Abstract
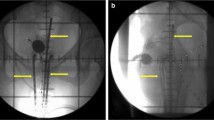
The objective of this study was to compare the effect of combined external beam radiotherapy (EBRT) and Californium (Cf)-252 neutron intracavity brachytherapy (ICBT) on cervical squamous versus adenocarcinoma. A total of 106 patients with stage IB–IIIB cervical cancer were accrued between January 2005 and May 2011 and divided into squamous cell carcinoma (SCC) and adenocarcinoma (AC) as a pair with 53 patients in each group according to tumor size, stage, age, and hemoglobin level using matched-pair design. The whole pelvic EBRT was performed with 2 Gy/fraction, 4 fractions/week. The total dose was 48–54 Gy (the center of whole pelvic field was blocked by 4 cm in width after 20–36 Gy). Cf-252 neutron ICBT was delivered with 11 and 12 Gy-eq/f with the total dose at point A of 44 and 48 Gy-eq for SCC and AC patients, respectively. The mean follow-up time was 43 months. The 5-year LC, OS, DFS, LAC rates, and mean survival time were 66.0, 56.6, 52.8.0, 17.0 %, and 76.4 ± 6.2 months, respectively, for AC patients, whereas they were 81.1, 69.8, 67.9, 11.3 %, and 93.3 ± 4.3 months, respectively, for SCC patients. Furthermore, the early treatment toxicity was mild in both groups, the late treatment complications were mainly radiation-induced proctitis and cystitis, and there were no grade 3 or higher complications. Although the combination of Cf-252 neutron ICBT and EBRT was effective in both histology types of cervical cancer, a more aggressive strategy is needed to control cervical AC.


Similar content being viewed by others
References
Jemal A, et al. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90.
Mathew A, George PS. Trends in incidence and mortality rates of squamous cell carcinoma and adenocarcinoma of cervix–worldwide. Asian Pac J Cancer Prev. 2009;4(10):645–50.
Canavan TP, Doshi NR. Cervical cancer. Am Fam Physician. 2000;61(5):1369–76.
Kumar V et al. Robbins basic pathology, 8th ed. New York: Saunders Elsevier; 2007. pp. 718–721.
Gien LT, Beauchemin MC, Thomas G. Adenocarcinoma: a unique cervical cancer. Gynecol Oncol. 2010;116(1):140–6.
Smith HO, et al. The rising incidence of adenocarcinoma relative to squamous cell carcinoma of the uterine cervix in the United States—a 24-year population-based study. Gynecol Oncol. 2000;78(2):97–105.
Sasieni P, Adams J. Changing rates of adenocarcinoma and adenosquamous carcinoma of the cervix in England. The Lancet. 2001;357(9267):1490–3.
Mabuchi S, et al. Impact of histological subtype on survival of patients with surgically-treated stage IA2-IIB cervical cancer: adenocarcinoma versus squamous cell carcinoma. Gynecol Oncol. 2012;127(1):114–20.
Green JA, et al. Survival and recurrence after concomitant chemotherapy and radiotherapy for cancer of the uterine cervix: a systematic review and meta-analysis. The Lancet. 2001;358(9284):781–6.
Rose PG. Are the differences in treatment outcome for adenocarcinoma of the cervix different enough to change the treatment paradigm? Gynecol Oncol. 2012;125(2):285–6.
Katanyoo K, Sanguanrungsirikul S, Manusirivithaya S. Comparison of treatment outcomes between squamous cell carcinoma and adenocarcinoma in locally advanced cervical cancer. Gynecol Oncol. 2012;125(2):292–6.
Kasamatsu T, et al. Radical hysterectomy for FIGO stage I–IIB adenocarcinoma of the uterine cervix. Br J Cancer. 2009;100(9):1400–5.
Shinglefon HM, et al. Is there really a difference in survival of women with squamous cell carcinoma, adenocarcinoma, and adenosquamous cell carcinoma of the cervix? Cancer Cell. 1995;10(suppl 76):1948–55.
Chen JL, et al. Differential clinical characteristics, treatment response and prognosis of locally advanced adenocarcinoma/adenosquamous carcinoma and squamous cell carcinoma of cervix treated with definitive radiotherapy. Acta Obstet Gynecol Scand. 2014;93(7):661–8.
Huang YT, et al. Long-term outcome and prognostic factors for adenocarcinoma/adenosquamous carcinoma of cervix after definitive radiotherapy. Int J Radiat Oncol Biol Phys. 2011;80(2):429–36.
