YC, Chiu TJ, Huang PH, Tang MJ, Chen LT, Shan YS. Pancreatic stellate cells activated by mutant KRAS-mediated PAI-1 upregulation foster pancreatic cancer progression via IL-8. Theranostics. 2019. https://doi.org/10.7150/thno.36830.
Kwak SY, Park S, Kim H, Lee SJ, Jang WS, Kim MJ, Lee S, Jang WI, Kim AR, Kim EH, Shim S, Jang H. Atorvastatin inhibits endothelial PAI-1-mediated monocyte migration and alleviates radiation-induced enteropathy. Int J Mol Sci. 2021. https://doi.org/10.3390/ijms22041828.
Ajamieh H, Farrell G, Wong HJ, Yu J, Chu E, Chen J, Teoh N. Atorvastatin protects obese mice against hepatic ischemia-reperfusion injury by toll-like receptor-4 suppression and endothelial nitric oxide synthase activation. J Gastroenterol Hepatol. 2012. https://doi.org/10.1111/j.1440-1746.2012.07123.x.
Ghasemi A, Ghashghai Z, Akbari J, Yazdani-Charati J, Salehifar E, Hosseinimehr SJ. Topical atorvastatin 1% for prevention of skin toxicity in patients receiving radiation therapy for breast cancer: a randomized, double-blind, placebo-controlled trial. Eur J Clin Pharmacol. 2019. https://doi.org/10.1007/s00228-018-2570-x.
Jenrow KA, Liu J, Brown SL, Kolozsvary A, Lapanowski K, Kim JH. Combined atorvastatin and ramipril mitigate radiation-induced impairment of dentate gyrus neurogenesis. J Neurooncol. 2011. https://doi.org/10.1007/s11060-010-0282-x.
Checker R, Patwardhan RS, Jayakumar S, Maurya DK, Bandekar M, Sharma D, Sandur SK. Chemical and biological basis for development of novel radioprotective drugs for cancer therapy. Free Radic Res. 2021. https://doi.org/10.1080/10715762.2021.1876854.
Schleicher SM, Moretti L, Varki V, Lu B. Progress in the unraveling of the endoplasmic reticulum stress/autophagy pathway and cancer: implications for future therapeutic approaches. Drug Resist Updat. 2010. https://doi.org/10.1016/j.drup.2010.04.002.
Chan KK, Oza AM, Siu LL. The statins as anticancer agents. Clin Cancer Res. 2003;9:10–9.
Sassano A, Platanias LC. Statins in tumor suppression. Cancer Lett. 2008. https://doi.org/10.1016/j.canlet.2007.11.036.
Apel A, Herr I, Schwarz H, Rodemann HP, Mayer A. Blocked autophagy sensitizes resistant carcinoma cells to radiation therapy. Cancer Res. 2008. https://doi.org/10.1158/0008-5472.CAN-07-0562.
He Z, Mangala LS, Theriot CA, Rohde LH, Wu H, Zhang Y. Cell killing and radiosensitizing effects of atorvastatin in PC3 prostate cancer cells. J Radiat Res. 2012. https://doi.org/10.1269/jrr.11114.
Hennessey D, Martin LM, Atzberger A, Lynch TH, Hollywood D, Marignol L. Exposure to hypoxia following irradiation increases radioresistance in prostate cancer cells. Urol Oncol. 2013. https://doi.org/10.1016/j.urolonc.2011.10.008.
Chen B, Zhang M, Xing D, Feng Y. Atorvastatin enhances radiosensitivity in hypoxia-induced prostate cancer cells related with HIF-1α inhibition. 2017. Biosci Rep. https://doi.org/10.1042/BSR20170340.
Ricco N, Flor A, Wolfgeher D, Efimova EV, Ramamurthy A, Appelbe OK, Brinkman J, Truman AW, Spiotto MT, Kron SJ. Mevalonate pathway activity as a determinant of radiation sensitivity in head and neck cancer. Mol Oncol. 2019. https://doi.org/10.1002/1878-0261.12535.
He Z, Xu D, Shen F, Zeng F, Qi P, Zhai Z, Wang Z. Atorvastatin enhances inhibitory effects of irradiation on tumor growth by reducing MSH2 expression both in prostate cancer cells and xenograft tumor models. Anticancer Agents Med Chem. 2022. https://doi.org/10.2174/1871520621666210602133005.
Ding N, Cui XX, Gao Z, Huang H, Wei X, Du Z, Lin Y, Shih WJ, Rabson AB, Conney AH, Hu C, Zheng X. A triple combination of atorvastatin, celecoxib and tipifarnib strongly inhibits pancreatic cancer cells and xenograft pancreatic tumors. Int J Oncol. 2014. https://doi.org/10.3892/ijo.2014.2350.
