Abstract
Afatinib, a second-generation epidermal growth factor receptor (EGFR)—tyrosine kinase inhibitor (TKI) for mutant non-small cell lung cancer (NSCLC), was approved in Japan in 2014. This study evaluated clinical outcomes of afatinib in real-world practice. Medical records of patients who received afatinib for advanced EGFR-mutant NSCLC were retrospectively reviewed. In total, 128 patients were analyzed. Seventy-six patients received afatinib as the first-line setting and 52 as the re-challenge setting (i.e., after failure of prior first-generation TKI). There was no difference in patient characteristics, such as age, sex, and PS, between the first-line and the re-challenge settings. In the first-line setting, the median progression-free survival (PFS) was 17.8 months (95% confidence interval [CI] 13.7–21.5 months). The overall survival (OS) was 39.5 months (95% CI 34.4- not reached). The response rate (RR) was 64.4%. Subset analysis indicated that patients with dose reduction showed longer PFS than those without dose reduction (18.5 months versus 7.9 months) (P = 0.016). In the re-challenge setting, the median PFS was 8.0 months (95% CI 4.9–9.5 months). The RR was 25%. Most common adverse events leading to dose modification or treatment discontinuation included diarrhea, paronychia, and oral mucositis in both settings. Interstitial lung disease occurred in 5.4% (7/128). In the real-world practice in Japan, afatinib showed comparable or better efficacy compared with that shown in previous clinical trials in both the first-line and the re-challenge settings.
Similar content being viewed by others
Introduction
Lung cancer is one of the most common malignancies in the world, with non-small cell lung cancer (NSCLC) accounting for 85% [1]. Currently, the most established target is the epidermal growth factor receptor (EGFR), a member of the ErbB kinase family of structurally related receptor tyrosine kinases. In human, the ErbB family consists of EGFR (HER1, ErbB1), HER2 (ErbB2), HER3 (ErbB3), and HER4 (ErbB4) [2]. The prevalence of EGFR mutation is 50% in Asian patients with NSCLC [3].
NSCLC with EGFR mutations is recommended to treat with molecular target therapy with EGFR-tyrosine kinase inhibitors (TKIs) [4,5,6,7,8]. Recently, a phase III FLAURA trial revealed that osimertinib has better progression-free survival (PFS) than the first-generation EGFR-TKIs (gefitinib and elrotinib) [9]. Afatinib, a second-generation EGFR-TKI, irreversibly blocks signaling through not only EGFR but also HER2 and ErbB4 [10, 11]. In two pivotal phase III studies, afatinib showed better PFS than standard platinum-based chemotherapy [8, 12]. In subgroup analysis of Lux-lung 3 and Lux-lung 6 trials, afatinib provided a better overall survival (OS) benefit than standard chemotherapy [12]. The OS benefit with afatinib could be associated with its potential advantages in targeting the entire ErbB family rather than EGFR alone. In addition, Lux-lung 7 study revealed that afatinib might offer improved PFS compared with gefitinib [13].
Preclinical data suggested that afatinib is more active than first-generation EGFR-TKIs in NSCLC that acquired resistance to gefitinib or erlotinib [14]. Lux-lung 1 study, which examined the efficacy of afatinib in a re-challenge setting, did not show significant improvement in the OS, although the EGFR mutation status of the study subjects was not shown [15]. The efficacy of re-challenge treatment with afatinib for patients with EGFR-mutated metastatic NSCLC previously responsive to first-generation TKIs has not been clear. Here, we report a real-world data of afatinib in first-line or re-challenge settings for Japanese patients with EGFR mutant NSCLC.
Patients and methods
Study design
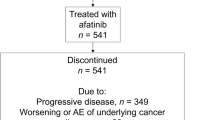
This study was a multicenter retrospective study involving 5 institutions in Aomori, Japan. We reviewed medical records of all the patients who were treated with afatinib at the participating hospitals. In the first-line setting, chemo-naïve patients were screened. In the re-challenge setting, patients who had disease progression or discontinuation due to toxicity for at least one of first-generation TKIs were included. Because, in Japan, osimertinib was approved for NSCLC patients with T790 M mutation in May 2016, we excluded the patients who were diagnosed as NSCLC with T790 M mutation after May 2016. The study was performed according to the protocol approved by the ethics committee of each participating hospital. Institutional Review Board of Hirosaki University approved this study (approval number: 2016-1108). Because this was a retrospective cohort study, informed consent was waived. Opt out was done on the web site of Hirosaki University.
