Abstract
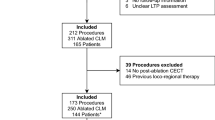
A standardized cone beam computed tomography (CBCT) protocol may impact optimal ablation probe(s) positioning during ultrasound-guided microwave ablation (MWA). To evaluate this hypothesis, 15 patients underwent ultrasound-guided percutaneous MWA of 15 liver lesions (10 hepatocellular carcinomas, 5 metastasis ranging 11–41 mm) with the ultrasound guidance assisted by a dedicated CBCT protocol. Pre-procedural enhanced CBCT (ceCBCT) was performed after intravenous contrast administration to visualize the lesion and determine the optimal approach using CBCT-based ablation planning software. MW antennas were positioned under ultrasound guidance, and non-enhanced CBCT was performed after deployment and fused with pre-procedural ceCBCT to assess tumor targeting and modify subsequent steps of the procedure. CBCT lesion detection accuracy and number of needle repositioning on the basis of CBCT information were recorded. Clinical success was measured on 1-month follow-up contrast-enhanced CT. The target lesion was detected on ceCBCT in 13 out of 15 patients (87%). The undetected lesions were only visible on diagnostic contrast-enhanced magnetic resonance imaging, which was then fused to the CBCT and fluoroscopy to facilitate targeting. MW antennas were repositioned on the basis of CBCT in 11 lesions (73%). Clinical success was achieved in 14/15 ablations (93%) with a mean follow-up of X months. The only case of local recurrence was expected, as the intent was tumor debulking. CBCT imaging during ultrasound-guided liver ablation is feasible and leads to ablation device repositioning in the majority of cases.




Similar content being viewed by others
References
Gervais DA, Goldberg SN, Brown DB, et al. Society of interventional radiology position statement on percutaneous radiofrequency ablation for the treatment of liver tumors. J Vasc Interv Radiol. 2009;20(7 Suppl):S342–7.
Gillams A, Goldberg N, Ahmed M, et al. Thermal ablation of colorectal liver metastases: a position paper by an international panel of ablation experts, the interventional oncology sans frontières meeting 2013. Eur Radiol. 2015;25(12):3438–54.
Scialpi M, Palumbo B, Pierotti L, Gravante S, Piunno A, Rebonato A, Dandrea A, Reginelli A, Piscioli I, Brunese L, Rotondo A. Detection and characterization of focal liver lesions by split-bolus multidetector-row CT: diagnostic accuracy and radiation dose in oncologic patients. Anticancer Res. 2014;34(8):4335–44.
Ahmed M, Solbiati L, Brace CL, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria—a 10-year update. Radiology. 2014;273(1):241–60.
Abi-Jaoudeh N, Kruecker J, Kadoury S, et al. Multimodality image fusion-guided procedures: technique, accuracy, and applications. Cardiovasc Interv Radiol. 2012;35(5):986–98.
Klibanov AL, Hossack JA. Ultrasound in radiology: from anatomic, functional, molecular imaging to drug delivery and image-guided therapy. Invest Radiol. 2015;50(9):657–70.
Orth RC, Wallace MJ, Kuo MD. Technology assessment committee of the society of interventional R C-arm cone-beam CT: general principles and technical considerations for use in interventional radiology. J Vasc Interv Radiol. 2008;19(6):814–20.
Floridi C, Radaelli A, Abi-Jaoudeh N, et al. C-arm cone-beam computed tomography in interventional oncology: technical aspects and clinical applications. Radiol Med. 2014;119(7):521–32.
Ierardi AM, Petrillo M, Xhepa G, et al. Cone beam computed tomography images fusion in predicting lung ablation volumes: a feasibility study. Acta Radiol. 2015;29:188–96.
Cazzato RL, Battistuzzi JB, Catena V, et al. Cone-beam computed tomography (CBCT) versus CT in lung ablation procedure: which is faster? Cardiovasc Interv Radiol. 2015;38:1231–36.