Lehman TA, Modali R, Boukamp P, Stanek J, Bennett WP, Welsh JA, Metcalf RA, Stampfer MR, Fusenig N, Rogan EM, et al. p53 mutations in human immortalized epithelial cell lines. Carcinogenesis. 1993. https://doi.org/10.1093/carcin/14.5.833.
Cauley JA, McTiernan A, Rodabough RJ, LaCroix A, Bauer DC, Margolis KL, Paskett ED, Vitolins MZ, Furberg CD, Chlebowski RT; Women's Health Initiative Research Group (2006) Statin use and breast cancer: prospective results from the Women's Health Initiative. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djj188
Ali A, Levantini E, Fhu CW, Teo JT, Clohessy JG, Goggi JL, Wu CS, Chen L, Chin TM, Tenen DG. CAV1 - GLUT3 signaling is important for cellular energy and can be targeted by Atorvastatin in non-small cell lung cancer. Theranostics. 2019. https://doi.org/10.7150/thno.35805.
Otahal A, Aydemir D, Tomasich E, Minichsdorfer C. Delineation of cell death mechanisms induced by synergistic effects of statins and erlotinib in non-small cell lung cancer cell (NSCLC) lines. Sci Rep. 2020. https://doi.org/10.1038/s41598-020-57707-2.
Wang H, Sun N, Li X, Li K, Tian J, Li J. Simvastatin suppresses cell migration and invasion, induces G0/G1 cell cycle arrest and apoptosis in osteosarcoma cells. Int J Clin Exp Pathol. 2016;9(6):5837–48.
Wolfe AR, Debeb BG, Lacerda L, Larson R, Bambhroliya A, Huang X, Bertucci F, Finetti P, Birnbaum D, Van Laere S, Diagaradjan P, Ruffell B, Trenton NJ, Chu K, Hittelman W, Diehl M, Levental I, Ueno NT, Woodward WA. Simvastatin prevents triple-negative breast cancer metastasis in pre-clinical models through regulation of FOXO3a. Breast Cancer Res Treat. 2015. https://doi.org/10.1007/s10549-015-3645-3.
Li J, Liu J, Liang Z, He F, Yang L, Li P, Jiang Y, Wang B, Zhou C, Wang Y, Ren Y, Yang J, Zhang J, Luo Z, Vaziri C, Liu P. Simvastatin and Atorvastatin inhibit DNA replication licensing factor MCM7 and effectively suppress RB-deficient tumors growth. Cell Death Dis. 2017. https://doi.org/10.1038/cddis.2017.46.
Zhou M, Zheng J, Bi J, Wu X, Lyu J, Gao K. Synergistic inhibition of colon cancer cell growth by a combination of atorvastatin and phloretin. Oncol Lett. 2018. https://doi.org/10.3892/ol.2017.7480.
Terzi H, Altun A, Şencan M. In vitro comparison of the cytotoxic effects of statins on U266 myeloma cell line. Indian J Med Res. 2019. https://doi.org/10.4103/ijmr.IJMR_672_18.
Göbel A, Breining D, Rauner M, Hofbauer LC, Rachner TD. Induction of 3-hydroxy-3-methylglutaryl-CoA reductase mediates statin resistance in breast cancer cells. Cell Death Dis. 2019. https://doi.org/10.1038/s41419-019-1322-x.
Yang Z, Xiao H, Jin H, Koo PT, Tsang DJ, Yang CS. Synergistic actions of atorvastatin with gamma-tocotrienol and celecoxib against human colon cancer HT29 and HCT116 cells. Int J Cancer. 2010. https://doi.org/10.1002/ijc.24766.
Kumar VL, Guruprasad B, Wahane VD. Atorvastatin exhibits anti-inflammatory and anti-oxidant properties in adjuvant-induced monoarthritis. Inflammopharmacology. 2010. https://doi.org/10.1007/s10787-010-0057-1.
Farsaei S, Khalili H, Farboud ES. Potential role of statins on wound healing: review of the literature. Int Wound J. 2012. https://doi.org/10.1111/j.1742-481X.2011.00888.x.
Kurçer Z, Özbakiş-Dengiz G, Füsun B, Banoğlu ZN (2017) Statinlerin Testiküler İskemi Reperfüzyon ile Oluşturulan Histopatolojik Hasar Üzerine Etkileri
Marková I, Malínská H, Hüttl M, Miklánková D, Oliyarnyk O, Poruba M, Rácová Z, Kazdová L, Večeřa R. The combination of atorvastatin with silymarin enhances hypolipidemic, antioxidant and anti-inflammatory effects in a rat model of metabolic syndrome. Physiol Res. 2021. https://doi.org/10.33549/physiolres.934587.
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shaghaghi, Z., Alvandi, M., Farzipour, S. et al. A review of effects of atorvastatin in cancer therapy. Med Oncol 40, 27 (2023). https://doi.org/10.1007/s12032-022-01892-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-022-01892-9