Evaluation and statistical analysis
All analyses were performed using JMP 13 (SAS Institute, Cary, NC, USA). PFS and OS were estimated using the Kaplan–Meier method. PFS has been defined as the time from the date of treatment initiation to the date of disease progression, death, or the last contact. If either event was not observed, survival event was considered to be censored with the latest observation date. If post-treatment is started, survival event was considered to be censored with the date of initiation of the next line chemotherapy. OS was defined as the time from the treatment initiation to any death. Tumor responses were assessed using chest computed tomographic scan. Unidirectional measurements were adopted on the basis of the Response Evaluation Criteria in Solid Tumors (RECIST), version 1.1. The adverse events (AEs) were graded using National Cancer Institute Common Toxicity Criteria Version 4.0. Differences were assumed to be significant when a P value of < 0.05 was achieved.
Results
Patient characteristics
From October 2014 to January 2017, a total of 128 patients were screened from 5 participating institutions in Aomori, Japan. Seventy-six patients received afatinib in the first-line setting (the first-line group) and 52 in the re-challenge setting (the re-challenge group). Table 1 showed the characteristics of the eligible patients.
In the first-line group, the median age was 68 years (range, 42–88 years), and 52 patients (68.4%) were under 75 years. There were 52 female patients (68.4%). The number of patients with a performance status (PS) 0–1 was 67 (88.1%). Only 3 (3.9%) patients had poor PS (3–4). Seventy-four patients (97.4%) had adenocarcinoma histology. Only one patient (1.3%) had squamous cell carcinoma, and another patient (1.3%) had NSCLC not otherwise specified (NOS). Nine patients (11.8%) had stage IIIB, 45 (59.3%) had stage IV, and 22 (28.9%) had recurrent disease. The EGFR mutation status was as follows: exon 19 deletion/exon 21 L858R/exon 18 G719X in 46/28/2, respectively.
In the re-challenge group, the median age was 65 years (range, 39–90 years), and 41 patients (78.9%) were female sex. Most patients (88.4%) had PS 0–1. The EGFR mutation status was as follows: exon 19 deletion/exon 21 L858R/exon 18 G719X in 29/21/2, respectively. Gefitinib was used most frequently as the previous treatment. Thirty-eight patients (73.1%) received afatinib as the 3rd or later line treatment. On the other hand, 14 patients (26.9%) were treated as the second line. In the second line setting, twelve (85.7%) discontinued the prior EGFR-TKI treatment due to its toxicity.
Efficacy
-
The response to afatinib treatment in the first-line setting is summarized in Table 2. One patient achieved complete response (CR) and 48 patients attained a partial response (PR). The ORR was 64.4%. Sixteen patients (34.3%) had stable disease (SD). The median PFS was 17.8 months (95% confidence interval [CI] 13.7–21.5) (Fig. 1a). The OS was 39.5 months (95% CI 34.4- not reached) (Fig. 1b). We conducted additional subgroup analysis about relationship between patient characteristics and survival outcome. There was no difference in median PFS and OS according to age (≤ 74 or 75 ≤) (Supplementary Fig. 1). The ORR was 74.9% in elderly group. One patient CR and 17 patients attained a PR. Fifty-eight patients (76.3%) received reduced dose of afatinib due to adverse events. However, dose reduction did not affect its efficacy in terms of OS (39.5 months in the patients with dose reduction vs. not yet reached in those without, P = 0.37). Moreover, the patients with dose reduction showed even longer PFS than those without (18.5 months and 7.9 months, respectively) (P = 0.018) (Fig. 1c). There was no difference in median PFS and OS between the patients with exon 19 deletion and those with exon 21 L858R mutation (Supplementary Fig. 2). There were two patients with minor mutation in the first-line setting. One patient had PR and the other had SD. The PFS was 7.8 months in these two patients.