Bapst B, Lagadec M, Breguet R, Vilgrain V, Ronot M. Cone beam computed tomography (CBCT) in the field of interventional oncology of the liver. Cardiovasc Interv Radiol. 2016;39:308–20.
Abi-Jaoudeh N, Venkatesan AM, Van der Sterren W, et al. Clinical experience with cone-beam CT navigation for tumor ablation. J Vasc Interv Radiol. 2015;26(2):214–9.
Toporek G, Wallach D, Weber S, Bale R, Widmann G. Cone-beam computed tomography-guided stereotactic liver punctures: a phantom study. Cardiovasc Interv Radiol. 2013;36(6):1629–37.
Morimoto M, Numata K, Kondo M, et al. C-arm cone beam CT for hepatic tumor ablation under real-time 3D imaging. AJR Am J Roentgenol. 2010;194(5):W452–4.
Schernthaner R, Schernthaner RE, Chapiro J, Sahu S, et al. Feasibility of a modified cone-beam CT rotation trajectory to improve liver periphery visualization during transarterial chemoembolization. Radiology. 2015;277(3):833–41.
Ierardi AM, Mangano A, Floridi C, Dionigi G, Biondi A, Duka E, Lucchina N, Lianos GD, Carrafiello G. A new system of microwave ablation at 2450 MHz: preliminary experience. Updates Surg. 2015;67(1):39–45.
Widmann G, Bodner G, Bale R, et al. Tumour ablation: technical aspects. Cancer Imaging. 2009;9:S63–7.
Phee SJ, Yang K. Interventional navigation systems for treatment of unresectable liver tumor. Med Biol Eng Comput. 2010;48:103–11.
Kikuchi L, Menezes M, Chagas AL, et al. Percutaneous radiofrequency ablation for early hepatocellular carcinoma: risk factors for survival. World J Gastroenterol. 2014;20(6):1585–93.
Rhim H, Lee MH, Kim YS, et al. Planning sonography to assess the feasibility of percutaneous radiofrequency ablation of hepatocellular carcinomas. AJR. 2008;190:1324–30.
Kim PN, Choi D, Rhim H, et al. Planning ultrasound for percutaneous radiofrequency ablation to treat small (≤3 cm) hepatocellular carcinomas detected on computed tomography or magnetic resonance imaging: a multicenter prospective study to assess factors affecting ultrasound visibility. J Vasc Interv Radiol. 2012;23(5):627–34.
Lee MW, Rhim H, Cha DI, et al. Percutaneous radiofrequency ablation of hepatocellular carcinoma: fusion imaging guidance for management of lesions with poor conspicuity at conventional sonography. AJR. 2012;198:1438–44.
Lim S, Lee MW, Rhim H, et al. Mistargeting after fusion imaging-guided percutaneous radiofrequency ablation of hepatocellular carcinomas. JVIR. 2014;25:307–31.
Cazzato RL, Buy X, Alberti N, et al. Flat-panel cone-beam CT-guided radiofrequency ablation of very small (≤1.5 cm) liver tumors: technical note on a preliminary experience. Cardiovasc Interv Radiol. 2015;38(1):206–12.
Iwazawa J, Ohue S, Hashimoto N, Mitani T. Ablation margin assessment of liver tumors with intravenous contrast-enhanced C-arm computed tomography. World J Radiol. 2012;4(3):109–14.
Abdel-Rehim M, Ronot M, Sibert A, Vilgrain V. Assessment of liver ablation using cone beam computed tomography. World J Gastroenterol. 2015;21(2):517–24.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Floridi, C., Radaelli, A., Pesapane, F. et al. Clinical impact of cone beam computed tomography on iterative treatment planning during ultrasound-guided percutaneous ablation of liver malignancies. Med Oncol 34, 113 (2017). https://doi.org/10.1007/s12032-017-0954-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-017-0954-x