Wakatsuki M, et al. Clinical outcomes of carbon ion radiotherapy for locally advanced adenocarcinoma of the uterine cervix in phase 1/2 clinical trial (protocol 9704). Cancer. 2014;120(11):1663–9.
Maruyama Y, et al. A review of californium-252 neutron brachytherapy for cervical cancer. Cancer. 1991;68(6):1189–97.
Gong L, et al. Clonal status and clinicopathological observation of cervical minimal deviation adenocarcinoma. Diagn Pathol. 2010;5(1):25.
Lea JS, et al. Adenosquamous histology predicts poor outcome in low-risk stage IB1 cervical adenocarcinoma. Gynecol Oncol. 2003;91(3):558–62.
Nakano T, et al. Carbon beam therapy overcomes the radiation resistance of uterine cervical cancer originating from hypoxia. Clin Cancer Res. 2006;12(7 Pt 1):2185–90.
Lei X, et al. Californium-252 brachytherapy combined with external-beam radiotherapy for cervical cancer: long-term treatment results. Int J Radiat Oncol Biol Phys. 2011;81(5):1264–70.
Tacev T, Ptkov B, Strnad V. Californium-252 (252Cf) versus conventional gamma radiation in the brachytherapy of advanced cervical carcinoma long-term treatment results of a randomized study. Strahlenther Onkol. 2003;179(6):377–84.
Bidmead M. Dose and volume specification for reporting intracavitary therapy in gynecology. ICRU report 38. Washington: ICRU; 1985.
Maruyama Y, et al. Neutron brachytherapy is better than conventional radiotherapy in advanced cervical cancer. Lancet. 1985;1(8438):1120–2.
van Nagell JR, et al. Phase II clinical trial using californium 252 fast neutron brachytherapy, external pelvic radiation, and extra fascial hysterectomy in the treatment of bulky, barrel-shaped stage IB cervical cancer. Cancer. 1986;57(10):1918–22.
Zhang M, et al. Low-dose-rate californium-252 neutron intracavitary after loading radiotherapy combined with conformal radiotherapy for treatment of cervical cancer. Int J Radiat Oncol Biol Phys. 2012;83(3):966–71.
Maruyama Y, et al. Five-year cure of cervical cancer treated using californium-252 neutron brachytherapy. Am J Clin Oncol. 1984;5(7):487–93.
Grigsby PW, et al. Adenocarcinoma of the uterine cervix: lack of evidence for a poor prognosis. Radiother Oncol. 1988;12(4):289–96.
Niibe Y, et al. High-dose-rate intracavitary brachytherapy combined with external beam radiotherapy for stage IIIb adenocarcinoma of the uterine cervix in japan: a multi-institutional study of Japanese Society of Therapeutic Radiology and Oncology 2006–2007. Jpn J Clin Oncol. 2010;40(8):795–9.
Raju MR, et al. A heavy particle comparative study. Part III: OER and RBE. Br J Radiol. 1978;51:712–9.
van Nagell JR, et al. Phase II clinical trial using californium 252 fast neutron brachytherapy, external pelvic radiation, and extra fascial hysterectomy in the treatment of bulky, barrel-shaped stage IB cervical cancer. Cancer. 1986;10(57):1918–22.
Das D, et al. Treatment of cervical carcinoma with high-dose rate intracavitary brachytherapy: two years follow-up study. Asian Pac J Cancer Prev. 2011;12:807–10.
Buranawit K, et al. The treatment outcome of adenocarcinoma of uterine cervix at Phramongkutklao Hospital. J Med Assoc Thai. 2010;93(Suppl 6):S13–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclosures and conflict of interest statement
We declare that we have no financial disclosures and conflict of interest.
Ethical statement
Our study has been approved by the appropriate ethics committee and has been performed in accordance with the ethical standards laid down in 1964 Declaration of Helsinki and its later amendments.
Informed consent
All persons have given their informed consent prior to their inclusion in the study.
Additional information
Yanli Xiong is the first author.
Rights and permissions
About this article
Cite this article
Xiong, Y., Liu, J., Chen, S. et al. Combination of external beam radiotherapy and Californium (Cf)-252 neutron intracavity brachytherapy is more effective in control of cervical squamous cell carcinoma than that of cervical adenocarcinoma. Med Oncol 32, 231 (2015). https://doi.org/10.1007/s12032-015-0670-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-015-0670-3