In the re-challenge setting, 1 patient had CR and 12 attained PR. The RR was 25%, and 29 patients (55.9%) had SD (Table 2). The median PFS was 8.0 months (95% CI 4.9–9.5) (Fig. 2). There was no difference in median PFS according to mutation status or prior TKI regimen. In second line setting, there were twelve (85.7%) of 14 patients who discontinued the prior EGFR-TKI treatment due to its toxicity. We conducted additional analysis of ORR and PFS of 12 patients excluded. The ORR was 22%, and the median PFS was 5.7 months (95% CI 3.3–7.6) (Supplementary Fig. 3).
T790 M status after first-line afatinib
Forty-eight patients had progressive disease (PD) at the time of analysis, 28 patients underwent re-biopsy. Sixteen patients (57.1%) were positive of T790 M after the first-line afatinib treatment. The OS data of T790 M positive cases was 42.3 months (95% CI 26.9–42.5) (Supplementary Fig. 4).
Toxicity analysis
The major toxicities in both settings are shown in Table 3. Most of the patients who received afatinib needed dose reduction. The primary reasons for dose reduction included diarrhea, paronychia, and oral mucositis. Grade 3 or higher hematologic toxicities observed were anemia (5.2%) in the first-line setting and neutropenia (3.8%) and anemia (3.9%) in the re-challenge setting. Grade 3 non-hematologic toxicities observed frequently included skin rush (11.8%), anorexia (14.4%), and diarrhea (7.8%) in the first-line setting and, rush (4.3%), anorexia (7.6%), diarrhea (13.4%) in the re-challenge setting. Grade 1 or 2 non-hematologic toxicities were fatigue, paronychia, oral mucositis, abnormal liver dysfunction and infection, which were generally mild and reversible. Interstitial lung disease (ILD) was observed in 7 patients (5.7%). There was no grade 4 or 5 ILD in this study.
Discussion
This is one of the largest real-world studies that evaluated the efficacy of afatinib for patients with advanced NSCLC harboring EGFR mutations in both the first-line and the re-challenge settings. In the first-line setting, we revealed afatinib provided PFS of 17.8 months and OS of 39.5 months, which were longer than the numbers shown in Lux-lung 3 (11.1 months and 33.3 months, respectively), Lux-lung 6 (11.0 months and 31.4 months, respectively), and Lux-lung 7 (11.0 months and 27.9 months, respectively) studies [8, 13, 16]. Recently, Liang and colleagues evaluated the real-world efficacy of afatinib in patients with EGFR mutations in Taiwan and reported that median PFS and OS were 12.8 and 36.7 months, respectively [17]. Although the OS was close to our data, the PFS was longer.
A third-generation EGFR-TKI, osimertinib, has recently been compared with gefitinib or erlotinib in the global phase III FLAURA trial [9]. The median PFS was 18.9 months in the osimertinib arm, although OS data are currently immature. However, second-generation EGFR-TKIs were not included in the comparator arm, which made it difficult to draw conclusions regarding potential benefits of osimertinib over afatinib or dacomitinib in the first-line setting. In our study, the PFS data were comparable to that of osmertinib shown in the FLAURA trial. Moreover, in an observational study, Hochmair and colleagues reported long OS outcome in patients with EGFR mutation-positive NSCLC receiving sequential afatinib and osimertinib, especially in those with exon 19 deletion (30.3 months [90% CI 27.6–44.5]) or Asian (46.7 months [90% CI 26.8-not reached]) [18]. They suggested that first-line afatinib followed by osimertinib in patients with NSCLC who acquire T790 M might be a feasible therapy.
In our study, which included elderly patients (31.6%), there were no differences in median PFS and OS between younger patients and elderly. There have been a few reports that prospectively evaluated the efficacy and safety profile of afatinib in the elderly patients. Imai and colleagues recently reported the first study of afatinib (30 mg/day) for the elderly (70 ≤) patients harboring sensitive EGFR mutations. The median PFS was 12.9 months [19]. Our data of the PFS in elderly were 15.4 months. Paz-Ares and colleagues reported that there was no difference in OS among patient subgroups and that similar median OS was seen at cutoffs of 60, 65, 70, and 75 years old [13, 20]. Moreover, we previously reported the phase I trial of afatinib for elderly patients (75 ≤). Although dose reduction rate of afatinib was high, the response rate was as high as 73.3% and PFS was 22 months (95% CI 13.1- not reached) [21].
The most frequent drug-related AEs in the current study were diarrhea, rash, paronychia, and oral mucositis, which were main reasons for the dose modification. However, the dose reduction did not affect the efficacy of afatinib. Preferably, the patients with dose reduction showed even longer PFS than those without dose reduction. In our study, interstitial lung disease was observed in 5.7%, which was similar to the numbers in previous reports [21].
In the present study, two patients with G719X, one of minor mutations of EGFR gene, were included and their median PFS was 7.8 months, although the sample size was too small to discuss the efficacy of afatinib for NSCLC with minor mutations. EGFR mutations G719X and L861Q are found in approximately 3% and 2% in NSCLC with EGFR mutation, respectively [22]. In a retrospective study that included 16 patients with minor mutations, first-generation EGFR-TKIs provided the median PFS of 1.5 months and the RR of 25.0% [23]. Yang and colleagues reported the efficacy of afatinib in 38 patients with advanced NSCLC harboring minor mutations. The RR was 71.1%, and the median PFS and OS were 10.7 and 18.6 months, respectively [24]. These data suggest that, in NSCLC patients with minor mutations, afatinib may have greater efficacy than first-generation EGFR-TKIs.
In the re-challenge setting, the RR was 25%, and 29 patients (55.9%) had SD. The median PFS was 8.0 months (95% CI 4.9–9.5). We summarized 4 prospective studies and 1 retrospective study that evaluated the efficacy of afatinib on NSCLC patients in whom prior EGFR-TKIs failed (Table 4). The Lux-lung 1 investigated the efficacy of afatinib in patients who had PD after first-generation EGFR-TKI, which showed improvement of a median PFS in those treated with afatinib without improvement in the OS. EGFR mutation status was not evaluated in the Lux-lung 1 study [25]. Lux-lung 4 study was a phase II trial in Japan, which evaluated the efficacy of afatinib monotherapy as the in third- or fourth-line treatment in patients with NSCLC who had PD while receiving erlotinib and/or gefitinib treatment. The ORR was 8.2%, which did not meet the primary endpoint, and the median PFS was 4.4 months [26]. In another prospective study, Lee and colleagues reported afatinib might offer improved PFS and ORR compared with erlotinib in Chinese patients [27]. Other studies also showed that afatinib provided approximately 4 months of PFS [28, 29]. Our study showed better PFS compared to these previous reports.
In our study, 14 patients (26.9%) received afatinib as the second line treatment. Twelve patients (85.7%) of them discontinued prior EGFR-TKI treatment due to toxicity, which might be one of the main reasons for their long PFS.
Chemotherapy has been a common option for the patients who had PD for EGFR-TKI. In the previous clinical trials, ORR ranged about 8.8–22.9% and median PFS was 2.9–4.5 months for patients who received chemotherapy [30, 31]. The hematologic adverse effects were more common in chemotherapy. Considering the efficacy and toxicity, afatinib could be a treatment choice as salvage therapy.
In our clinical practice, osimertinib has been used in the first-line treatment for EGFR mutant NSCLC. The efficacy data of the first- or second-generation EGFR-TKIs for patients with T790 M negative NSCLC who had PD after osimertinib is needed.
The present study has some limitations. First, because our study was retrospective, the schedule of image inspection of tumor was not determined, which might affect the PFS estimation. Second, efficacy measurements were not taken by central review but by each investigator. Finally, as we collected the data before approval of osimertinib in Japan, T790 M mutation was not examined. Since T790 M positive patients are currently treated with osimertinib, re-challenge data in patients with T790 M negative NSCLC will be required.
Conclusions
In conclusion, afatinib showed a manageable safety profile and comparable or better efficacy in real-world practice in both the first-line and the re-challenge settings compared with those described in previous reports. Dose reduction or age factor did not affect the efficacy of afatinib.
Abbreviations
- NSCLC:
-
Non–small cell lung cancer
- EGFR:
-
Epidermal growth factor receptor
- TKIs:
-
Tyrosine kinase inhibitors
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- IRB:
-
Institutional review board
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- AEs:
-
Adverse events
- PS:
-
Performance status
- NOS:
-
Not otherwise specified
- CR:
-
Complete response
- PR:
-
Partial response
- SD:
-
Stable disease
- CI:
-
Confidence interval
- PD:
-
Progressive disease
- ILD:
-
Interstitial lung disease
References
Siegel R, Naishadham D, Jemal A. Cancer statistics 2012. CA Cancer J Clin. 2012;62:10–29.
Roskoski R Jr. The ErbB/HER family of proteintyrosine kinases and cancer. Pharmacol Res. 2014;79:34–74.
Shi Y, Au JS, Thongprasert S, et al. A prospective, molecular epidemiology study of EGFR mutations in Asian patients with advanced non-small-cell lung cancer of adenocarcinoma histology (PIONEER). J Thorac Oncol. 2014;9:154–62.
Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362:2380–8.
Mitsudomi T, Morita S, Yatabe Y, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010;11:121–8.
Zhou C, Wu YL, Chen G, et al. Erlotinib versus chemotherapy as frst-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12:735–42.
Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13:239–46.
Wu YL, Zhou C, Hu CP, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15:213–22.
Soria JC, Ohe Y, Vansteenkiste J, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2018;378:113–25.
Hynes NE, Lane HA. ERBB receptors and cancer: the complexity of targeted inhibitors. Nat Rev Cancer. 2005;5:341–54.
Li D, Ambrogio L, Shimamura T, et al. BIBW2992, an irreversible EGFR/HER2 inhibitor highly effective in preclinical lung cancer models. Oncogene. 2008;27:4702–11.
Yang JC, Wu YL, Schuler M, et al. Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6): analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol. 2015;16:141–51.
Paz-Ares L, Tan EH, O’Byrne K, et al. Afatinib versus gefitinib in patients with EGFR mutation-positive advanced non-small-cell lung cancer: overall survival data from the phase IIb LUX-Lung 7 trial. Ann Oncol. 2017;28:270–7.
Solca F, Dahl G, Zoephel A, et al. Target binding properties and cellular activity of afatinib (BIBW 2992), an irreversible ErbB family blocker. J Pharmacol Exp Ther. 2012;343:342–50.
Miller VA, Hirsh V, Cadranel J, et al. Afatinib versus placebo in patients with advanced, metastatic non-small-cell lung cancer after failure of erlotinib, gefitinib, or both, and one or two lines of chemotherapy (LUX-Lung1): a phase 2b/3 randomised trial. Lancet Oncol. 2012;13:528–38.
Sequist LV, Yang JC, Yamamoto N, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol. 2013;31:3327–34.
Liang SK, Lee MR, Liao WY, et al. Prognostic factors of afatinib as a first-line therapy for advanced EGFR mutation-positive lung adenocarcinoma: a real-world, large cohort study. Oncotarget. 2018;9:23749–60.
Hochmair MJ, Morabito A, Hao D, et al. Sequential treatment with afatinib and osimertinib in patients with EGFR mutation-positive non-small-cell lung cancer: an observational study. Future Oncol. 2018;14:2861–74.
Imai H, Kaira K, Suzuki K, et al. A phase II study of afatinib treatment for elderly patients with previously untreated advanced non-small-cell lung cancer harboring EGFR mutations. Lung Cancer. 2018;126:41–7.
Liu CY, Wang CL, Li SH, et al. The efficacy of 40 mg versus dose de-escalation to less than 40 mg of afatinib (Giotrif) as the first-line therapy for patients with primary lung adenocarcinoma harboring favorable epidermal growth factor mutations. Oncotarget. 2017;8:97602–12.
Tanaka H, Taima K, Tanaka Y, Itoga M, Ishioka Y, et al. A phase I study of afatinib for patients aged 75 or older with advanced non-small cell lung cancer harboring EGFR mutations. Med Oncol. 2018;35:34.
Murray S, Dahabreh IJ, Linardou H, et al. Somatic mutations of the tyrosine kinase domain of epidermal growth factor receptor and tyrosine kinase inhibitor response to TKIs in non-small cell lung cancer: an analytical database. J Thorac Oncol. 2008;3:832–9.
Watanabe S, Minegishi Y, Yoshizawa H, et al. Effectiveness of gefitinib against non-small-cell lung cancer with the uncommon EGFR mutations G719X and L861Q. J Thorac Oncol. 2014;9:189–94.
Yang JC, Sequist LV, Geater SL, et al. Clinical activity of afatinib in patients with advanced non-small-cell lung cancer harbouring uncommon EGFR mutations: a combined post hoc analysis of LUX-Lung 2, LUX-Lung 3, and LUX-Lung 6. Lancet Oncol. 2015;16:830–8.
Miller VA, Hirsh V, Cadranel J, et al. Afatinib versus placebo for patients with advanced, metastatic non-small-cell lung cancer after failure of erlotinib, gefitinib, or both, and one or two lines of chemotherapy (LUX-Lung 1): a phase 2b/3 randomised trial. Lancet Oncol. 2012;13:528–38.
Katakami N, Atagi S, Goto K, et al. LUX-Lung 4: a phase II trial of afatinib in patients with advanced non-small-cell lung cancer who progressed during prior treatment with erlotinib, gefitinib, or both. J Clin Oncol. 2013;31:3335–41.
Lee VH, Leung DK, Choy TS, et al. Efficacy and safety of afatinib in Chinese patients with EGFR-mutated metastatic non-small-cell lung cancer (NSCLC) previously responsive to first-generation tyrosine-kinase inhibitors (TKI) and chemotherapy: comparison with historical cohort using erlotinib. BMC Cancer. 2016;16:147.
Chang GC, Tseng CH, Hsu KH, et al. Predictive factors for EGFR-tyrosine kinase inhibitor retreatment in patients with EGFR-mutated non-small-cell lung cancer—a multicenter retrospective SEQUENCE study. Lung Cancer. 2017;104:58–64.
Schuler M, Yang JC, Park K, et al. Afatinib beyond progression in patients with non-small-cell lung cancer following chemotherapy, erlotinib/gefitinib and afatinib: phase III randomized LUX-Lung 5 trial. Ann Oncol. 2016;27:417–23.
Hanna N, Shepherd FA, Fossella FV, et al. Randomized phase III trial of pemetrexed versus docetaxel in patients with non-small-cell lung cancer previously treated with chemotherapy. J Clin Oncol. 2004;22:1589–97.
Garon EB, Ciuleanu TE, Arrieta O, et al. Ramucirumab plus docetaxel versus placebo plus docetaxel for second-line treatment of stage IV non-small-cell lung cancer after disease progression on platinum-based therapy (REVEL): a multicentre, double-blind, randomised phase 3 trial. Lancet. 2014;384:665–73.
Acknowledgements
The authors are grateful to the patients and their family and medical staffs who contributed to this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
HT and KT prepared the manuscript and the literature search; HT and MI conducted statistical analysis; YI, KB, TS, HS and JT contribute to treated and observed patients in Hirosaki University; HN treated and observed patients in Hirosaki National Hospital; YH treated and observed patients in Aomori Prefectural Central Hospital; HY treated and observed patients in Hachinohe City Hospital; KO treated and observed patients in Hirosaki Central Hospital; ST and ST reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declared that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the institutional review boards of all participating institutions. (approval number: 2016-1108).
Informed consent
Because this was a retrospective cohort study, informed consent was waived. Opt out was done on the web site of Hirosaki University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12032_2019_1278_MOESM1_ESM.pdf
Supplementary material 1 (PDF 424 kb). Supplementary Fig. 1 Additional sub group analysis between patient characteristics and survival outcome in first-line setting. There was no difference in median progression-free survival and overall survival according to age (< 74, 75 ≦)
12032_2019_1278_MOESM2_ESM.pdf
Supplementary material 2 (PDF 409 kb). Supplementary Fig. 2 Additional sub group analysis between patient characteristics and survival outcome in first-line setting. There was no difference in median progression-free survival and overall survival according to between exon19 del and exon21 L858R
12032_2019_1278_MOESM3_ESM.pdf
Supplementary material 3 (PDF 402 kb). Supplementary Fig. 3 Kaplan-Meier analysis of progression-free survival in the re-challenge setting excluded 12 patients who discontinued the prior EGFR-TKI treatment due to its toxicity. The median PFS was 5.7 months
12032_2019_1278_MOESM4_ESM.pdf
Supplementary material 4 (PDF 393 kb). Supplementary Fig. 4 Kaplan-Meier analysis of overall survival of patients with T790M positive cases in the first-line setting. The overall survival was 42.3 months
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Tanaka, H., Taima, K., Itoga, M. et al. Real-world study of afatinib in first-line or re-challenge settings for patients with EGFR mutant non-small cell lung cancer. Med Oncol 36, 57 (2019). https://doi.org/10.1007/s12032-019-1278-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-019-1278-9